Rodent Poison (Rat Bait Poisoning) in Pets: information about rodenticides with emphasis on anticoagulant rodent baits.
Rodent Poison (Rat Bait Poisoning) in Pets: information about rodenticide poisoning in animals, focusing
particularly on anti-coagulant rodenticides (e.g. warfarin, bromadiolone, brodifacoum).
Rodenticide toxicity, otherwise known as rodent poison, 'rat bait' or 'ratsak poisoning', is one of the more commonly encountered types of pet poisoning seen in most veterinary clinics around the world. This page includes everything you, as a pet owner, need to know about rodenticide poisoning in animals (dogs and cats being the focus), including: sources of rodenticide poisoning, lethal doses of particular rat and mouse poison-types, symptoms of poisoning, treatment and therapy for anti-coagulant rodenticide poisoned animals and tips and techniques you can use to prevent pets from becoming poisoned at home. The topics are discussed in the following order:
1) What is rat bait (rodenticide) poisoning? - a brief overview and summary.
2) What are the active ingredients (toxins) included in rat baits?
The above two topics include information on all rodenticide groups, including vitamin D poisons, bromethalin, zinc phosphide, thallium, strychnine, cyanide, 1080 and others. Links to pages dedicated to each of these non-anticoagulant poisons is provided in section 2.
The following sections (3-11) of this page contain information specifically targeted towards your understanding of
the anticoagulant, warfarin-related rodenticides.
3) What doses of anticoagulant rodenticides are required in order for animals to develop symptoms of poisoning?
4) How do pets become poisoned by rat bait?
4a) Poisoning at home - how animals access baits.
4b) Poisoning in the field - how animals get baits on farms, industrial areas, grains storage areas etc.
4c) Secondary poisoning - how animals become poisoned by eating poisoned vermin.
4d) Handy hints on how to determine whether someone has deliberately baited your pet.
4e) Can human anti-coagulant drugs or medications (e.g. warfarin sodium, Coumadin) poison my pet?
5) Symptoms of anti-coagulant rodenticides in animals - what they are and how they occur.
5a) An overview of the normal blood-clotting mechanisms in the animal body.
5b) What does an anti-coagulant rodenticide do to the animal's blood clotting mechanisms?
5c) Cat and dog rat poison symptoms and how long they take to appear.
6) Diagnosis of anti-coagulant rodenticide toxicity in pets:
6a) History given by owner.
6b) The vomit test.
6c) In-house testing - the Activated Clotting Time (ACT).
6d) Laboratory testing - the aPTT and PT tests.
6e) Laboratory testing - rodenticide detection.
6f) Blood smear.
6g) PIVKA testing.
6h) Treatment trial.
7 What other diseases can look like anti-coagulant rodenticide toxicity in pets?
8) Treatment: What should you do if your pet has recently eaten anti-coagulant rat bait, but has no symptoms?
8a) Making pets vomit in the vet clinic.
8b) Tips and cautions on making pets vomit at home.
8c) Gastric lavage?
8d) Enemas.
8e) Adsorbents and cathartics.
8f) Prophylactic vitamin K1 therapy.
9) Treatment of clinical anti-coagulant rodenticide toxicity:
9a) How to stop excessive bleeding at home.
9b) How to stop excessive bleeding in the vet clinic.
9c) Vitamin K1 therapy of the symptomatically poisoned pet.
9d) Intravenous fluid support.
9e) Plasma transfusions.
9f) Blood transfusions.
9g) Therapeutic draining of blood from body cavities.
9h) Tips on feeding these patients.
10) Tips on getting rid of rats and mice without pet-toxic rodenticides:
10a) Preventing mice and rats and rodents from coming to your house and staying.
10b) Natural, non-harmful mouse and rat repellants.
10c) Non-chemical, lethal mouse and rat control commercial products.
10d) Non-chemical, humane rat and mouse catching alternatives.
10e) Natrocell's Eradibait: An alternative, safe, pellet rodenticide?
11) Hints and tips for preventing rodenticide toxicity when you are using pet-toxic baits:
11a) Choice of bait.
11b) Placement of baits.
11c) Preventing secondary toxicity.
11d) Extra tips on what to do with dogs that keep on getting access to ratbait (e.g. basket muzzles, regular Vitamin K dosing).
11e) Natrocell's Eradibait: An alternative, safe pellet rodenticide?
WARNING - IN THE INTERESTS OF PROVIDING YOU WITH COMPLETE AND DETAILED INFORMATION, THIS SITE DOES CONTAIN MEDICAL AND SURGICAL IMAGES THAT MAY DISTURB SOME READERS.

1. What is rodenticide toxicity?
Rodenticide toxicity, otherwise known as rat bait poisoning or 'Ratsak' poisoning (a lay term
that has often been adopted for all rodent poisons, regardless of brand name or active ingredient, because of a once-ubiquitous rodent control product: Ratsak), is the poisoning of pets, livestock, wildlife and humans with any product that is normally used to kill rodent and lagomorph (rabbits and hares - often incorrectly termed rodents) vermin pests. Although the term typically refers to poisoning that occurs with commonly-implicated commercial anti-coagulant, coumarin-derived rodenticide products (e.g. warfarin, bromadiolone, brodifacoum); commercial Vitamin D analogue products (e.g. cholecalciferol), commercial metal phosphide products (e.g. zinc phosphide) and commercial bromethalin containing products, any poison used to kill mice, rats, rabbits, hares and large rodents (squirrels etc.) that was inadvertently (or deliberately) fed to pets, livestock, non-target-wildlife or humans would be termed a rodenticide toxicity. Arsenic, strychnine, 1080, cyanide, thallium and a whole host of other commercial, non-commercial or homemade rodent-killing products could be implicated in rodenticide toxicity of non-target
pet, livestock and wildlife animals.
Most cases of rodenticide toxicity occur when pets and livestock directly consume grain-based commercial pellets or wax blocks containing rodenticide toxins. These commercial poison products
are normally accessed by pets after being placed in the pet's environment by an owner, however, poisoning
of pets may also occur as a result of malicious neighborhood baiting or as a result of rodents and birds moving baits around or as a result of a pet finding a previously-unknown
stash of bait (e.g. bait left in a garden shed by a previous house tenant). Secondary poisoning
is also possible with some products (see 4c): carnivorous pets and omnivorous livestock
(e.g. pigs) become poisoned when they consume the corpses of dead rats and rodents that contain poison residues in their bodies.
The most well-known symptoms of rodenticide toxicity in pets are those that pertain to the anti-coagulant effects of the coumarin-derived rodenticides (see section 2 for a list of anti-coagulant rodenticide names and active ingredients). Pets that ingest
these baits develop an inability to clot their blood and this results in a wide range of symptoms including: wounds that won't stop bleeding, injection sites that won't stop bleeding, large bruises on the body or gums, acute swelling of one or more joints, swelling of regions of skin (big, bruised lumps called hematomas under the skin), sudden swelling of the abdomen (if the animal haemorrhages
into the belly cavity), difficulty breathing (if the haemorrhage occurs within
the chest cavity or lungs), coughing up of blood, vomiting of blood, defecation of blood, pale
to white gum colour and, in severe cases, collapse of the animal and signs of shock. Left untreated, severe, ongoing bleeding will result in the death of the animal (this
is how the mice and rats that eat the bait die too).
The symptoms of rodenticide toxicity that occur with many of the other less-common, less-well-known
mice and rat control products are hugely variable. Symptoms seen are very much
dependant on the product and active ingredient ingested. For example, Vitamin D analogue
(cholecalciferol) poisoning typically causes high blood calcium levels and mineralization
of the animal's body tissues with eventual onset of acute renal failure. Symptoms seen with this poison are often non-specific and initially very subtle and include: depression, weakness, inappetence or anorexia, vomiting and constipation, eventually progressing to vomiting of blood, passing of black feces, lack of urination, heart arrhythmias and death. Different again from the anticoagulant
rodenticides and Vitamin D analogues, there are yet other rodent poison ingredients (e.g. bromethalin, strychnine and 1080) that act by attacking the animal's nervous system. These
typically produce symptoms of severe seizuring, rigor (a stiff body) and pronounced neurological signs with death generally being caused by severe brain damage and/or disruption to the
animal's ability to coordinate its chest muscle movements for normal breathing function.

2) What are the active ingredients of rat bait?
There are many kinds of rodenticides available and most of these are as potentially toxic to pets and livestock animals as they are to the vermin they are intended for. Commonly encountered rodenticides include the anticoagulant rodenticides, Vitamin D analogue
rodenticides (cholecalciferol), metal phosphides (e.g. zinc phosphide), bromethalin and strychnine. All of them are still being formulated into commercial rodenticide products
that may be readily available to the public and to industry. Other rodenticides such
as red squill, cyanide, thallium, arsenic, 1080 (sodium monofluoroacetate), pyriminil, phosphorus, norbromide and barium may still occasionally be encountered in pet poisonings, but are
much less common. Note that this may, of course, depend on the country and region: some
poisons that are considered 'rare' in Australia may have widespread use in other countries.
2a) The anti-coagulant rat poisons:
The anti-coagulant rat and mice poisons contain chemicals that have all been derived and engineered from a natural anti-coagulant compound called coumarin or
dicoumarol, a benzopyrone compound found in the tissues of certain plants, including mouldy sweet
clover, trees of the Cassia family (e.g. cinnamon), woodruff and tonka beans.
The toxin was first discovered when cattle were found to show increased bleeding tendencies following
the ingestion of spoiled sweet clover.
Over time, many coumarin-derived chemicals, far superior in their rodent-killing abilities
than the coumarin parent compound, have been invented by commercial chemical laboratories and placed into grain-based pellets and wax-blocks for the purpose of killing rodent vermin. These anticoagulant rodenticide compounds can be divided into two groups: the first-generation or multiple-feed rodenticides and the second-generation or single-feed rat baits (also termed Super Warfarin compounds).
First-generation or multiple-feed rodenticides:
 The first-generation anticoagulant compounds were the first of the coumarin-derived chemicals invented for controlling rodent pests. Less potent than the more recent, second-generation anti-coagulant poisons, these first-generation compounds require a mouse or rat to feed on them over a course of several
days, gradually accumulating a lethal dose of poison in their tissues, before they
will cause death in the pest animal. Although a single, large feed of a first-generation bait will sometimes poison a cat or dog, first-generation rodent poisons do not persist as long in the dog or cat's tissues and blood (i.e. they have a shorter biological half-life)
and, thus, much shorter courses of antidote medication (Vitamin K1) are required to treat these patients. Additionally, because the mouse or rat often has to feed for several days in order to obtain a dose of poison that is lethal to it (i.e. a cumulative dose that is usually too small to be lethal to a dog or cat predator), the chances of secondary poisoning, whereby the dog or cat becomes
poisoned by eating a dead or dying vermin animal, are very low with these compounds.
The first-generation anticoagulant compounds were the first of the coumarin-derived chemicals invented for controlling rodent pests. Less potent than the more recent, second-generation anti-coagulant poisons, these first-generation compounds require a mouse or rat to feed on them over a course of several
days, gradually accumulating a lethal dose of poison in their tissues, before they
will cause death in the pest animal. Although a single, large feed of a first-generation bait will sometimes poison a cat or dog, first-generation rodent poisons do not persist as long in the dog or cat's tissues and blood (i.e. they have a shorter biological half-life)
and, thus, much shorter courses of antidote medication (Vitamin K1) are required to treat these patients. Additionally, because the mouse or rat often has to feed for several days in order to obtain a dose of poison that is lethal to it (i.e. a cumulative dose that is usually too small to be lethal to a dog or cat predator), the chances of secondary poisoning, whereby the dog or cat becomes
poisoned by eating a dead or dying vermin animal, are very low with these compounds.
Common first-generation or multiple-feed rodenticide active ingredients:
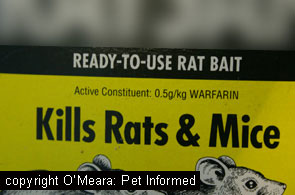
Warfarin - trade names include: Warfarin, Ratsak, Kaput products, Adios Mouse Killer, Adios Mole Killer.
Coumatetralyl - trade names include: Racumin 8, Racumin products, Endox products.
Dicoumarol - the original anticoagulant compound found in mouldy sweet clover.
Pindone - trade names include Pival, a once-commonly used rabbit poison in Australia, and Rabbait.
Coumafuryl - trade names include Fumarin.
Coumachlor - trade names include Famarin.
Valone
Isovaleryl
Second-generation or single-feed rodenticide (Super Warfarins) active ingredients:
 The second generation anticoagulant rodenticide compounds were the most recent coumarin-derived chemicals invented for use in killing rodent pests. They were developed because, in certain locations where widespread, intensive first-generation rodenticide use was occurring (e.g. Europe, USA),
many of the rats and mice were becoming resistant to the first-generation poisons, leading to
a failure of effective rodent control in these regions. Highly potent, the second-generation anti-coagulant rat poisons are easily able to kill a mouse or a rat after only a single feed of bait. A single feed of a second-generation rodent bait will, likewise, poison a cat or dog and, because these chemicals persist in the dog or cat's tissues (especially the animal's liver and fat) for a long time, long courses of antidote treatment (Vitamin K1) are required to effectively treat animals that have been inadvertently poisoned (around 5-6 weeks of treatment). Additionally, because the mouse or rat only has to feed once to obtain a lethal dose of poison (a single dose that may well exceed the minimum amount that would
have been needed to kill it) the chances of secondary poisoning of carnivorous pets are much higher with these compounds. In a single feed, a mouse or rat may be capable of consuming and storing in its tissues a dose of poison that is lethal for a dog or cat or wild animal predator.
The second generation anticoagulant rodenticide compounds were the most recent coumarin-derived chemicals invented for use in killing rodent pests. They were developed because, in certain locations where widespread, intensive first-generation rodenticide use was occurring (e.g. Europe, USA),
many of the rats and mice were becoming resistant to the first-generation poisons, leading to
a failure of effective rodent control in these regions. Highly potent, the second-generation anti-coagulant rat poisons are easily able to kill a mouse or a rat after only a single feed of bait. A single feed of a second-generation rodent bait will, likewise, poison a cat or dog and, because these chemicals persist in the dog or cat's tissues (especially the animal's liver and fat) for a long time, long courses of antidote treatment (Vitamin K1) are required to effectively treat animals that have been inadvertently poisoned (around 5-6 weeks of treatment). Additionally, because the mouse or rat only has to feed once to obtain a lethal dose of poison (a single dose that may well exceed the minimum amount that would
have been needed to kill it) the chances of secondary poisoning of carnivorous pets are much higher with these compounds. In a single feed, a mouse or rat may be capable of consuming and storing in its tissues a dose of poison that is lethal for a dog or cat or wild animal predator.
Second-generation or single-feed rodenticide (superwarfarin) active ingredients:
Brodifacoum - trade names include Final products, Talon-G products, WeatherBlok XT Bait Rodenticide, Havoc products, Klerat, Ratak Plus, Volid.
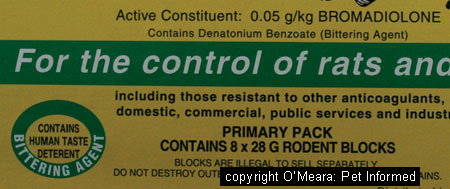
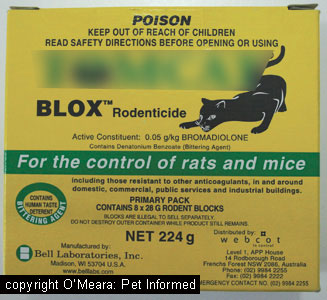
Bromadiolone - trade names include Contrac products, MOUSEOFF products, Maki products, Bromakil, Bromone and Tomcat products.
Flocoumafen - trade names include Storm products.
Difethialone - trade names include Generation products, Generation BlueMax products.
Diphenacoum or difenacoum - trade names include Ratak, Frunax-DS.
Diphacinone - trade names include Liqua-Tox II, Kaput D products, Ditrac products, PCQ Rodenticide-CA, Bait Block, RCO Mole and Gopher Patrol Bait, RCO Squirrel Patrol Bait, Adios Gopher Killer, Ramik products, Pestoff
Ferret Paste, RatAbate, Diphacin and many others.
Chlorophacinone - trade names include A-C Formula 90, Rozol products, Ground Force Paraffinized pellets Rodenticide, RCO Mole Patrol Bait, Drat, Topitox, Raviac, Ramucide, Ratomet and others.
Author's note: Depending on what you read, diphacinone and chlorophacinone are often classified as either first generation products or second generation products. Even government drug classification
agencies and drug companies seem to have great difficulty placing them in one group or the
other. The reality is that these two compounds seem to be somewhere in the middle. They are possibly up to 4x more toxic than the first generation compounds and, like
the second generation compounds, they have a much longer biologic half life than the first generation
products (they persist in the animal's tissues for longer). Unlike the second generation
compounds, however, they do not seem to have the long-lasting environmental residues
that the first generation ones do (note - chlorophacinone does have some residue accumulation
in wild animals); they can kill individual rodents in a single feed, but
often require more than one feeding to control a large rodent population (e.g. multiple feed qualities)
and they do not last quite as long in animal tissues as the truly second generation ones: brodifacoum and bromadiolone.
I have elected to group these two compounds into the second generation group because, from a veterinary viewpoint, this is where they seem to fit best from a treatment perspective. Like the second generation compounds, diphacinone and chlorophacinone have much longer
biologic half lives than the first generation compounds do. For example, diphacinone has
a plasma half-life of 5 days, similar to the half life of bromadiolone (6 days), whereas
the plasma half life of first-generation warfarin is only around 15 hours. Consequently, much longer courses of vitamin K1 therapy (up to 4-6 weeks) are required in order
to effectively treat dogs and cats that have eaten diphacinone or chlorophacinone
than are needed to treat animals that have consumed first generation rodenticides (only 1-2 weeks).
2b) The cholecalciferol (vitamin D analogue) rat baits:
Several rodenticide products have been created that contain derivatives of cholecalciferol (Vitamin D) and which work on the toxicological principles of acute, lethal vitamin
D overdose. Normal amounts of vitamin D are crucial to an animal's survival: the vitamin is required in order for an animal to regulate the levels of calcium and phosphorus
in its bloodstream and bones. Consumed to excess, however, Vitamin D rapidly becomes a lethal poison. Vitamin D, consumed to excess, increases massively the levels of calcium absorbed from the animal's
food and into its bloodstream. In excess, Vitamin D also promotes the rapid reabsorption of
calcium from an animal's bones and into its bloodstream. The calcium in the animal's blood rises
to abnormally high levels, resulting in many effects on the body including: nervous system depression, muscle
weakness, sluggish reflexes, disorders of heart muscle contractility and heart rhythm and reduced intestinal motility (e.g. constipation, abdominal pains, reduced appetite). Levels of blood calcium exceeding 17mg/dl result in calcium phosphate crystals precipitating
throughout the animal's bodily organs (e.g. the renal tubules, lungs, linings of blood vessels)
and this effect, taken to excess, results in the failure of many organs, especially
the kidneys. Death occurs within 2-5 days.
Vitamin D analogue (cholecalciferol) baits are highly lethal to mice and rats. They are
also extremely toxic to domestic pets who inadvertently consume them. Although there is
a theoretical antidote to the poison's effects (Calcitonin - a drug that works by opposing the mechanisms that increase calcium levels in the blood), the drug is only effective
at preventing calcium level increases and tissue mineralisation and organ damage if it is given
early (i.e. if the owner knows the animal has eaten the bait and seeks early vet attention),
before the onset of severe clinical signs. By the time the animal shows obvious signs of poisoning
(e.g. vomiting, renal failure, organ failure), it may already be too late to save that animal. This is unlike the situation seen with the anti-coagulant rodenticides: with anticoagulant
rodenticides, even if symptoms of anticoagulant poisoning are seen, so long as the bleeding is not too severe or located in an unfavorable part of the body, such as the brain, animals that have eaten anti-coagulant rodenticides can often still be saved. Vitamin D analogue rodenticides
are considered so lethal to pets and other animals that they have been discontinued for sale in many countries, including Australia. Old packets may still be lying around, however, even in countries where the product is now banned, and so it pays to aware of them and what they can do to pets.
The risk of secondary poisoning is very low with cholecalciferol and, thus, the risk to wild predators and domestic carnivores, should they eat vermin killed with these products, is low. The chemical does not tend to accumulate in the tissues of pest animals or last in soil
and waterways and, consequently, environmental contamination with toxic residues is minimised.
This is one of the reasons why the New Zealand forestry department still uses such
products in the control of pest vermin and possums in its wildlife reserves.
Vitamin D analogue rodenticides - active ingredients:
Cholecalciferol - trade names include Quintox products, Feracol, Rampage, Ortho Rat-B-Gone, Ortho Mouse-B-Gone.
The vitamin D rodenticides will not be discussed much further on this anticoagulant rodenticide focussed page. This poison has its own special page:
For everything on Cholecalciferol/Vitamin D rodent poisons, click here.
2c) The metal phosphide rat baits (zinc phosphide, magnesium phosphide, aluminium phosphide):
The metal phosphide baits were invented, for the most part, to protect commercial grain stores (mostly indoors) and the edible produce of farming ventures and food-industry food producers from the ravages of rats, mice and larger rodents, such as the vole and gopher. These baits were designed for the purposes of large scale rodent control in commercial facilities
and wildlife management (e.g. wildlife reserves) situations and have tended to replace
many of the more dangerous, human-risk compounds that were commonly in use in such facilities
prior to their invention (e.g. arsenic, cyanide and strychnine). These baits are not generally intended for domestic house-hold use.
Following consumption by an animal, the desiccated metal phosphide within the bait reacts with
acid and moisture in the animal's stomach; a chemical reaction which releases a poisonous
gas called phosphine gas. This gas interferes with the oxidative phosphorylation process (oxidative phosphorylation, is a series/cycle of chemical reactions that occurs within special organs called mitochondria, located within an animal's cells, so that the cell can produce the ATP energy it needs for normal cellular function) of the cells
that it comes into contact with, in particular the intestinal cells and cells of the lungs. This renders these cells unable to create a compound called ATP (adenosine triphosphate), the
main energy unit of the cell needed for normal cell function. Unable to produce energy
to meet their normal cell-function needs, the animal's cells begin to die rapidly. The animal (rodent or domestic pet) suffers severe depression, weakness, gastrointestinal distress (inappetence, vomiting, vomiting blood, diarrhoea, abdominal pain), respiratory distress (the animal's lung cells become damaged and lose their integrity, allowing fluid from the blood vessels within the lungs to leak into the airways, effectively drowning the animal), tremors, convulsions, collapse, 'fainting' or syncope. coma and death. Damage to the heart muscle and severe heart arrhythmias may also be seen. In dogs, an initial
hyperexcitability may be seen, whereby the animal seems to 'go crazy', racing around madly and
screaming (howling and yelping crazily) and biting or snapping before progressing
to severe tremors and seizures and rapid death. A similar 'mad dog' episode is seen with 1080
poisoning too.
There is no known antidote to metal phosphide poisoning and treatment of the poison
is by decontamination (if caught early) and supportive care only. The mortality, particularly
for pets that were not witnessed to eat the bait (thereby delaying therapy), would be expected
to be high.
Metal phosphide rodenticides - active ingredients:
Zinc Phosphide (most common) - trade names include ZP rodent products, RodentRid, RCO/R-M Vole Bait, Prozac.
Magnesium Phosphide.
Aluminium Phosphide.
The metal phosphide rodenticides will not be discussed much further on this anti-coagulant rodenticide page. These poisons have their own special page:
For everything on metal phosphide (e.g. zinc phosphide)
rodent poisons, click here.
2d) Rat baits that act upon the central nervous system:
A wide variety of rodent poisons are available that act upon the central nervous system (brain)
and/or peripheral nervous system (nerves directly supplying the limbs and organs) of
rodents and other animals, producing symptoms of severe neurological disorder (e.g. tremors, seizures, salivation, wobbliness) and death. Although some of these compounds can occasionally be found
in routine, household-use rodent poisons (e.g. bromethalin "Fastrac" pellets), most of them tend to be highly toxic, highly restricted (difficult for the general public to access) and reserved for use in vermin control programmes within farmland and wildlife reserves (places where highly-effective, low-residue, low environmental accumulation characteristics are highly important). These products are most commonly encountered in mole, vole, possum (New Zealand), mustelid (feral stoat and ferret), fox, feral canine and feline
and gopher control products. Although nowhere near as common as with the aforementioned rodenticide products (sections 2a-2c), domestic pet poisoning with these neurological system toxins does sometimes occur, making them worth a mention here.
Bromethalin - similar to the effect of the metal phosphides, bromethalin is thought to deactivate oxidative phosphorylation and, thereby, impede the production of ATP (adenosine triphosphate) energy in the brain and liver cells of the animal. These brain and liver cells start to swell with fluid
as a result of subsequent inactivity of ATP-dependent water removal mechanisms
within the liver and brain cells (ATP energy is needed to operate a 'gateway' that is responsible for
controlling sodium, potassium and water levels within a cell). In the brain, this fluid swelling is termed cerebral oedema (also spelled edema). The swollen brain cells fail to work properly and eventually start to die off, resulting in symptoms of severe neurological dysfunction: seizuring, hyperexcitability, muscle
tremors, paddling, hyperthermia (excessive bodyheat), coma and death. Sublethal doses may only
produce signs of transient wobbliness and hind leg incoordination, without the seizures and brain signs. Depending on the dose of poison consumed and how long the symptoms of severe neurological dysfunction have been present prior to the onset of
veterinary attention, the prognosis for a poisoned pet may be guarded to poor. There is no specific antidote to this toxin.
Strychnine (Strychnos nux vomica) - illegal or highly-restricted in Australia and many other countries because of its high potential for human poisoning and misuse, strychnine can still occasionally be encountered in several farm-use rodent eradication products.
In particular, strychnine seems to be a favored choice for certain gopher eradication products. Domestic pets can become poisoned if they consume unthoughtfully placed commercial products or
food items deliberately laced with poison (strychnine used to be a common poison used in the malicious baiting of 'nuisance' neighborhood pets). The poison acts upon the peripheral nerves supplying the animal's limb and respiratory muscles. Strychnine
works by inhibiting the action of glycine, a chemical neurotransmitter (chemical produced
by a nerve to regulate the activity of that same nerve (feedback mechanism) or another nearby nerve) which normally acts to regulate the intensity of the nerve signals supplying the animal's muscles in order that they do not over-stimulate the animal's muscles during normal muscle movement and respiratory activities. By preventing this natural glycine-mediated neurological feedback mechanism, strychnine makes it possible for nerves supplying the animal's muscles to severely overstimulate these muscles, resulting in uncontrolled muscle excitation, severe muscle and limb rigidity, severe tremors, hyperthermia and death from a failure of relaxation of the muscles of respiration (breathing). Treatment is supportive and there is no specific antidote.
Cyanide - severely restricted and often illegal in many countries (e.g. Australia) because of its high potential for human toxicosis and misuse, cyanide can still occasionally be encountered in farm-use and wildlife reserve vermin eradication projects. For example, because cyanide does not tend to leave much behind in the way of environmental contamination and toxic residues, cyanide products are still sometimes used in New Zealand for the control of rats and possums in its wildlife reserves. The cyanide absorbed into the body works by binding up copper and iron ions within the
mitochondria of the animal's cells. The mitochondria are 'organelles' (small organs) contained within the body of the cell whose role it is to coordinate oxidative phosphorylation
and energy production within the cell (oxidative phosphorylation occurs within the
body of the mitochondria). By binding up iron and copper ions within the mitochondria, the cyanide effectively stops the oxidative phosphorylation pathway, which relies on
the iron and copper for electron transport within the pathway, resulting in an inability
of the cell to use oxygen in order to produce energy (ATP) for cellular processes. This effectively starves the bodily organs, especially the brain and heart, of vital oxygen use and energy.
The animal dies rapidly from seizures and respiratory distress. Sudden death with no obvious
signs apparent to the owner may also be noted - it can be very rapid.
Sodium monofluoroacetate or fluoroacetate (Compound 1080) - highly restricted, but not uncommon in Australia and many other countries, 1080 is widely used in the control of foxes, rabbits, rodents and various feral or wild carnivorous pests (e.g. dogs, coyotes).
A lethal poison, 1080 disrupts the Kreb's cycle or Citric Acid cycle: a cyclic series of
chemical reactions that take place in the mitochondrion, the purpose of which is to produce
hydrogen atoms essential to the functioning of the energy-producing oxidative phosphorylation
process mentioned previously. Without the Citric Acid Cycle, oxidative phosphorylation can
not occur and the body cells can not generate energy for cellular processes. Starved
of energy, 1080-affected cells, especially the high-energy-needing cells of the brain
and heart, start to die. This results in severe neurological signs in dogs: 'mad-dog' running around
and screaming, hyperexcitability, convulsions, overheating and rapid death and rigor mortis. No canine species: rodents, rabbits, horses and ruminants tend to show cardiac signs more than
neurological signs with weakness, staggering, arrhythmias and sudden death more typical. Cats and pigs tend to show a combination of both neurological and cardiac signs. There is
no specific antidote to 1080 poisoning. The mortality is high.
Central nervous system rodenticides - active ingredients:
Bromethalin - trade names include Fastrac products, Talpirid Mole Bait, Top Gun products, Trounce, Vengeance, Hot Shot, Sudden Death Mouse Killer, Assault.
Strychnine - trade names include Gopher Bait 50, RCO Omega Gopher Grain Bait.
Cyanide - trade names include Feratox.
Fluoroacetate or 1080.
The central nervous system acting rodenticides will not be discussed much further on this anti-coagulant rodenticide page. These poisons have their its own special pages:
For everything on Bromethalin rodent poisons, click here.
For everything on Strychnine poisoning, click here.
For everything on Cyanide poisoning, click here.
For everything on 1080 poisoning, click here.
2e) Other, less common rodenticides:
Alpha-Naphthyl Thiourea (ANTU) - prior to the development of highly-effective
rodenticides such as warfarin and its anticoagulant relatives, ANTU used to be a common rodenticide used in the eradication of rats from rubbish dumps and large, commercial
facilities. The poison causes the blood vessel walls of the capillaries within the lung
tissues to become 'leaky', such that watery fluid from the bloodstream is able to
leak through the walls of the blood vessels and into the air spaces of the lungs. This is termed pulmonary oedema of non-cardiogenic origin (i.e. fluid in the lungs
that is not being caused by congestive heart failure). The animal is unable to
get oxygen into its lungs because of the fluid in the lungs and it dies from a lack of
oxygen (it effectively 'drowns'). The clinical signs relate to this drowning - blue
mucous membrane colour, difficulty breathing, coughing up of frothy fluid and death.
Arsenic (arsenic trioxide) - arsenic as a poison for pets and livestock can be found
in a wide range of commercial preparations (old paint, arsenic treated wood products, insecticides and old livestock dips and medicants), not just in arsenic-based rodenticides,
and residues of arsenic may persist in soil and waterways for many years after use of these
types of products has been discontinued (arsenic tends to persist in the environment).
Arsenic is a highly-cumulative, toxic substance that can persist in the environment and affect animals and humans adversely for years to come and, for these
reasons, as a rodenticide, arsenic has been pretty much superseded by a huge variety of better
products. Arsenic has a range of effects within the body, including adverse effects on
the Citric Acid Cycle (see 1080) and on oxidative phosphorylation as well as adverse effects
on the roles of many oxidative enzymes and other enzymes found within cells that are required for
normal cellular function. In particular, arsenic tends to favor the cells lining the
blood vessels of the intestinal tract, kidneys and liver, leading to severe intestinal
damage, liver damage and renal failure as these blood vessels (as well as blood vessels
in other organs) become severely impaired. Animals that ingest a lethal dose can die very suddenly with minimal signs (abdominal pain and collapse) or they may linger for several days with severe intestinal signs (vomiting, inappetence, blood in the vomit
and faeces, projectile, watery diarrhea), tremors, staggering, hind leg paralysis, hypothermia, acute renal failure (e.g. no urine production) and sometimes convulsions.
Thallium - thallium is a metal-type poison, not all that dissimilar to arsenic in its actions,
that used to be widely available to the public for the control of rodents in properties and business facilities. Toxicity to pets and livestock, referred to as
thallotoxicosis, used to be commonplace. The restriction of this substance (it is now
under strict government control and regulation) has greatly reduced the incidence of
inadvertent thallium poisoning of pets, however, thallium toxicity can still sometimes
be encountered when pets access old, long-forgotten stashes of the substance. The
clinical effects typically resemble arsenic in many ways: animals that ingest a lethal dose can die very suddenly with minimal signs (abdominal pain and collapse) or they may linger for several days with severe intestinal signs (vomiting, inappetence, blood in the vomit
and faeces, projectile, watery diarrhea), tremors, staggering, paralysis, hypothermia, breathing difficulties and sometimes convulsions. Animals that eat a sublethal dose
will experience a longer duration (weeks) of intestinal signs and neurological signs
(tremors, convulsions, paralysis) and may develop severe skin signs (red skin, pustules
on the skin that start at ears and nose and progress bodywide, drying and cracking
and infection of the skin and loss of the hair coat) and respiratory signs (pneumonia
and bronchitis).


3. What doses of anticoagulant rodenticides are required in order for animals to develop symptoms of poisoning?
This section comes with an important disclaimer:
The following information on anticoagulant rodenticide toxic dosages and LD50s in pets and livestock have been referenced from a wide range of respectable veterinary and non-veterinary sources, including various veterinary textbooks, pharmacological textbooks and the website of the World Health Organisation. Although every attempt has been made to ensure the accuracy of these dosages in order to provide you, the owner, with some idea of what your pet might need to consume in order to be poisoned with these chemicals, I can not vouch for what the outcome might be in every pet or poison situation that might be encountered.
There are several reasons for this:
1) Individual commercially-available rodent poison formulations are all different.
Individual drug companies blend their rodenticide products with all manner of additives
these days: additives designed to increase the digestibility of the product
and enhance the absorption of the active poison ingredient/s into the rodent animal's body and tissues. This individual variation in product digestibility and absorption
can make it difficult to guess exactly what amount or dosage of rodenticide product is likely to be toxic to a domestic pet. For example, one product containing warfarin may be more highly digestible and better absorbed than another product containing the exact same amount of warfarin per gram of product, thereby making the first product potentially more lethal at much lower doses than the second product.
2) Individual animals absorb and metabolise drugs differently to others.
Some animals may become poisoned by significantly lower doses of a drug or toxin
than other animals due to variations in their breed or species genetics; variations in
their intestinal absorption abilities; differences in their blood protein levels or
body fat levels (these variations affect the poison's distribution and storage within the body)
and variations in their liver and kidney functions. For example, animals with intestinal
malabsorption diseases (e.g. inflammatory bowel disease) may not absorb as much of a
poison as a healthy animal and, thus, tolerate larger poison doses. For example, animals with renal (kidney) disease or hepatic (liver) dysfunction may have a reduced ability to break down or excrete toxins from their bodies and, therefore, these animals
may suffer from toxic side effects at much lower doses than normal animals would.
Even the amount of food in an animal's stomach when it ate the poison may be enough to alter the amount of poison that is absorbed into the animal's system and, therefore,
affect whether signs of toxicity manifest.
3) You, as the owner, may not be able to determine 100% just how much of a poison your pet has actually eaten.
In my experience as an emergency clinic veterinarian, many owners are never 100% sure just how
much bait was actually present within the box of rat bait or snail bait pellets before their pet
got into it. There can be a huge difference in toxic outcome between the consumption of
3/4 of a box or "just a few pellets".
4) Aged baits may not be as toxic as newly purchased baits.
Consumption of large amounts of an ancient, long-forgotten bait supply may not result
in the severe toxic side effects that would be expected of such a dosage, due to
the advanced disintegration of the bait ingredients over time. Newly purchased baits, on the other hand, would be expected to be fully operational and at maximum toxicity at the time of purchase.
5) The toxicity of various poisons can be altered by the
presence of other drugs, medications and hormones within the individual animal's system.
This is particularly true of the anticoagulant rodenticides. There is a wide range
of medications and drugs that can alter the metabolism of anticoagulant rodenticide poisons, thereby increasing or decreasing their toxicity for a certain poison dosage. For example, phenobarbitone drugs enhance the liver's ability to break down anticoagulant rodenticides, thereby reducing their toxicity, by increasing the activity of certain liver enzymes. Compounds such as phenylbutazone and other non-steroidal anti-inflammatory drugs may increase
the toxicity of rodenticides by competing with them for spaces on blood transportation proteins
(rodenticide compounds pushed off these proteins are free to interact with the liver cells and
produce signs of toxicity). Even seemingly-innocuous 'natural' herbal remedies, used commonly
by human patients, can play a role. Plants such as passionflower, juniper and verbena contain high levels of vitamin K1 and can lessen the effects of warfarin. Other plants
such as japonicum, pawpaw, ginseng, garlic, ginger, red clover and horse chestnut may, alternatively, potentiate the toxicity of the rodenticide anticoagulant drugs.
These dose rates have been provided to you for general information purposes only.
As mentioned above, different pets react to different levels of poison ingestion differently
and no real guarantee can ever be given as to which doses will and will not be safe in all
pets. The best advice I can give you on the matter of toxic drug doses in pets is to always play it safe and visit a vet (or at least talk to a local vet on the phone and get advice).
Always assume that your pet has eaten more than you think.
Always call your local veterinarian or emergency center for advice if you suspect any poison ingestion and always assume that your pet could be one of the ones that is more susceptible to the effects of poisoning at lower doses. You are far better
to take the suspect-poisoned animal to a vet and have it declared 'all-clear' than to
leave it untreated for want of a couple of hundred dollars and have it die from what
seemed to be a very low dose of poison. This is true of all suspect poison ingestions, not just rodenticides.
Toxic doses of anticoagulant rodenticides:
Warfarin:
rats and mice - a single dose of 50-150mg/kg or a minimum of 1mg/kg/day for 6 days or more. LD50 Norway rat 58mg/kg.
ruminants - 200mg/kg/day for 12 days or more.
dog LD50 - 20-50mg/kg or a minimum of 1-5mg/kg/day for 5-15 days.
cat LD50 - 5-50mg/kg or a minimum of 1-5mg/kg/day for 5-15 days.
pigs LD50 - 1-5mg/kg or a minimum of 0.05-0.4mg/kg/day for 7 days.
rabbit LD50 - 800mg/kg
fowl and horses are highly resistant, but can be poisoned by high doses.
Diphacinone:
rat LD50 - 1.5 mg/kg.
mouse LD50 - 340mg/kg.
rabbit LD50 - 35mg/kg.
dog LD50 - 3-7.5mg/kg.
cat LD50 - 15mg/kg.
pig LD50 - 150mg/kg.
Brodifacoum:
rat LD50 - 0.27mg/kg
mouse LD50 - 0.4mg/kg
rabbit LD50 - 0.29mg/kg
pig LD50 - 0.5-2mg/kg
dog LD50 0.25-3.5mg/kg.
cat LD50 - 25mg/kg
chicken LD50 - 10-100mg/kg
Bromadiolone:
rat LD50 1.25mg/kg
mouse LD50 - 1.75mg/kg
rabbit LD50 - 1mg/kg
dog LD50 - 10mg/kg
cat LD50 - 25mg/kg
Difenacoum:
rat LD50 - 1.8mg/kg
mouse LD50 - 0.8mg/kg
rabbit LD50 - 2mg/kg
pig LD50 - 80-100mg/kg.
dog LD50 - 50mg/kg
cat LD50 - 100mg/kg
chicken LD50 - 50mg/kg
sheep LD50 - 100mg/kg
Flocoumafen:
rabbit LD50 - 0.7mg/kg
pig LD50 - 60mg/kg.
dog LD50 - 0.075-0.25mg/kg
cat LD50 - >10mg/kg
sheep LD50 - >5mg/kg
Difethialone:
rabbit LD50 - 0.75mg/kg
pig LD50 - 2-3mg/kg.
dog LD50 - 5mg/kg
cat LD50 - >16mg/kg
What is LD50 and how do we use it?
The LD50 is a measurement of a chemical's toxicity based upon tests on animals
that are performed in a laboratory setting. The LD50 is the dose of a poison required
to kill at least 50% of animal test subjects. Thankfully, LD50 testing on animals
is going out of fashion as newer ways of testing poison and medication efficacy
are developed. The LD50 data for rodenticides is available because most of the rodenticides
were invented and tested decades ago, well before LD50 testing became unpopular.
As a general rule, the minimum toxic dose required to poison an animal is said to
be approximately 10% of the LD50 dosage. So, for example, a dose of 10mg/kg
is the minimum dose of difenacoum that would be needed to poison a sheep (this
is 10% of 100mg/kg). This dose will not kill all sheep (remember, 50% of the population
tested die if 100mg/kg is given), but it is enough to kill susceptible sheep.
As
mentioned before, as an owner it is always best to assume that your pet is one of the susceptible
ones when it comes to poisoning. The 10% of LD50 rule gives you a handy estimate of what the minimum doses of a poison might be for a susceptible pet and gives you somewhere
to start. I would always advise ringing a vet for information, however, with any case of
suspected poisoning, even if the dose ingested seems to be very low by this calculation.
Author's note: poison concentrations in commercial products are often stated in
ppm (parts per million) or as a percentage (e.g. diphacinone 0.005%).
1 part per million of a chemical = 1mg/kg = 0.0001%.
Drugs and chemicals that can potentiate (increase) the toxicity of the anticoagulant rodenticides:
Acetaminophen (e.g. paracetamol, panadol).
Non-steroidal anti-inflammatories (e.g. phenylbutazone, ketoprofen, aspirin, ibuprofen, meloxicam, carprofen).
Corticosteroids (e.g. prednisolone, dexamethasone, triamcinolone).
Certain antibiotics (e.g. trimethoprim-sulfonamides, chloramphenicol, neomycin, metronidazole, erythromycin, clarithromycin, tetracyclines, ciprofloxacin).
Certain antifungals (e.g. fluconazole, itraconazole).
Phenytoin (an epileptic medication).
Cimetidine.
Omeprazole.
Amiodarone.
Quinidine.
Hormones released during stress - ACTH, corticosteroids (e.g. cortisol).
Thyroxine.
Certain plant extracts - genoderma, ginkgo, japonicum, pawpaw, papain, dong quai, ginseng, garlic, ginger, red clover, devil's claw, horse chestnut.
Please note that this is not an exhaustive, all-inclusive list. There are a huge range of
chemicals and hormones and drugs that can interfere with the toxicity of these rodenticides.
Drugs and chemicals that can reduce the toxicity of the anticoagulant rodenticides:
Barbiturates (e.g. thiopentone, phenobarbitone, pentobarbitone).
Phenytoin.
Rifampin.
Primidone.
Griseofulvin.
Azathioprine.
Certain plant extracts - passionflower, juniper, St John's Wort and verbena.
Please note that this is not an exhaustive, all-inclusive list. There are a huge range of
chemicals and hormones and drugs that can interfere with the toxicity of these rodenticides.

4) How do pets become poisoned by rat bait?
4a) Poisoning in the home.
Most of the cases of rodenticide poisoning that I, as a veterinarian, have encountered have occurred
within the owner's own home, yard or shed environment. Of these, the vast majority of the baits were put out by the owners themselves, with the owners either oblivious to the risk posed by the baits to their pet or, more commonly, with the owners fully
aware of the risks, but "absolutely certain" that their pet couldn't possibly get to the baits. "I can't think how he would have gotten it out from the top of the cupboard."
Never underestimate the ability of a pet to get into ratbait or snail bait or any other tasty
bait. Baits used to kill rats and other vermin contain grains and rich smells (e.g. apple odour) and are designed to be maximally attractive and palatable to the rodents that they are intended for. Unfortunately, they are also often highly attractive
to dogs and cats and other pets as well (dogs more so than cats - cats tend to be more finicky and
suspicious of new food items). I have seen dogs scale cupboards and push over shelves
and leap to immense, unexpected heights to access such tasty delights as ratsak.
As long as there is rat bait in your house, yard or shed, no matter where it is placed, you need to be prepared for the possibility that your pet might find a way to get to it.
Section 11 contains loads of great tips for preventing pets from accessing rodent baits.
Another thing to be aware of is that mice and rats and other rodents will carry baits
around your house. These animals are caching animals, which means that they carry excess food
back to their nests for eating later on. It is not uncommon for mice and rats to carry loose and non-anchored-down rodenticide pellets about the house with them.
Although this caching habit is useful in the eradication of large rodent populations (poison carried back to the nest will be eaten by and thus kill many rodents), the moving of baits can pose a risk to your pet. A rat bait that you carefully placed out of reach in the ceiling, may well find its way, via rodent transportation, onto the carpet
of the living room where your dog or cat could access it and become poisoned. Birds too, will often
move baits around the place. Crows, ravens, currawongs, magpies and other birds are very curious
animals, often attracted to the brilliant blues and greens used in most wax blocks and pellets. Birds that consume pellets will often be poisoned, but large wax blocks may be easily picked out of ceiling spaces and gutters by curious birds and, found to be unpalatable, dropped into the yard, where your dog could access it. Section 11 contains loads of great tips for preventing mice and rats from moving baits around.
 Another common 'at-home' poisoning situation that I have encountered is the poisoning that occurs when
a person, normally a renter or new house-owner, moves into a new house for the first time, unaware that the previous tenant has put down rat poison. Generally, if the new owner or tenant
has explored his or her new house thoroughly, he or she will have removed any rodenticide boxes located in obvious areas like the corners of rooms and the inside of kitchen cupboards. However, there are many obscure places that people will commonly hide bait boxes. Places to also check include: garden sheds, the gap behind or alongside garden sheds, behind hot water systems (e.g. under the kitchen sink), behind doors (the space
behind the door that gets hidden when you open a door into a bedroom), inside walk-in-robes,
inside pantries, behind or alongside the fridge, under the house (beware of snakes and spiders if you check here though), under the oven, in the gap beside the
oven and bench or the oven and nearest walls, inside the ceiling space. Without a careful, step-by-step, systematic, house-and-yard hunt for these hidden baits, you may not even notice them, however, you can be very sure that your canine or feline friend's keen nose will discover them one day when you are out at work.
Another common 'at-home' poisoning situation that I have encountered is the poisoning that occurs when
a person, normally a renter or new house-owner, moves into a new house for the first time, unaware that the previous tenant has put down rat poison. Generally, if the new owner or tenant
has explored his or her new house thoroughly, he or she will have removed any rodenticide boxes located in obvious areas like the corners of rooms and the inside of kitchen cupboards. However, there are many obscure places that people will commonly hide bait boxes. Places to also check include: garden sheds, the gap behind or alongside garden sheds, behind hot water systems (e.g. under the kitchen sink), behind doors (the space
behind the door that gets hidden when you open a door into a bedroom), inside walk-in-robes,
inside pantries, behind or alongside the fridge, under the house (beware of snakes and spiders if you check here though), under the oven, in the gap beside the
oven and bench or the oven and nearest walls, inside the ceiling space. Without a careful, step-by-step, systematic, house-and-yard hunt for these hidden baits, you may not even notice them, however, you can be very sure that your canine or feline friend's keen nose will discover them one day when you are out at work.
Another 'at-home' situation to be aware of is rodenticides in other people's houses. You might be completely anti-chemicals and anti-poisons, but that certainly does not mean that other people
share your views. When taking your dog or cat to other people's places (particularly
people without pets or children), be aware of the potential for there to be poisons about in that home. Having poisons in the house is certainly not a slur on those people who have them - most people, particularly those without kids and pets to be cautious of, find rodenticides a highly effective, cheap and easy way to rid themselves of a vermin problem. It just might become an issue should you elect to bring your pet around and let it wander, unobserved, throughout their house. Most people, particularly your friends, don't mind if you politely enquire whether there is anything that could hurt or poison your pet companion. If poisons are present, you will have to keep your dog or cat with you on a lead and perhaps consider not bringing it with you the next time you visit.
An important author's note: rodenticides are not only poisonous in their edible
pelleted, powdered or wax-block forms. It is possible for animals (cats in particular)
to become poisoned after walking through powdery bait residues: they get bait powder
on their paws and then consume it when they lick and groom themselves. It is also possible
for animals and humans to become poisoned through inhalation of rodenticide dust
and powder. Masks should be worn when laying out baits (especially powdered or pelleted
baits which have a powdery residue) and baits should not be placed where these powders
can be easily blown into the air and inhaled.
4b) Poisoning in the field (outdoors):
Dogs and cats and livestock animals can become poisoned if allowed to wander and fossick for tidbits on properties where rodent control programs are underway. Factories, particularly
those engaged in food production; grain storage areas (e.g. silos); hay and silage storage areas;
aviaries (e.g. zoos and bird breeding facilities) and farms producing or using grain and fruit products are at high risk of developing a significant rodent infestation and owners of such premises
often use a wide range of rodent control products, including poisons. Wildlife corridors and reserves
also pose a high risk of poisoning to wandering pets because a range of poisoning programs
may be in place in such sanctuaries to control feral pest animals (e.g. possums and rats in New Zealand, foxes,
cats and feral dogs in Australia).
Typically, the anticoagulant rodenticides are favoured for use in farm, grain and hay storage
and factory facilities, however, unlike the home, it is also not uncommon for some of the other, more dangerous rodenticides (e.g. cholecalciferol, zinc phosphide) to be used. Because factory and farm owners are generally not expecting domestic
pets (or children) to wander around their premises consuming their baits, these baits are often left out in easy-to-reach, unprotected packets that pets and kids can easily access and consume. For example, in parts of Australia and other countries,
it is common for farmers to soak carrots and vegetable cuttings in rodenticide powder (e.g. strychnine powder when it used to be freely available) and leave these out in the open paddock for feral rabbits. These poisoned veggies, placed in such a way, can be easily accessed by wandering domestic pets and livestock and wild fauna that come into contact with them. Often causing severe organ damage or severe, acute neurological dysfunction and often having no effective antidote or easy means of diagnosing the toxin, these alternative rodenticide poisons pose a much more lethal risk to the wandering, bait eating pet than the anti-coagulant rodenticides do.
Wildlife reserves, similarly, pose a high risk of poisoning with dangerous non-anticoagulant
rodenticides. Although many feral animal baiting programs do include anticoagulant rodenticides
in their repertoire, most of the highly effective, second generation anticoagulant toxins pose a
high risk of leaving poisonous environmental residues behind (in soil and water and organic matter)
and a high risk of causing secondary poisoning to wild animal predators and scavengers of
carcasses. Consequently, it is the low-residue, low-persistence, low-secondary-poisoning-risk
rodenticides that are favoured in wildlife corridors and reserves, including: cyanide, vitamin D analogue baits, zinc phosphide baits and 1080 baits. These non-anticoagulant
baits, although better for the environment as a whole, are often lethal to roaming pets. Monofluoroacetate (1080), in particular, is a highly lethal bait commonly used in animal
reserves within Australia and New Zealand and elsewhere to poison feral animals (mostly
cats and foxes and mustelid species, but occasionally rodent vermin as well).
Occasionally, farms engaged in the production of meat and animal products (e.g. beef, milk, pork, poultry) will also employ poisoning programs targeting the mice and rats that infest and spoil the grain and grain-meal products used to feed the livestock. Such farms have to be very careful in the placement of their baits: pigs and poultry are attracted to the grains used in rodenticides and can become poisoned by inappropriately-placed baits. Additionally, it is possible for certain consumed bait residues to build up in the organs and meat of such animals, thereby posing a risk of secondary poisoning to human meat and offal consumers. To reduce this risk of meat contamination, producers of meat animals tend to favour low-residue rodenticides such as cholecalciferol (vitamin D),
zinc phosphide and first generation, multiple-feed anticoagulant baits in their premises. These
poisons can pose a risk to domestic dogs and cats that come into the premises searching
for food.
Obviously farm, factory and wildlife reserve poisoning risks can be reduced by not letting
domestic pets and livestock animals wander freely in such baited areas. It must be mentioned, however, that pets can sometimes become poisoned as a result of such baiting programs without ever coming into direct contact with properties on which baiting is occurring. Similar to the situation described in section 4a, birds and caching
rodents are able to carry baits from farms and reserves for long distances, dropping them into areas outside the baiting zone (e.g. into your pet's yard) where domestic pets might access them. Because some baits take time to work, feral animals that eat a bait may travel for variable distances outside the baiting zone before suffering the ill effects of the bait. Vomit produced by these poisoned animals may be lethal to a dog or cat that decides to eat that
vomit (e.g. 1080 contained in vomitus is a good example) and, obviously, there is the additional risk of secondary poisoning to pets that consume the offal or carcasses of dead, poisoned animals
(see next section - secondary poisoning).
4c) Secondary poisoning:
Secondary poisoning is poisoning that occurs when a predatory carnivorous or omnivorous animal (domestic pet or wild animal) consumes the carcass of a poisoned animal and becomes secondarily
poisoned by the same toxin that killed the first animal. Although just as likely to consume ratbaits directly, dogs may become poisoned by eating sickly or deceased mice and rats and scavenging the carcasses of poisoned larger animals. Cats, in particular, are much more likely to become secondarily poisoned by anticoagulant rodenticides than they are to consume a poison bait directly. This is because they are keen hunters of rodents (poison-weakened
rodents pose an easy target) and because their finicky, selective tastes makes them less inclined to eat unfamiliar substances like pelleted or wax-block baits. The risk of secondary poisoning of cats and dogs is greatly increased with the anticoagulant-type rodenticides because weak, bleeding, dehydrated mice and rats often come out into the open to look for water: this makes them easy pickings for alert felines and canines.
Which poisons pose greatest risk of secondary toxicity?
Secondary poisoning is a particular risk with the second generation, single feed rodenticides (e.g.
bromadiolone, brodifacoum, difethialone) because these poisons are stored for long
periods of time in the rodent's liver and other tissues; because they are very potent
(small doses are capable of killing large animals) and because, at a single feeding, a mouse
or rat can potentially consume enough poison to kill not only itself, but a secondary
predator. Strychnine also poses a high risk of secondary poisoning of predators and
scavengers, as do long-lasting, high-residue poisons such as arsenic and thallium. The risk of secondary poisoning of domestic pets and wildlife is greatly reduced
with the multiple-feed, first-generation anticoagulant rodenticides because mice and
rats have to feed on these poisons several times in order to ingest enough to kill them: a dose of poison that is far under the amount required to kill a much larger dog or cat. The risk of secondary poisoning is also low with vitamin D analogue poisons, metal phosphide
poisons and cyanide-based poisons.
Secondary poisoning is also a risk with regard to the active hunting and consumption of 'healthy-looking' wild animals (e.g. deer) in reserves and consumption of meat-animals in farmland where poisoning is occurring. Certain poisons (especially the second-generation anticoagulant rodenticides) are high residue, difficult to break-down poisons, which build up in soils and waterways over time. These residues find their way into the livers, fat and organs of herbivorous animals grazing and drinking in these regions and accumulate to high levels within these organs. Humans, domestic carnivores and wild animal carnivores that hunt living, poison-contaminated wild herbivores (e.g. deer in New Zealand) or farm animals and consume the meat and organs (especially the liver) of these asymptomatic animals may potentially consume enough toxic residues to become poisoned. The risk of build-up of poisonous residues in the organs of live prey animals is highest with the second generation anticoagulant rodenticides
and certain heavy-metal poisons such as arsenic and thallium. Although diphacinone is categorised as a 'second-generation' product in terms of veterinary treatment
protocols, it is actually favoured in many wild animal and farm pest (e.g. voles, gophers) control programmes because it poses a low residue risk, lower meat accumulation risk and low environmental contamination risk
(i.e. it degrades quickly, leaving minimal traces). Likewise, cholecalciferol, zinc phosphide
and cyanide-based poisons are also favoured in such programs because they too pose a lower risk of tissue residues and environmental persistence.
A final note, it is also possible for predatory domestic pets and wild animals to become poisoned following the consumption of vomitus or stomach contents from recently-deceased
rodents and feral animals. The stomach contents (broken down vegetables and plant matter)
are a favoured source of vitamin and mineral nutrition for carnivorous hunters. With rapid-kill baits (baits that kill within minutes to hours of consumption),
the stomach contents of deceased pest animals can be full of poison pellets, poisoned meat
or poisoned vegetable matter and, consequently, pose a huge risk to the predator. Rapid-kill baits in which secondary consumption stomach contents can be a poison issue include: strychnine, ANTU, cyanide, arsenic and 1080 baits. Vitamin D analogues and anticoagulant rodenticide poisons, in contrast, tend to exert their effects over a period of days (2-5 days) and, by the time the animal dies, its intestinal tract is normally clear of the poison and thus does not pose a risk of predator toxicosis.
4d) How to know if someone has deliberately baited a pet?
The one question I am asked almost every time I get a case of pet poisoning into the clinic, be it rodent bait poisoning, snail bait poisoning or any other form of poisoning, is: "Do you think he or she could have been baited?" By this, the person
asking the question is usually referring to the deliberate, malicious baiting of their
pet by a neighbour, relative or stranger.
Certainly, the deliberate baiting of pets does occur (although it does not occur anywhere near
as often as pet owners seem to think it does). The most common instance occurs when
a neighbour or someone living close by perceives a pet to be a nuisance that needs to be dealt with.
Incessantly barking dogs are most commonly targeted by irate neighbours; as are wandering nuisance dogs; dogs and cats that dig in, urinate in or defecate in other people's yards and aggressive dogs that growl at or intimidate people as they walk past with their own pets or children. Sometimes these annoyed people will give owners a chance to change the behaviour of the pet (they might write the owner a warning letter
defining the issue or report the pet to the local council) but, if nothing changes, they may see no alternative but to take matters into their own hands. Some people give
no such notice, they just target the pet. Revenge attacks also occur sometimes with pet owners and/or parents targeting individual animals, usually dogs, that have attacked or threatened their own pets or children. Owners of pets that have been attacked by dogs are more typical of this because dogs that attack children are normally destroyed under government law, thus negating the need for a revenge attack. Occasionally, neighbourhoods will experience a rare, freak case of baiting where
an individual decides to poison someone's pet or a group of pets in a neighbourhood or suburb
for no apparent reason.
So how do you know?
The truth of the matter is that the deliberate baiting of pets is normally very difficult to prove
and prosecute, particularly if the poisoned pet in question is or was prone to wandering (wandering pets can go anywhere and pick up anything).
This difficulty in the diagnosis and
proof of baiting occurs for several reasons:
1) Many of the clinical signs seen with poison baiting could occur with a vast range of
non-poison-related causes. For example: seizures or convulsions may occur following the consumption some types of poison baits (e.g. 1080, bromethalin), however,
fits may also occur as a result of a huge number of metabolic diseases and brain diseases. Just because a pet has a seizure and dies does not mean that the pet was baited, even if the pet has never been witnessed to have a fit before. You need more evidence than just clinical
signs alone to prove poisoning.
2) Many of the toxins used in baiting are obscure and difficult to test for. Certain toxins (e.g. cholecalciferol) produce symptoms of poisoning and death well after the toxin
has left the stomach and blood stream (where it could be tested for). Some toxins (e.g.
zinc phosphide, bromethalin) may not have a reliable laboratory test for detecting them. Some toxins (e.g. neurotoxic fungal moulds and mushrooms) are so rare and obscure that one would
be unlikely to think to test for them.
The reality of poison testing in pets is that you need to have some idea of what the poison could be before you test for it. In the case of suspected deliberate baiting, you really have no idea: anything could be used. There are literally hundreds of poisons: testing for every possible toxin that is out there is not
only impractical, it is often highly expensive. The reality is that, unlike human poisoning cases
where cost is not an issue, most owners will not go to the expense of testing for every kind
of possible pet poison, particularly if the pet in question is already deceased.
3) It is rare for pets (especially cats) to never wander from their own properties and/or never go off lead during a walk. The second that you, as a pet owner, can not account for every moment of your pet's activities and locations within the last week is the moment that doubt of deliberate baiting must set in. It only takes a second for a wandering, hungry pet to find and consume a poisonous product. Pets that become poisoned as a result of wandering into other people's yards and properties are not considered maliciously baited. Land-owners have a right to place legal poisons in their own yards. It is the owner of the wandering pet who is in the wrong in this situation, not the homeowner who laid out the baits on his or her own property.
Author's note: with certain, highly-restricted poisons (e.g. 1080) land owners do have a responsibility to warn their neighbours if baiting is occurring. For example, 1080
baited properties must be sign-posted to let neighbours know. Land owners that fail to
put up such warnings may be at fault if a wandering pet becomes poisoned on their property.
4) Baits can be moved around by non-human sources. Although uncommon, it is not impossible for birds and rodents to carry baits around from property to property, leaving baits behind in yards that were not previously baited. Rodents, in particular, like to cache (carry foods, including poison-laced foods, back to their nests for later consumption). Rodents may travel great distances throughout neighborhoods looking for foodstuffs to bring back to their nests. You may have a rodent nest in your roof and a rodent willing to travel three streets away to collect and bring back a rodenticide block which, if
accidentally dropped, could poison your pet.
5) Secondary poisoning has no boundaries.
Just as rodents can move baits from yard to yard, so too can poisoned rodents move from
yard to yard. You may have no baits in your yard and yet your pet still manages to
become poisoned through the consumption of a sick rodent that happens to wander in.
6) Owners unaware of the timeframes of poison action can falsely assume their
pet was baited. Certain poisons (e.g. anticoagulant rodenticides, vitamin D analogues)
have a delayed onset of symptoms. Due to variable rates of bait digestion, 1080 can take up to 6-8 hours from time of consumption of the bait to create symptoms. The anti-coagulants can take 2-3 days to work. Vitamin D can take 2-5 days
to create tissue mineralisation and signs of renal failure. It is common for most owners to assume that their pet must have been baited on the day the symptoms appeared, when, in fact, the baiting may have occurred days ago when the pet escaped from its yard.
The fact is, a lot of deliberate baitings probably occur that can never be proven. Probably the vast
majority: people that suddenly discover a previously healthy pet dead in the yard
often never find out the truth about their pet's cause of death, baiting or otherwise. To help you, I
have listed some points of consideration that might help you to tell if your pet was baited and
if it was deliberate.
Indicators that baiting might have been deliberate:
You have been the recipient of letters of complaint or your pet has been reported to the
local council or police in the recent past. Most people dislike baiting and killing animals
and many will try to get a nuisance animal situation resolved peacefully and non-lethally
by writing a letter to the owner about the animal or reporting the problem to the council. These
letters of complaint will often be anonymous as people fear retribution from selfish or
aggressive pet owners. The mysterious death or illness of the pet, shortly after receiving such
a complaint, should be considered highly suspicious of deliberate baiting and
toxicological diagnostics would be highly recommended.
Author's note - not every owner of a nuisance pet will receive a warning in advance. People are terrified
of being targeted in return by angry pet owners and may simply bait the pet and remove
the problem with no prior notification.
Your pet has been involved in previous acts of cruelty or unexplained injury. This is normally the case for pets that regularly stray onto other people's properties and pose a nuisance there. Householders, farmers in particular (farmers with breeding bitches and livestock especially), can be very aggressive in their attempts
to deter and repel roaming, nuisance pets from their properties. Pets that find their way home with bruises or wounds from being kicked at or struck with objects (e.g. bricks, pipes); bullet-wounds or other weird injuries (e.g. I once treated a dog that returned home from a property with a lambing ring placed around its testicles: punishment for mating the farmer's prized kelpie bitches) may next time be targeted by that property owner with malicious baiting.
Your pet vomits or defecates bright green or blue pellets or chunks of wax. The presence of such material in the vomit or faeces is not in itself proof of malicious intent
(e.g. rodents can walk around with baits, pets can access baits by wandering on other people's properties), but it is a good clue that your pet has eaten some form of bait from somewhere. Most rodent and snail baits come in the form of dyed blue or green (occasionally brown) pellets or wax blocks.
Your pet vomits strange meat or foodstuffs that you did not feed it. Many would-be-baiters of dogs and cats tend to place poison substances into baits that are highly attractive to dogs and cats: meat and offal. Soft, tasty meats, such as chicken breast, sausages, mince and internal organs (liver, kidney) are favoured because bait is easy to hide inside them. Since an early effect of many poisons
(not the anticoagulant rodenticides, unfortunately) is gastric irritation and vomiting, many pets will bring up some of the ingested, poisoned meat products. This should be immediately suspicious
to you if you did not feed the animal the meat it vomits up; if the meat looks strange to
you (e.g. has a white, grey or colored powder or slime on it or has colored granules dotted
throughout it) and/or if there has been no chance of your animal wandering and scavenging food from other households or properties within the last 12-24 hours. Remember to check your own bin of course: your pet could have stolen the food from your own bin and be vomiting and trembling for reasons other than baiting (food poisoning, pancreatitis etc.).
Poison testing comes back with an atypical poison. It can be very difficult to prove malicious baiting when it involves poisons that
are likely to be commonly distributed throughout a neighborhood (e.g. snail bait, vitamin D analogues and anticoagulant rat poisons). Common poisons such as these could easily be picked up by a wandering pet or transported into your yard by a bird or rodent. If the poison, however, turns out to be a restricted, rarely encountered or difficult to access
poison (e.g. strychnine, 1080 (depending on the area), ANTU, thallium, cyanide, arsenic), then the chances of a pet randomly accessing this bait on a walk or roam is much less likely
and the likelihood of deliberate baiting increases.
There are colored (especially green or blue) pellets in your yard, that you did not put there. If you suspect a case of deliberate poisoning, search your yard thoroughly for signs of poison residues (e.g. a few green pellets scattered here or there). In particular, hunt along the fenceline. Most people are not that elaborate about poisoning pets. Most would-be-baiters just want to get in and out of a yard unwitnessed and will simply dump a few handfuls of bait over the fence in the hope that the pet will consume them and die. You can often find evidence of this poisoning with a thorough search.
As mentioned previously, it is possible for rodents and birds to bring baits into your yard that can poison your pet. In these cases, you are more likely to come across
one or two pellets or perhaps a wax block (or nothing at all) and these could be found anywhere in the yard, not just the fenceline. In the case of human-mediated baiting, there is likely to be a lot of bait present (a pile of
pellets or a couple of wax blocks - more than a rat would carry) and these are most likely
(not always) to be located near the fenceline. The only time you are likely to encounter piles
of pellets and bait with rodent activity is if your pet has unearthed a rodent nest
where the animals have been storing their food. In these cases the nest is likely to be located underground, in a hollow log, in dense foliage or in a man-made structure (e.g. wall, ceiling, car body), not out in the open.
The poisoning occurs while you are at work or in the middle of the night. Again, most baiters want to get in and out of a yard unwitnessed and want to maximise the chances
of the annoying pet dying. Many baitings will, therefore, occur while owners are away at work
(reducing the chance of owners finding the pet and saving it) or in the middle of the
night.
 Your house is broken into. Some baitings of pets (particularly the use of rapid-acting baits) occur because thieves are trying to rid themselves of a guard dog. The sudden death of a pet, shortly followed by a burglary, should always rouse suspicion that the pet was deliberately targeted.
Your house is broken into. Some baitings of pets (particularly the use of rapid-acting baits) occur because thieves are trying to rid themselves of a guard dog. The sudden death of a pet, shortly followed by a burglary, should always rouse suspicion that the pet was deliberately targeted.
There has been a spate of suspicious pet deaths in the area. Occasionally, someone will go around to various properties deliberately poisoning other people's pets. A large number of atypical pet deaths in one area should be instantly suspect. Sometimes these deliberate baitings will reach the news, but more often they won't. The vet clinics in the area will know about it though: veterinary clinics are the first places that pet owners go to when their pets have mysteriously died. If you are suspicious of a malicious baiting, it is always useful to ring a few of the
local veterinary clinics about it and ask if they have had any suspicious pet deaths
recently. If they have, this adds to the possibility that your pet has been deliberately targeted. Additionally, the veterinarians may have done tests on some of the pets and may even have diagnosed the name of the poison most likely used in the crime.
4e) Can human anti-coagulant drugs (e.g. warfarin sodium, "Marevan", "Coumadin") poison my pet?
Of course. Warfarin is warfarin, whether it be in the form of a medication for saving lives
or a rodent poison for taking them. Warfarin is commonly administered to human and,
occasionally, feline and canine patients for its anticoagulant properties. It is used in the treatment of people and animals who are prone to thromboembolism (blood clots)
and stroke. Used in excess or given inappropriately, warfarin medicine can cause excessive bleeding (poisoning symptoms) in patients that the medication is intended for
and in animals and humans that the medication was not intended for (e.g. curious dogs and cats that decide to eat their owner's warfarin sodium pills).
As discussed in section 3, it is not possible to 100% guarantee the effect
that warfarin ingestion will have on any one pet, even if the dose ingested is known. Some pets
are highly susceptible to very low doses of the drug for a multitude of reasons (renal disease,
liver disease, concurrent drug use etc.) and some pets will miraculously show no symptoms at all even after ingestion of a massive dose of drug.
To refresh, the LD50s of warfarin is as follows:
rats and mice - a single dose of 50-150mg/kg. LD50 for a Norway rat = 58mg/kg.
dog LD50 - 20-50mg/kg.
cat LD50 - 5-50mg/kg.
pigs LD50 - 1-5mg/kg.
rabbit LD50 - 800mg/kg.
The minimum dose required to poison some animals is usually estimated as being 10% of the LD50 dose. Please remember, however, that lower doses than this may harm some highly-susceptible animals
and, thus, you should always seek veterinary advice if your pet has inadvertently consumed warfarin medications or been given an overdose of prescribed warfarin.
NOTE: The same principle applies with other anticoagulant, warfarin-related medications. Dicoumarol, phenprocoumaron, nicoumalone/acenocoumarol are relatives of warfarin that
are still in use today for their antithrombotic properties. They too can poison pets.

5) Symptoms of anticoagulant type rat baits in dogs and cats - what they are and how they occur.
The most basic way of describing the effect of anticoagulant rodenticide toxicity
is to say that anticoagulant rodent poisons inhibit the ability of the poisoned animal to clot its blood. This effect is seen 36-72 hours (around 2 days) after ingestion of a lethal dose of bait and animals may hemorrhage anywhere into their bodies
(e.g. brain, lungs, chest cavity, abdominal cavity, joints, under the skin, into the eye and
so on) and so severely that they can go into shock and die.
The following discussion is mostly for those of you who are interested in how the
poison actually works in order to disrupt the animal's clotting mechanisms and
create the anticoagulant symptoms seen. Understanding how the poison works is useful because it aids your understanding of why symptoms occur; how long they take to occur; how the diagnostic tests work; why certain treatments are helpful and how long animals are expected to take to respond to treatment.
5a) An overview of normal blood-clotting mechanisms in the animal body.
In order to understand the mechanisms by which blood clotting can be made to fail, it is important to understand how normal blood clotting mechanisms operate within the healthy animal.
The diagram below is an outline of the three major mechanisms by which animals and
humans clot their blood and are prevented from bleeding to death from minor to moderate
traumas and the hundreds of tiny vascular 'accidents' that take place within the body
every second of every day. Don't panic! The diagram looks very complex, but you'll find
it quite simple once I have explained it.
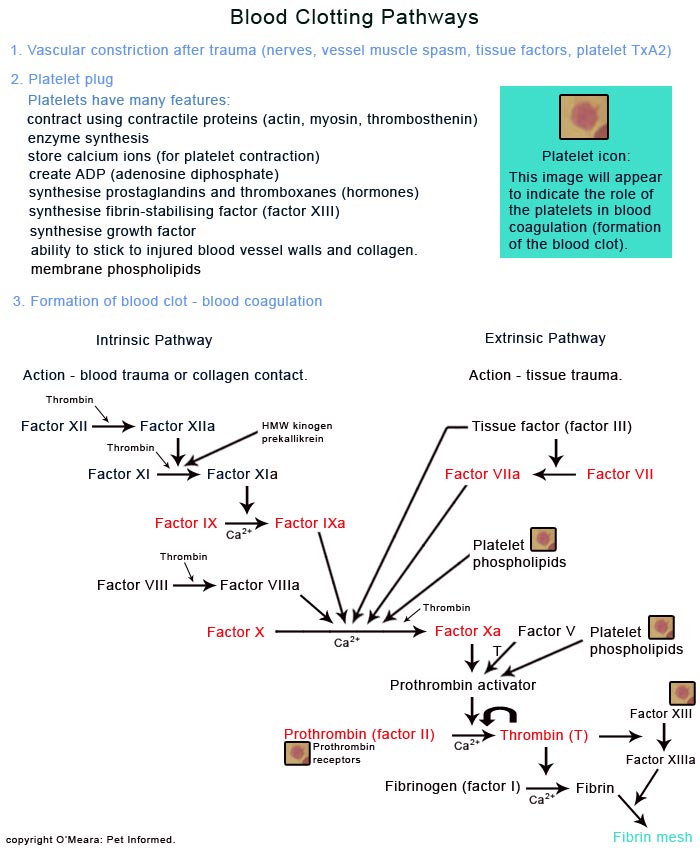
Image: A summary of the three main mechanisms of blood clotting - vascular constriction,
formation of a platelet plug and formation of a blood clot.
There are three main mechanisms by which the body acts to stem the flow of blood from an
injured blood vessel and prevent excessive bleeding. These are: the spasming and constriction
of the wounded/traumatised blood vessel itself; the clumping of blood platelets to
form a platelet plug (this plugs the hole in the blood vessel wall) and the activation of a complex blood clotting pathway (clotting cascade) in order to generate a mesh of fibrous webbing called a blood clot. Because no one of these processes will work 100% effectively without the contribution of the others (e.g. platelet factors are required by the blood clotting cascade and both the platelet plug and the blood clotting cascade are aided greatly by the blood-slowing effects of blood vessel constriction), all three processes will be discussed here. Although these mechanisms are all co-dependent on each other, the third mechanism (the formation of a blood clot) is the most important for you to read about with regard to this rodenticide topic because it is the process that gets disrupted by the effects of anticoagulant rodenticide toxicity.
A. Vascular constriction (spasming and narrowing of the traumatised blood vessels - part of primary hemostasis):
When a blood vessel is injured or traumatised, particularly if it becomes injured as a result of severe
external trauma (e.g. crushing of the blood vessels), the muscles within the wall of the blood vessel spasm, resulting in the blood vessel tube constricting down to a very
narrow size. i.e. the blood vessel goes from being a large diameter tube, capable of letting a lot of
blood flow through it, to a tube with a tiny diameter that lets little flow through.
This reflex blood vessel constriction is caused by a range of processes that are present at a site of trauma:
Nerve impulses: pain sensors and other nerve impulses in the traumatised blood vessel and surrounding traumatised tissues send messages about this pain back to the brain and spinal nerves.
These centres respond, sending nerve impulse messages back down to the blood vessel
walls, telling them to contract and narrow the vessel diameter.
Muscle spasm from trauma: muscles that are injured and torn often spasm as a direct result
of this injury. The muscles in the walls of blood vessels are no different: when they are damaged and irritated
they will spasm and tighten, resulting in blood vessel constriction.
Constriction induced by local hormones and inflammatory products: when bodily tissue is injured, it releases certain chemicals that act upon the walls of the local blood vessels, inducing them to constrict. Endothelin (a chemical released by the cells that line the blood vessel walls when they are traumatised); along with certain prostaglandins (chemicals released by traumatised tissues) and thromboxane A2 or TxA2 (a chemical that is released by activated platelets which come into the traumatised area as part of the platelet plug - see how the processes are all interlinked?) all act to stimulate local blood vessel constriction.
The overall effect of this vascular constriction is to reduce the volume of blood
passing through and along the damaged blood vessel (i.e. reduce the amount of blood
that can pass through the area and, thus, leak out of the hole in the vessel) and slow the
rate of flow of the blood moving through the injured vessel. Fluid, including blood, flows much more slowly through
narrow diameter tubing and this not only reduces the speed at which blood can leak through
the holes in the vessel walls, it also reduces the ability of the turbulent flowing blood to disturb and
disrupt the platelet plugs and blood clots which are trying desperately to seal the hole in the vessel
wall.
B. The platelet plug (also called primary hemostasis: 'primary' = first, 'hemo' = blood, 'stasis' = stop the flow or motion of. Quite literally - "the first way of stopping blood flow"):
Platelets are tiny discs, much smaller than a red or white blood cell, that are formed in the bone marrow of a person or animal through the fragmentation of a huge, nucleated bone marrow cell called a megakaryocyte. Essentially, platelets are just chunks of the megakaryocyte's cytoplasm, surrounded by a wall of megakaryocyte-derived cell membrane.
Platelets contain no nuclear material (no DNA) and, thus, they can not divide or replicate
within the bloodstream. They do, however, contain certain cytoplasmic enzymes, chemicals and
cytoplasmic organelles (tiny 'organs' within the cell's cytoplasm that act as factories to
produce the various proteins and chemicals needed for cellular function), which enable them
to complete their essential functions and tasks within the body.
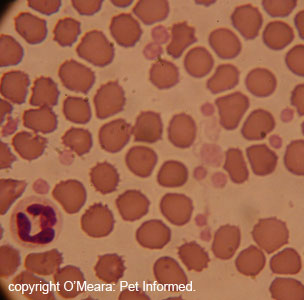
Image: This is a normal stained blood smear as seen through a microscope lens. The large red circles are red blood cells whose role it is to carry oxygen around the body. The much smaller, irregular, paler-pink circles are the platelets. A large white blood cell (a neutrophil), is seen on the lower left hand side. The white blood cell has a nucleus (the central lobe-shaped part of the cell that stains dark purple)
containing DNA. Notice how there is no darkly-staining purple center inside the platelets or red blood cells?
These cells do not possess a nucleus or DNA.
The wall of intact, undamaged, blood vessels is lined by a layer of extra-smooth cells called an
endothelium. This endothelium is so smooth and inert that normal platelets are unable to attach to
it and, thus, are unable to trigger the formation of a platelet plug or blood clot. This blood vessel wall inertness is one of the major mechanisms by which spontaneous blood clotting and platelet plug formation is discouraged by the body (excessive blood clotting is as undesirable as excessive bleeding: it can result in nasty problems such as strokes, blockage of blood vessels and the death of organs that are supplied with blood by those blocked blood vessels).
When a blood vessel wall becomes traumatised and develops a hole in it, the smooth
layer of endothelial cells is stripped away from the injured area as a result of the trauma,
exposing the roughened, irregular connective tissues underneath. In particular, loss of the endothelial
cell layer exposes the blood to collagen: one of the major connective tissues of the body.
Collagen is the minimally-cellular, fibrous connective tissue that supports and lends strength and structure to most bodily organs, blood vessel walls,
muscles and high-tension structures such as the eyeball, tendons and ligaments.
Collagen is what makes skin strong and tendons and ligaments appear white.
Exposure of the blood to the collagen underlying the endothelial cell layer is what initiates the
formation of a platelet plug. A platelet plug is simply a clump of tightly adhered platelets
that bind together at a site of blood vessel injury, essentially acting as a plug to halt the
loss of blood through the rent in the blood vessel wall. The outer membrane of the platelets
contains a coating of glycoproteins (molecules made up sugar and protein complexes), which adhere to collagen fibres located within exposed, traumatised tissues and within
blood vessels that have been stripped of their protective, smooth endothelial cell layer.
Author's note: this binding of platelets to the damaged areas of a blood vessel wall is not as straight forward as the platelets simply recognising a damaged wall and exposed collagen
and adhering to it. Platelets can only adhere to damaged endothelial cells and
exposed collagen in the presence of adequate volumes of von Willebrand Factor (vWF).
vWF is a chemical produced by normal endothelial cells that travels throughout the blood
stream and facilitates the adhesion of platelets onto regions of vessel wall injury.
Upon attaching to the exposed collagen, the platelets activate. They swell (filling the defect in the injured blood vessel wall even more); alter their shape (they stretch out their cell membranes in all directions, forming 'feet' that anchor them to the defect even better) and then they contract spasmodically (they contract using special, calcium-dependent, muscle-like, contractile
proteins contained inside them: actin, myosin and thrombosthenin). The contraction of the
activated platelets is a violent action which causes the platelets to expel and secrete many substances and chemicals that add to and enhance the formation of the platelet plug and which also contribute to the activation of the blood clotting cascade (next section).
These substances include:
ADP (adenosine diphosphate): this acts to 'turn on' other platelets in the region, increasing their 'stickiness' so that they then adhere to the activated platelets already attached to
the exposed collagen in the blood vessel wall. This increases the size and strength of the platelet plug, further
closing the defect in the blood vessel wall.
Thromboxane A2 (TxA2): this also acts to 'turn on' other platelets in the region, increasing their 'stickiness' so that they adhere to the activated platelets already attached to
the exposed collagen. Additionally, TxA2 also stimulates the wall of the blood vessel, making
it contract and constrict and narrow in diameter as described in process 1.
Various prostaglandins: these are chemicals with many functions, including various
roles in blood vessel constriction and dilation.
Factor XIII (fibrin stabilizing factor): a chemical compound which has a vital role in
the formation of a mature blood clot (see next section).
Growth factor: a hormone that acts upon the cells of the blood vessel wall (including
the muscle cells, connective tissue-producing cells and endothelial lining cells) and which causes
them to multiply and grow such that they permanently grow across and seal the hole in the blood vessel wall located under the platelet plug: a process known as healing.
Platelet phospholipids: the outer membranes of the activated platelets release fatty chemicals
termed phospholipids that play a vital role in the clotting cascade and in the formation of a blood clot (see next section). In fact, without platelet phospholipids, the ability of the animal
or person to form a firm blood clot is greatly impaired.
In addition to the chemicals secreted by the platelets, there is one other major role
that the platelet plug plays with regard to the formation of a stable blood clot (next section)
and this relates to the presence of prothrombin receptors. The platelets contain on their
surfaces, protein complexes called prothrombin receptors which bind to and 'anchor' one of the
major clotting factors in the blood clotting cascade: factor II, otherwise known as
prothrombin. The activation of prothrombin, which then acts directly upon a substance called fibrinogen in order to create fibrin: the final product of the blood clotting
cascade, is one of the very last steps in the blood clotting cascade. By having
the right receptors to bind prothrombin to them, the platelets ensure that the formation of the final blood clot occurs where it is most needed: in the region of blood vessel injury.
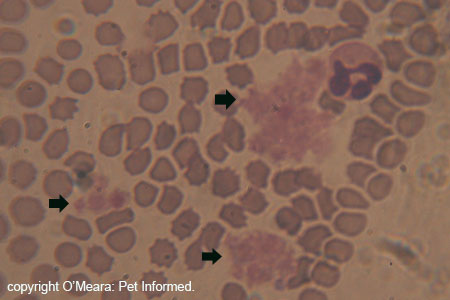
Image: Platelet clumps or platelet plugs (indicated with black arrows) as seen
in a blood smear. Sometimes, if you are not quick and atraumatic when taking blood
from an animal, the blood trauma involved in taking a blood sample from
a dog or cat can be enough to activate the platelets within the sample. These platelets
will secrete ADP and TxA2 and clump together in the blood sample, similar to
what occurs in traumatised tissues.
Question: The platelet plug seems to be very effective at plugging holes, so why do we need a blood clotting
cascade too?
The platelet plug is a really neat system, however, it is not very strong and can be easily swept away
in the current by large blood flows. As a result, although a platelet plug is highly effective at plugging and
sealing very small blood vessel tears (the kinds of miniscule vascular accidents and traumas
that happen hundreds of times a day in normal people and animals), on its own it is too weak
and flimsy to sufficiently plug a large hole in a blood vessel wall (i.e. the kind of hole that
occurs with venipuncture and large traumas). The role of the blood clotting cascade (next section) is
to produce a tight mesh of a strong, sticky, string-like protein called fibrin, which weaves in and around the platelet plug, binding it tightly, reinforcing its strength and anchoring it to the defect in the blood vessel wall so that it can not be easily swept away. The platelet plug bound and reinforced with fibrin from the clotting cascade is what is referred to as a blood clot. Without the support of a tough fibrin meshwork, the platelet plug alone will never be enough to plug a large tear in a blood vessel wall.
C. The blood clotting cascade (formation of fibrin mesh and blood clot), also termed secondary hemostasis:
This is the part where the complex, but critical, diagram comes in. Here it is again.
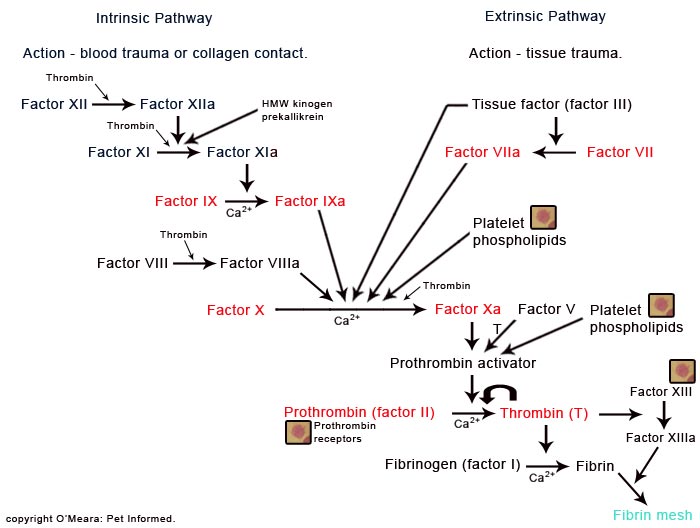
Image: This is a diagrammatical image of the blood clotting cascade, the part
of the blood clotting mechanism that gets disrupted by rodenticide toxicity. The clotting
factors printed in red writing (factors 2, 7, 9 and 10) are the clotting factors that
are depleted as a result of rodenticide toxicity.
As mentioned previously, the entire purpose of the blood clotting cascade is the formation of
a protein mesh called fibrin: a firm, thread-like protein which is designed to stabilize
and strengthen the platelet plug.
There are two main pathways (series of chemical reactions) by which the formation of
the fibrin mesh can occur. These are known as the intrinsic pathway and the extrinsic pathway
and they will now be discussed separately.
The Intrinsic pathway:
The intrinsic pathway typically occurs within the bloodstream and is a cascade of
chemical reactions that is initiated when a particular blood protein termed clotting factor XII or Hageman factor is activated by exposure to traumatically exposed collagen fibres (i.e. the collagen exposed in blood vessel walls) or as a direct
result of trauma to the blood itself (e.g. blood-injuring toxins such as snakebite toxin or
heavy metals or immune mediated hemolytic anaemia diseases).
The activation of factor XII results in the formation of an enzyme (an enzyme is an
active chemical compound that mediates or initiates chemical reactions of and between other
chemical compounds). We term this enzyme factor XIIa (the letter 'a' indicates that the factor XII has gone from being inert and non-reactive to activated). This activated factor XIIa then reacts with another protein in the blood, termed
clotting factor XI, to create an activated enzyme referred to as XIa. As indicated
in the diagram, the activation of factor XI by factor XIIa needs to occur in the presence
of a couple of blood proteins (called prekallikrein and high-molecular-weight kininogen) in
order for the activation of factor XIa to occur. Factor XIIa can not activate XI at all
without high-molecular-weight kininogen and, in the absence of prekallikrein, the
reaction can occur, but is so slow that it is too inefficient to be effective (i.e. the prekallikrein speeds the reaction up).
Factor XIa then reacts with yet another protein factor in the blood: clotting factor IX, to form an activated enzyme called factor IXa.
This reaction can not occur without the presence of adequate levels of ionised calcium (Ca2+)
in the blood. Calcium is vital to normal blood clotting processes.
Factor XIa then reacts with another protein in the blood: clotting factor X, to form
an activated enzyme called factor Xa. This is a more complex reaction than the previous ones. In order for factor X to be activated by factor IXa, many other chemicals and blood clotting factors
must be present. Adequate levels of activated factor eight (VIIIa): a clotting factor that
is not activated by the aforementioned clotting cascade, but by the presence of thrombin (one of the final products of the clotting process - see full diagram) must be
present. Adequate levels of platelet phospholipid: a chemical produced by platelets
when they come into contact with exposed tissue collagen and activate, must also be present. Additionally, there needs to be sufficient ionised calcium present in the blood in order for the
activation process to occur.
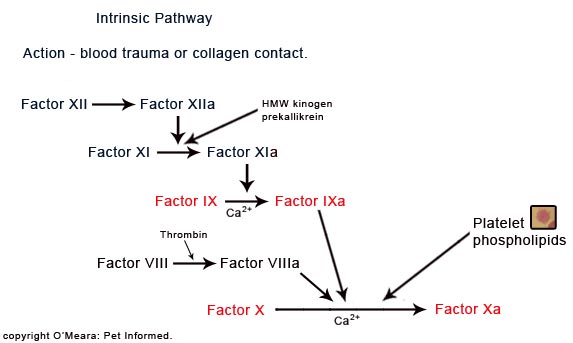
Image: this is a focus-diagram showing the intrinsic pathway of the blood clotting cascade.
It becomes disrupted by rodenticide poisoning.
The Extrinsic pathway:
The extrinsic pathway is a similar, but alternative, cascade of chemical reactions
that is initiated by the traumatised tissues (damaged blood vessel wall or damaged
underlying tissues) themselves. The tissues of the body, when injured, secrete a distress chemical
called tissue factor, which is similar in structure to the phospholipids released
by activated platelets (as described in the intrinsic pathway and platelet plug). This tissue factor, once released,
acts to activate a blood protein called clotting factor VII, in order to produce an enzyme called VIIa.
Factor VIIa then reacts with another protein in the blood: clotting factor X (yes, the same
one described in the intrinsic pathway), to form an activated enzyme called factor Xa. Similar to the situation described in the intrinsic pathway, in order for factor X to be activated by factor VIIa, other chemicals must also be present. Adequate levels of tissue factor (the distress protein that activated the factor VII) must be
present, in addition to activated factor VII (VIIa). Additionally, there needs to be sufficient ionised calcium present in the blood in order for the activation process to occur.
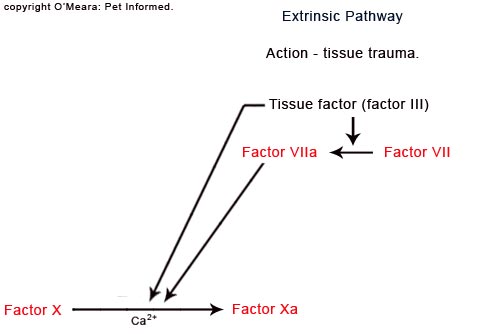
Image: this is a focus-diagram showing the extrinsic pathway of the blood clotting cascade.
It becomes disrupted by rodenticide poisoning.
As you can see from the above diagrams, the activation of the intrinsic and extrinsic blood clotting cascades both culminate in the production of activated factor X (Xa).
From this point on, the two pathways are identical, both following a common path
of chemical reactions (which is, funnily enough, called the common pathway)
in order to form a fibrin mesh - the ultimate final product.
One thing that is really important to mention is that, although we do illustrate
the intrinsic pathway and the extrinsic pathway as though they are separately occurring
processes, the reality is that they seldom ever occur independently of each other. It would be very unlikely for the intrinsic path to become activated in complete
absence of the extrinsic path and vice versa. This is because the initiating processes
(tissue trauma for the extrinsic pathway and collagen exposure or blood trauma for the intrinsic pathway)
would seldom occur in isolation. For example: it takes some degree of tissue trauma in
order for the underlying collagen of the blood vessels to become exposed (i.e. both paths activated).
The common pathway:
Following the activation of factor X, the activated form of this factor (Xa) then reacts with another protein in the blood: clotting factor II (typically referred to
as prothrombin), to form another activated enzyme called thrombin (essentially
factor IIa). Similar to the situation described for the activation of factor X, this reaction is highly complex. In order for prothrombin to be activated by factor Xa, many other chemicals and blood clotting factors must be present. Adequate levels of activated factor five (V): a clotting factor that is activated by the aforementioned intrinsic and extrinsic clotting cascades (by factor Xa) and by the presence of thrombin (one of the final products of the clotting process) must be present. Adequate levels of platelet phospholipid: a chemical produced by platelets
when they come into contact with exposed tissue collagen and activate, must also be present. Additionally, there needs to be sufficient ionised calcium present in the blood in order for the
activation process to occur. This combination of activated factor X, activated factor V, platelet phospholipid and calcium is sometimes referred to as Prothrombin activator.
You're probably wondering how it is that factor V and factor VIII (mentioned in the
intrinsic path section) can be activated by a chemical that is produced further
down the track (i.e. activated by a chemical that has seemingly not been created yet.)
The reason for this is that the blood clotting cascades described here are happening at low levels all
over the body all of the time. There is enough thrombin circulating at low levels throughout the animal's bloodstream (a result of many previous blood clotting cascade activities) to activate new blood clotting processes as described here. There is never 'no thrombin'
available in the body. Also, in the case of factor V, factor X also plays some role in its activation.
Thrombin, once formed, then acts as an enzyme. It reacts with yet another protein in the blood: clotting factor I (typically referred to as fibrinogen), to form a thread-like
proteinaceous substance called fibrin. This reaction can not occur without the presence of adequate levels of ionised calcium (Ca2+) in the blood.
This fibrin is the end-product of the clotting cascade, but it is initially not very useful. This is because, when fibrin is first formed, it is formed as individual strands, not the dense, interwoven meshwork that is essential for binding up and reinforcing the platelet plug.
Any bonds that do exist between these initially-formed fibrin strands are weak and easily broken down. One more step is required before the fibrin is useful.
Thrombin, in addition to its role in the production of fibrin, also serves to activate
a platelet-produced protein called factor XIII (usually referred to as fibrin-stabilising
factor). Factor XIII, when activated (XIIIa), acts upon the fibrin threads, altering their
chemical structures so that they cross-link with each other to form a strong, interwoven
meshwork that is united by extra-strong chemical bonds.
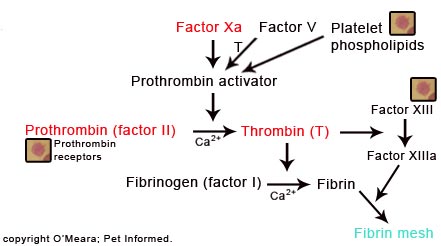
Image: The common pathway of the blood clotting cascade. The ultimate product is the fibrin
meshwork, indicated in green writing. This path also becomes disrupted by rodenticide poisoning.
A final thing to note about this blood clotting mechanism is that the blood clotting cascade, once initiated, ramps up, increasing in speed and magnitude the longer it is allowed to proceed. This occurs because of a positive feedback loop that is potentiated by the enzyme: thrombin. Thrombin is vital to the activation of factors VIII, XIII and V: the more thrombin
there is, the more of these factors get activated and the faster and greater the blood
clotting reaction proceeds. In addition to this, high levels of thrombin are also able to act as catalysts, accelerating the rate of activation of factors XII, XI and X and even feeding back onto its own production, enhancing the rate of activation of prothrombin into thrombin.
Question: the positive feedback loop mechanisms of the blood clotting cascade seem so immense. What stops the blood from clotting up indefinitely?
There are many control mechanisms in place within the body that tightly control and regulate the degree of blood clotting that occurs within the body and within injured tissues. These include the blood vessel wall structure itself (the smooth, inert endothelium layer); the thrombin-entrapping properties of the fibrin mesh (trapped thrombin is unavailable for
reaction) and the presence of anticoagulant hormones and chemicals such as: heparin, antithrombin III, Protein C, Protein S, thrombomodulin and alpha-2 macroglobulin. Also included are systems that actively break down the clots, once they have
formed, the main one being the plasmin system. I will not go into these systems in detail on this page as they are not essential to your understanding of rodenticide toxicity. Suffice to say, the body has many ways of controlling the excessive clotting of blood and ensuring that blood vessels do not become completely filled and occluded by the blood clots forming within their pipelines.
5b) What do the anticoagulant rodenticide poisons do to an animal's blood clotting mechanisms?
Once you understand the mechanisms by which blood actually congeals to form clots (section 5a),
in particular the blood clotting cascade (section 5a, part C), understanding the
mechanism by which the anticoagulant rodenticides and human drugs like warfarin sodium work to prevent blood from clotting is very simple.
Just about all of the clotting factors in the blood (factor I, right up to factor XII) are produced by the liver. Factor XIII is not - it is made predominantly by the platelets.
Of these, four factors in particular (factor II (prothrombin), VII, IX and X) are
created in the liver cells by a chemical process that absolutely, no-questions-asked, requires
the presence of active vitamin K within the liver cells. Without vitamin K, the liver can not
synthesize effective forms of these four factors, resulting in the complete failure of the intrinsic, extrinsic and common pathways of the blood clotting cascade and, consequently, a high likelihood of the animal suffering an uncontrollable bleeding episode.
How rodenticide poisoning affects Vitamin K:
Vitamin K exists within the animal and human body in two chemical forms: a reduced form and an oxidised form. Of the two forms, only the reduced form of Vitamin K is actually
functional and able to participate in chemical reactions that result in the formation
of the four vitamin K dependent clotting factors.
When a reduced molecule (active form) of Vitamin K has been consumed in a chemical
reaction within the liver, it exits this chemical reaction in an oxidised, inactive form.
This oxidised, inactive form of vitamin K can be reactivated, however, if it gets
converted back into its reduced form. Once reduced, the vitamin K can be used again
by the liver in more chemical reactions to make more clotting factors. This reduction and
reactivation of vitamin K is facilitated by two enzymes present within in the liver: vitamin K 2,3 epoxide reductase and vitamin K quinone reductase. If these two enzymes are not working, vitamin K recycling back to the active form can not occur and, consequently, the creation of active clotting factors II, VII, IX and X can not occur.
Warfarin and the anticoagulant rodenticides work by inhibiting the action of vitamin K 2,3 epoxide reductase and vitamin K quinone reductase, thereby preventing the
reactivation of 'used', oxidised vitamin K. Without the recycling of the Vitamin K, the liver is forced to use all of the body's reserves of active Vitamin K in the
production of blood clotting factors. Depending on the reserves of active Vitamin K
already present within the body, this complete Vitamin K depletion may take days (generally around 2-3 days). Once it is all gone, no more vitamin K dependent clotting factors can be created.
Following the cessation of vitamin K dependent clotting factor creation, there is a brief window of time whereby the animal can still clot its blood normally, whilst the most-recently-made clotting factors II, VII, IX and X are used up by the body. This window of time is under 12 hours. After this, the intrinsic, extrinsic and common blood clotting
pathways become disabled and the animal is at risk of suffering a major bleed.
Author's note: The active vitamin K is not required for the liver to actually create
the blood clotting factors II, VII, IX and X. The vitamin K is needed in order for the
liver to create reaction sites on the surface of the freshly created clotting factors
so that these clotting factors are able to bind calcium. As you can see from the flow
diagrams, calcium (Ca2+) is required in order for most of the clotting cascade reactions to
occur. In order to effectively participate in these reactions, the calcium needs to bind to specially-made
sites on the clotting factor molecules. It is the formation of these calcium binding sites
that requires the presence of the activated vitamin K. i.e. in the absence of active vitamin K, these clotting factors are still made, they just can't bind calcium to them
effectively and, consequently, are incapable of performing their roles in the blood clotting
cascade: they are created, but are useless to the body.
5c) Symptoms of rodenticide toxicity and how soon they appear.
As mentioned in section 5b, it takes time for the levels of Vitamin K and clotting
factors in the blood to become depleted. Consequently, the symptoms of anticoagulant
rodenticide toxicity (bleeding etc.), do not occur as soon as the bait has been consumed. It generally takes 36-72 hours (rarely, up to 5 days) for animals and humans to start to display symptoms of excessive bleeding tendency.
The severity of signs seen and the time taken for symptoms to show varies from
animal to animal and depends on the amount and type of poison ingested and on the animal itself. Higher doses of anticoagulant poison generally result in signs showing
up earlier and in more severe signs. Ingestion of a poison over several days is thought to
be more toxic to the animal than a single, large exposure (this is probably because
most of a single, large poison dose gets excreted in the animal's faeces before it
can all be absorbed into its body). Animals with large vitamin K reserves (e.g. that have been
on diets high in vitamin K) would be expected to manifest signs later than and of
less severity than an animal with low vitamin K reserves. Symptoms are more severe in
young animals and very old animals (probably because their ability to break down the
poison in their livers is less efficient). Signs generally seem to appear later in cats because of their naturally low physical exertion (they don't tend to run around
and traumatize themselves too much like dogs do).
Animals with symptoms of rodenticide toxicity can present in many ways, depending on where in the body the bleeding episode has occurred and how severe the bleed has been. Animals may bleed into any body cavity or tissue, including: the lungs, chest cavity, intestinal tract, joints,
abdominal cavity, brain and under the skin. Symptoms seen will generally relate to dysfunction of
these organs and/or to severe, generalized loss of blood from the vascular system (blood vessel system).
Non-specific symptoms:
Although some animals may present to a vet with very obvious, specific signs of bleeding
(e.g. vomiting blood, coughing blood, abdominal distension), it is not uncommon for animals to present initially for very vague, non-specific signs (signs that might not make you
think of rodenticide necessarily). Animals may present with symptoms of non-specific fever, depression, lethargy and weakness prior to overt bleeding signs. Pale gums might be
noticed, as might a sudden, unexpected collapsing episode from which the animal 'seems
to recover' without incident. Some animals show no obvious signs of where they have hemorrhaged
and simply present to the vet with signs of severe, inexplicable shock (pale gums, cold
extremities, cold rectal temperatures, depression, reduced mentation and responsiveness
and high heart rates). Some animals give no warning and are suddenly found dead
in the backyard (often due to a bleed into the brain or heart or a rapid, catastrophic bleed into a large abdominal cavity).

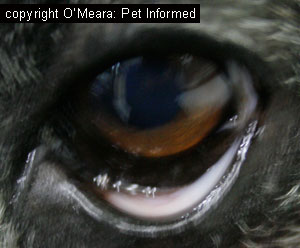
Image 1: These are the pale, almost white, gums of a dog that was in severe shock as a result of excessive haemorrhage. Ignore the black patches on the gums (this is natural pigment) and look
at the pale patches between the black spots. These spots should be salmon pink in color, not nearly white. This dog had severe anemia (lack of blood).
Image 2: This is the conjunctiva of the same dog (the normally-pink tissue that is seen
when you roll the lower eyelid out, exposing its underside). It is very pale also. Examining the
conjunctiva (which is normally pink) is a useful way of assessing the mucous membrane (gum) colour
of a dog with very black, darkly pigmented gums.
Animals that bleed into the lungs:
Animals that hemorrhage into their lungs may present with mild to very severe degrees of breathing difficulty. These animals will tend to adopt a rapid, shallow pattern of
respiration (almost panting) and, in severe cases, will be in considerable respiratory distress. These animals will often be reluctant to lay down or lay on their sides and they prefer to
stand still because any exercise exhausts them (they can barely breath standing, let alone walking).
They will often stretch out their necks in an attempt to get more oxygen down their windpipes.
These animals may present to vets coughing up blood and, in severe cases, may have blue-grey colored gums and be collapsed and unable to walk. Severely affected animals often die from a lack of oxygen uptake (they basically drown in their own blood).
Animals that bleed into the chest cavity.
Animals that bleed into the chest cavity space surrounding the lungs will also present
with difficulty breathing. These animals will tend to adopt a shallow, rapid respiratory
pattern and may be in considerable distress if the bleeding has been severe. Like the animals that haemorrhage into their lungs, these animals will often be reluctant to lay down or lay on their sides and prefer to remain standing upright and still because any exercise exhausts them (they can barely breath standing up, let alone walking).
These animals will often stretch out their necks in an attempt to get more oxygen down their windpipes.
Because the bleeding occurs into the chest cavity and not into the lungs, these animals will
not tend to cough nor bring up any blood (unless both sites have experienced bleeding). Because the chest space is so large, chest cavity bleeds can be very severe (animals
can lose a lot of blood into the chest space) and these animals may present with very pale
gums and sudden collapse as a result of acute, high volume, severe chest bleeds. These animals will often
be exhibiting signs of shock (depressed, collapsed and pale with cold extremities) and anaemia
and, if they are not treated quickly, they can die from a lack of oxygen supply to the tissues (blood
is required to carry oxygen to the organs, especially the heart, brain and kidneys).

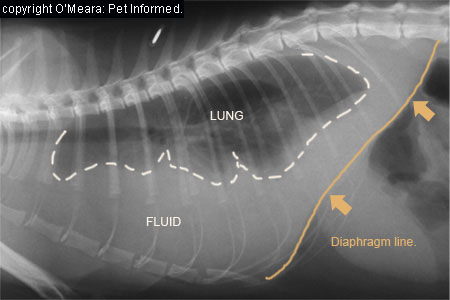
Images: These are radiographic images of a dog's chest with fluid occupying the potential space
(pleural space or pleural cavity) that exists between the lungs and the chest wall (rib cage). The fluid (white-colored density labeled Fluid) is actually blood from haemorrhaging that occurred following the consumption of rat and mouse bait. The lungs are the black-colored leaf-shaped structures, outlined in dashes, floating on top of the fluid. See how small the lungs are? They are being compressed by all of that blood. This animal nearly died from its severe, acute haemorrhage and trouble breathing.
Animals that bleed around the trachea.
This seems like nit-picking semantics, but it is important to note. Haemorrhaging into the tissues lining and/or surrounding the main airway, the trachea, is actually quite common
with rodenticide toxicity and can be extremely life-threatening. It can also be tricky to
diagnose. The pressure placed on the trachea by the blood can result in severe collapse and narrowing of the main airway. These animals are often severely distressed as a result of upper respiratory obstruction and display obvious difficulty breathing in. A high-pitched, whistling inspiration or wheezing sound may be noticed as the animal
breathes in. Allowed to progress, these animals may die from complete closure and obstruction
of the upper respiratory tract.
Animals that hemorrhage into the pericardium (the sac surrounding the heart):
Occasionally, animals with clotting factor deficiencies will bleed into the heart sac
(pericardium). The blood within the sac exerts pressure upon the heart chambers, stopping them from filling
properly and thereby inhibiting the heart's normal pumping activity. These animals will often present to a veterinarian for weakness, wobbliness and pale colored gums, however, they can sometimes present for acute collapse and shock and even sudden death (if the bleed has been severe). These animals will often display a deep, grunting respiratory pattern and sometimes owners will report that their dog was vomiting or retching prior to
arrival at the vet clinic (vomiting can be an early sign of pericardial bleeding). The vet may suspect the problem because the animal has an enlarged jugular (enlarged vein in the neck) or
because the heart is muffled and the heartbeat difficult to hear, however, the condition is
normally best confirmed using ultrasound (see image below).

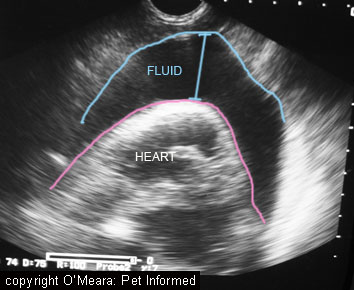
Image: these ultrasound images are the same, however, the second has been labeled for ease of understanding. These images are ultrasound pictures of a pericardial (heart sac) bleed in a dog that ate rat bait.
The fluid marked FLUID was actually blood in this case.
Animals that haemorrhage into the abdomen:
Animals that bleed into the abdominal cavity will often present to the veterinarian
with severe, acute collapse, pale mucous membranes (gums) and a hugely bloated-looking, expanded, distended abdomen (the belly swells, filling with blood). Huge volumes of blood can be
lost into an abdomen (a whole blood volume almost) and these animals will often display signs of severe shock (depressed, collapsed and pale with cold extremities) and severe anemia.
If not treated quickly, these animals can die from a lack of oxygen supply to the tissues (blood
is required to transport oxygen to the organs, especially the heart, brain and kidneys).
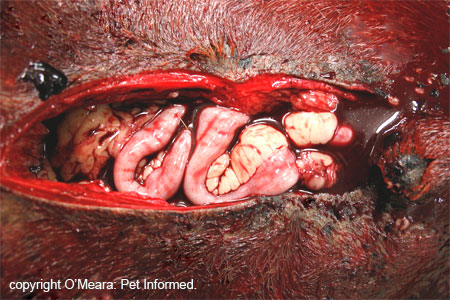
Image: This rather unpleasant image is of the abdomen of a dog that unfortunately died
at home from severe, acute abdominal haemorrhage. A post-mortem was performed to find a cause of death. The abdomen was very bloated and completely filled with blood. In this case, the animal had a ruptured splenic cancer, however, rodenticide toxicity would have presented very similarly. The blood coating the fur of the pet's belly gives you some indication of
just how much blood poured out when the abdomen was incised and just how severe and massive
in volume abdominal bleeds can be.
Animals that bleed into the brain:
Animals that hemorrhage even small quantities of blood into the skull cavity, brain or spinal canal can present with significant neurological signs. The signs seen vary greatly and are dependant upon the region of
the brain or spinal cord affected and on the severity of the bleed. Animals can present with anything from intermittent seizures; to wobbliness of the gait (incoordination); to paralysis
of one or multiple limbs; to tremors; head tilts or facial nerve paralysis. They may present
to the veterinarian simply for acting bizarrely: staring into space; circling a room endlessly; pacing restlessly
or compulsively pressing their heads into the corner of a room or cage (head pressing). In severe cases, animals may display uncontrollable seizuring, limb rigidity, non-responsiveness and coma. Continued, severe bleeding often results in massive increases in the animal's intracranial pressure (the pressure on the brain) and these animals will often lose their ability to breathe, regulate their heart rates and regulate their temperatures.
Regardless of veterinary attention given, many of these animals will die.
Author's note: not all animals that suffer a brain bleed will die. Animals with tiny bleeds that do not progress can often recover normal neurological function in days to weeks with the right medical therapy. Some animals that recover
may be left with permanent neurological dysfunction signs of variable severity and variable incapacitance.
Animals that haemorrhage into the intestinal tract:
Animals with bleeding into the gastrointestinal tract (stomach, esophagus, intestine or colon) are often pretty obvious. These animals will either vomit loads of fresh,
bright red blood and/or they will defecate faeces that are either black in coloration (signalling an upper intestinal bleed) or that contain fresh, bright red blood (suggestive of a lower intestinal, colonic or rectal bleed). Huge volumes of blood can be lost into an intestine (a whole blood volume almost) and these animals can go on to develop signs of severe shock (depressed, collapsed and pale with cold extremities) and severe anaemia. If not treated appropriately, these
animals may die from a lack of oxygen supply to the tissues (blood is required to get
oxygen to the organs, especially the heart, brain and kidneys).

Image 1: This is a large amount of blood in a dog's vomit. This particular animal
had stomach cancer, but could well have eaten rat and mice poison (we certainly tested for
it at the time).
Image 2: This tiny image is an image of the black faeces produced
by an animal with upper intestinal tract hemorrhage.
Animals that bleed into the urinary tract:
Occasionally bleeding will occur into the bladder or kidneys and the animal
will present to the veterinarian for urination of blood. Unlike a typical UTI (urinary tract infection), animals with blood clotting defects do not normally have bladder irritation and will, as
a result, usually show no symptoms of urinary discomfort (increased frequency of urination, pain on urination, vulval or penis irritation). They tend to simply wee as per normal, but fresh blood comes out with their urine.
Animals that bleed into the joints and/or muscles:
Bleeding into the joints seems to be a fairly common presentation for ratbait and other blood clotting defects. This is probably because the joints undergo a lot of concussive
force and minor trauma during normal daily activity. The animal will normally present to the vet clinic with an acutely swollen joint, usually one joint but occasionally two or more.
The animal will often be lame in the affected leg, not because of joint damage per se, but because of the blood build up stretching the joint's fibrous capsule (this joint capsule contains nerve receptors that detect stretching of the joint and stretching of the capsule with blood registers to the brain as joint pain). A needle placed into the joint
will yield fresh blood.
Animals will sometimes bleed into the muscles of the body, in particular, the muscles
of the limbs (e.g. the upper thigh and shoulder muscles). The animal may present for
an acutely swollen limb or muscle group and will often display signs of muscle pain
and a 'stiff' gait.
Animals that bleed into the skin, gums and eyes:
Animals may present to their veterinarian for severe bruising tendencies following the consumption
of rat bait. Owners may notice large patches of bruising on the skin or on the gums and eyeballs (scleras) of the animal. This bruising is often spontaneous with absolutely no history of trauma
preceding it. Any trauma that does occur to such animals (being hit with a ball etc.) will tend to result
in massive bruises, far in excess of the trauma that induced them. Spontaneous bruising can sometimes be seen on the gums and body as small, pinpoint spots of red called petechiae (petecchiae are particularly likely when the blood's platelets get consumed secondarily,
trying in vain to plug all the big bleeders that blood clots should have taken care of - see 6f)
or as larger areas of bruising termed ecchymoses. A bloodshot eye (bleeding into the
sclera - see image below) may be the first sign, as might bleeding into the eyeball itself. I had one observant owner who noticed her dog's tapetal reflection (the shiny part at the back of the dog's eye that makes it glow green or blue at night when light is directed at it) had changed from
green to red - that dog had hemorrhaged at the back of the eye.


Image 1: a dog with severe petechiation and bruising of the gums. This dog actually had a platelet deficiency (thrombocytopenia), but could easily have been a rodenticide case.
Image 2: a dog with severe bruising of the sclera possibly due to rodent poison ingestion.
Bleeding from the nose, ears and gums:
Animals will sometimes present to the veterinarian with uncontrollable bleeding of the nose (termed epistaxis), gums (usually in the areas directly around and adjacent to the teeth) or ears. A bleeding disorder must be considered a possibly
if these things occur with no known inciting trauma.
Animals that bleed from cuts:
Many animals present to vet clinics for rodenticide toxicity because a small, simple cut in the mouth or on the body, which should have clotted within minutes, simply refuses to stop bleeding. Cuts, even large cuts, unless they have gone through a major artery or large vein, should stop bleeding within
10 minutes at most (the vast majority usually stop bleeding far quicker than this). Animals with
cuts that keep on bleeding should always be assessed for some form of bleeding disorder
and rodenticide toxicity is high on the list.
Animals that are diagnosed at the vet by sheer accident:
There are many cases of rat bait toxicity that show no obvious clinical signs, but which are
discovered when a veterinarian goes to perform another procedure on that animal. Vaccination
and blood taking are common examples: the vet sticks a needle into the pet's jugular to get blood or gives the pet a vaccination and the animal's injection site blows up with a huge hematoma (lump
in the skin full of blood) or bruise or does not stop dripping blood. More serious are those cases of bleeding disorder that are discovered by accident during major
surgical procedures: desexing, joint surgery (I have personally seen a case where a blood-filled joint
was operated on as a ruptured cruciate when the animal, in fact, had eaten rat poison).
These animals can rapidly go from routine surgeries to absolute disasters and these
patients may potentially die from acute, severe blood loss.
A special note on pregnant cats and dogs (queens and bitches):
Pregnant animals can be affected by anticoagulant rodenticides in a number of ways. Pregnant animals that go into severe shock as a result of severe hemorrhage may potentially
abort their foetuses due to the stress on their bodies (I have personally seen a rodenticide-affected
bitch abort her entire litter). Anticoagulant rodenticides do cross the placenta and
may affect the unborn puppies and kittens (fetal bleeding, in utero foetal death and even abortion
may result). It is also thought that the anticoagulant rodenticides
may enter the bitch or cat's milk and affect the nursing litter after birth, causing the neonatal
animals to hemorrhage. Nursing pups and kittens and litters born to a poisoned mother should receive vitamin K1 treatment like their mother and have their blood clotting ability
and vitamin therapy monitored using PT testing (see section 6d and treatment sections 8 and 9).

6) Diagnosis of anticoagulant rodenticide toxicity in pets:
6a) History from owner.
 In most cases of rodenticide toxicity it is the owners of the pet, not a wayward bird or nasty neighbour,
who have put down the rodent poison that has caused their pet to bleed. Thus, veterinarians
tend to get a very strong clue as to the cause of a pet's excessive bleeding simply by
asking the question: "Have you put down any rat bait lately?" Most owners will tell
the truth about this, even if they do feel a tad guilty, and this makes the vet's diagnosis and
treatment plan very easy. The only difficulty comes when owners will not admit that they have
put down a poison and the vet has to work-out what has gone wrong with the animal's blood. Such time delayed whilst a diagnosis is being sought may potentially cost a pet its life.
In most cases of rodenticide toxicity it is the owners of the pet, not a wayward bird or nasty neighbour,
who have put down the rodent poison that has caused their pet to bleed. Thus, veterinarians
tend to get a very strong clue as to the cause of a pet's excessive bleeding simply by
asking the question: "Have you put down any rat bait lately?" Most owners will tell
the truth about this, even if they do feel a tad guilty, and this makes the vet's diagnosis and
treatment plan very easy. The only difficulty comes when owners will not admit that they have
put down a poison and the vet has to work-out what has gone wrong with the animal's blood. Such time delayed whilst a diagnosis is being sought may potentially cost a pet its life.
Sometimes, an owner will even witness the animal consuming the bait or come home to find ripped up bait
boxes strewn throughout the house, yard or shed. In these cases, the animal most likely
won't be showing any clinical signs (remember it generally takes 36+ hours for rodenticide toxicity to manifest),
however, it is still best that the animal is taken to a vet clinic. Owners of poisoned
pets should always take the box of poison with them to the veterinary clinic because the
active ingredient on the box label gives the vet important information about how to treat the animal and for how long to treat (e.g. second generation rodenticides may need 5-6 weeks of treatment, compared to 1-2 weeks for first generation rodenticides).
Animals witnessed to consume a dead mouse or rat (one they didn't kill themselves)
or a very sick, weak mouse or rat or other rodent should also be checked out by a vet, particularly if the owner has been putting down a second generation anticoagulant poison or
a high residue poison such as strychnine. Veterinary advice should be sought if consumption
of such a bait is seen. In the case of the anticoagulant rat poisons, a PT test (see
section 6d) can be performed 2, 3 and 5 days after consumption to see if secondary poisoning has occurred.
6b) The vomit test.
Many of the cases of rodenticide poisoning that present to veterinary clinics
involve suspected recent poison ingestions (i.e. the bait was thought to have been consumed within the last hour or so). In many of these cases, the owner has actually seen the pet fossicking near the bait (but is not sure if any was eaten) or
has found ripped up bait boxes strewn about the house, shed or yard (but, again, is not sure if
any was eaten). Owners often bring these animals in to the veterinary clinic, uncertain as to whether the pet has actually consumed any bait.
Proof of recent consumption can often be made using a vomit test - making the animal vomit and seeing if that vomit contains tell-tale evidence of rat poison (blue or green pellets or wax blocks). This is an especially useful technique if the owner has several dogs at home, all potential culprits, and wants to know which of them ate the bait.
In a similar fashion, rodenticides will eventually make their way out the other end of the animal, carried by its faeces. Sometimes, particularly with large poison ingestions, the colored pellet
dyes (the greens and blues) will appear in the animal's faeces, coloring them the same colour
as the ingested pellets. This can be another clue that the animal has ingested poison bait.
Limitations of the vomit test:
The trouble with the vomit test is that it is prone to false negative results. An animal
that consumed ratbait more than 2 hours ago may not have any bait left in its stomach to vomit up
(it is likely to have moved on to the intestines). An animal that has consumed a large meal may have the ratbait mixed through it, such that the poison pellets are hard to recognise. Also, an animal that ate only a very small amount of rodenticide
may not show any obvious green or blue pellets in the vomit, even though that small amount ingested may have been enough of a dose to poison it. Consequently, it is possible for one dog in a multiple-dog family to have eaten most of the bait and be easily diagnosed as positive, and for another dog in the same family to not have
eaten as much and to be falsely diagnosed as not having consumed it because it does not show up
in the vomit. This has obvious health implications for that second, less-greedy animal.
The vomit test is also of absolutely no use in the case of animals that present with active bleeding
tendencies. By the time a poisoned animal shows signs of bleeding, it has already had the poison in its system for 2-3 days - there will be no poison left in the stomach to vomit out. It would be unwise, in fact, to make such an animal vomit on purpose because the vigorous action of emesis (vomiting) could cause the animal's stomach to haemorrhage and this could be life threatening to an animal with a blood clotting issue.
Additionally, the vomit test is probably not of much use as a diagnostic aid in the diagnosis of
secondary poisoning: even if a mouse or rat is vomited up, one can not be sure what the rodent
actually died of. The act of bringing up the consumed mouse or rat, however, may go some way towards preventing the pet from developing symptoms of rat bait poisoning
if that is what the rodent died from.

Image: rat bait pellets (green) in a dog's vomit.
6c) In-house testing - the ACT (activated clotting time).
An activated clotting time test (ACT) is a useful, user-friendly, in-house means of testing the clotting function and clotting speed of an animal's blood. The ACT basically involves the veterinarian extracting a sample (usually 2 milliliters) of the animal's blood and placing this blood into a pre-warmed (37-38C) tube containing blood
clotting activators (diatomaceous earth or fine glass particles) and agitating this
tube gently in order to see how long it takes for the first signs of blood clotting to appear. The time measured is compared to a reference range of known clotting times in order to see whether the patient's blood clotting times are prolonged or not.
Normal ACT values for the dog: 60-120 seconds.
Normal ACT values for the cat: many reference ranges have been quoted and a recent study found the normal reference range to be from 55-165 seconds in the cat.
An abnormally prolonged activated clotting time (ACT) is suggestive of an abnormality
in the patient's intrinsic or common blood clotting pathway (see section 5a). It is usually prolonged in cases of clinical, symptomatic rodenticide poisoning.
Problems with the Activated Clotting Time Test (ACT):
The trouble with the ACT test in the diagnosis of rodenticide poisoning is that a prolonged clotting time is not specific for rodenticide toxicity. There is a large number of other bleeding disorders including: end-stage liver failure, snake bite, DIC (disseminated
intravascular coagulopathy), vitamin K deficiency, many consumptive coagulopathies, many
dilution coagulopathies and hemophilia, that can reduce clotting factor levels in the
body and thereby prolong the ACT. Many of these disorders that can affect blood clotting factor
levels (e.g. end-stage liver failure) will be obvious from the results of other tests (e.g. blood panels)
performed at the time, however, some of these disorders (e.g. DIC), can be much trickier to differentiate
from rodenticide poisoning. Additionally, to throw yet another spanner in the works, severe platelet deficiencies can also result in a prolonged ACT. Platelet issues do not tend to prolong the ACT as much as the clotting factor disorders tend to do, however, the ACT is still longer than normal.
Another problem with the ACT test is that it is operator-dependent. Traumatic or overly slow
blood-taking; not taking enough blood and not heating the ACT tube to the right temperature (too hot or cold)
prior to testing can all result in alterations to the ACT, artificially shortening or prolonging it.
Author's note: In Australia, the glass ACT tubes used in the detection of blood coagulation issues are becoming very difficult for vet clinics to source and may soon be unavailable (this is
a huge issue for Aussie vets, especially ER vets, wanting a quick, cheap and easy snakebite and rodenticide detection test). At a pinch, blood can be drawn into a simple, empty glass tube (one without any chemical residues in it) and timed to see how long the blood takes to form a clot. Normal blood should clot within 10 minutes. The trouble with this crude means of testing is that differences in glass tube smoothness, glass composition
and tube size all affect the clotting times, making it difficult to standardize the test and know what the exact values are meant to be.

Image: a nice, complete clot - the kind of blood clot that would be expected in a normal animal with a normal blood clotting ability.
6d) Laboratory testing: the aPTT (activated partial thromboplastin time) and PT (prothrombin time) tests.
For a more accurate, non-user-dependent diagnosis of whether an animal patient actually does have a blood clotting issue and for added clues about the kind of blood coagulation issue it has (e.g. rodenticide toxicity, hemophilia), a PT and an aPTT test can be performed. These two tests are much more accurate than the ACT test and are routinely performed
by most veterinary labs as part of their blood coagulation (blood clotting) panel. Some specialist vet clinics and emergency centres have even invested in in-house
PT and aPTT machines that will run these essential tests in-house, thereby negating the need for
blood to be sent off to a commercial lab.
All that is required in order to run a PT and an aPTT is for a blood sample to be
taken from the patient and sent to an animal laboratory in a special, blue-topped citrate tube.
Author's note: I have personally not had any issues with sending off whole blood to a lab in a citrate tube for PT and aPTT testing. Many texts, however, state that, for optimal accuracy of results, the blood-in-citrate sample should be centrifuged immediately after taking the blood sample
and the plasma taken from the top of the sample and frozen. These texts suggest that
the frozen plasma alone should be sent to the lab for PT and aPTT testing.
The PT (prothrombin time):
The PT test is used to measure deficiencies in the blood clotting ability of the extrinsic and
common blood clotting pathways. It essentially measures the availability and activity of factors
VII and X in the blood clotting cascade. Because anticoagulant rodenticides disrupt the functioning of both factors VII and X in the extrinsic blood clotting cascade, the PT is expected to be prolonged with toxic rodent poison doses.
The PT test is an extremely useful test. Of all of the clotting factors affected by rodenticide
toxicity, factor VII is the shortest lived (i.e. it breaks down in the body the fastest out
of all four rodenticide-affected clotting factors). What this means from a practical
sense is that the PT result will become abnormally prolonged the earliest of any of the clotting time tests (i.e. earlier than ACT and the aPTT). The PT will initially be prolonged
whilst the ACT and aPTT times are still normal. The PT can therefore be used to determine if an animal has received a toxic dose of a rodenticide prior to the onset of complete failure of all of the other clotting factors and the intrinsic clotting pathway (i.e. before a severe, clinical haemorrhage is likely to be experienced by the patient).
If an animal is thought to have had possible access to rodenticide poison, but the owner
is not really sure what amount, if any, was ingested (e.g. the house has several dogs and the owner does not know which of them, if any, ate the rat bait) or if an animal is known to have eaten rat poison, but the owner and vet are not sure if a toxic dose was consumed, the PT test can be run 2, 3 and 5 days
after consumption of the bait to tell. A prolonged PT on any of these days tells the vet that the rodenticide has at least wiped out factor VII (and most likely the others) and that the animal does indeed require rodenticide treatment (vitamin K1).
Author's note: the PT does not need to be repeated on days 3 and 5 if the PT is prolonged
on day 2 (a prolonged PT on day 2 is sufficiently diagnostic). Nor does the PT have to be repeated on day 5, if it is found to be prolonged on day 3. The reason for testing the PT on days 2, 3 and 5 is because, whilst most rodenticide poisoning cases show prolongations
in their bleeding times by days 2 or 3 following the consumption of the poison, some rare cases
take up to 5 days after consumption for blood clotting issues to manifest.
The PT test can also be used in order to see whether there has been a clinical response to vitamin K1 antidote therapy (a positive response is further supportive evidence of rodenticide toxicity
being the cause of the problems). Following the initial administration of vitamin K1 supplements to an animal with a prolonged PT or symptoms of bleeding, the PT times should start to improve within 8-12 hours of the first dose and normalise within 12-24 (up to 48) hours if rodenticide toxicity or another form of vitamin K deficiency was the cause of bleeding.
Finally, the PT test can also be used in order to determine when it is time to stop giving
the vitamin K1. Some rodenticides persist in the body for short periods of time (under 1 week)
and others persist for up to 6 weeks or more. Treating every single animal for a
full 6 weeks is very costly (vitamin K1 is expensive). Vets can attempt to reduce vitamin
costs for the owner by giving vitamin K1 courses for a week's duration at a time and then, 2, 3 and 5 days after the last dose is given, checking the PT.
If the PT is prolonged on any of these days, the course of vitamin K1 needs to continue (maybe 1 more week and then
check again and so on), but if the PT remains normal, then the treatment can stop.
An important thing to note is that a prolonged PT is not, on its own, complete proof
of rodenticide toxicity. Other coagulation defects that impair the activity or availability
of factors VII and X can prolong this test including: end-stage liver failure, DIC (disseminated
intravascular coagulopathy), other vitamin K deficiencies, various consumptive coagulopathies
and dilution coagulopathies.
The aPTT (activated partial thromboplastin time):
The aPTT is used to measure deficiencies in the clotting ability of the intrinsic and
common blood clotting pathways. It measures the availability and activity of factors
XII, XI, VIII, IX and X in the blood clotting cascade. Because the anticoagulant
rodenticides disrupt the function of factors IX and X (and factor II of the common pathway), the aPTT is expected to be prolonged with toxic doses.
An important thing to note is that a prolonged aPTT is not, on its own, complete proof
of rodenticide toxicity. Other coagulation defects that impair the activity or availability
of factors XII, XI, IX, VIII and X can prolong this test including: end-stage liver failure, DIC (disseminated intravascular coagulopathy), other vitamin K deficiencies, various consumptive coagulopathies, various dilution coagulopathies and several types of hemophilia. The aPTT is, however, unaffected by platelet deficiencies, making it a bit more specific and useful than the ACT.
Measuring a prolonged PT and aPTT together in the one animal is highly supportive
of a diagnosis of anticoagulant rodenticide toxicity.
If the PT is prolonged, but the aPTT is not, then this result could still be supportive
of early rodenticide toxicity as described in the PT discussion (i.e. factor VII of the extrinsic clotting pathway has been depleted, resulting in a prolonged PT, but the other clotting factors have not yet become depleted, resulting in a normal intrinsic and common pathway and a normal aPTT result). Usually, however, by the time clinical bleeding is witnessed, both the PT and the aPTT will be prolonged. The window of time whereby the PT is prolonged and the aPTT is normal is generally very brief.
A prolonged aPTT with a normal PT is suggestive of a disease process other than
rodenticide toxicity or a vitamin K responsive coagulopathy (e.g. vitamin K deficiency). In rodenticide toxicity or vitamin K responsive coagulopathy, the PT should always be prolonged. A normal PT
and prolonged aPTT is more suggestive of a specific clotting factor deficiency such as hemophilia.
How the PT and aPTT tests are performed:
Only those lab junkies amongst you really need to read this: I have included this technical section mostly
for completeness as, generally, the details of these tests are taken care of by the labs
and we vets just read and interpret the results.
Put simply, the reason that blood does not clot within the blood citrate tube is because
the citrate additive binds up all of the calcium within the blood, making this calcium unavailable
to react with blood clotting factors and form a fibrin clot. If you review the
blood clotting cascade diagram you'll see that calcium is required in order for most of the blood clotting reactions to occur. If calcium is added in excess amounts (i.e. in excess of what the
citrate can bind up) to the citrated sample the blood will clot eventually in contact
with the glass tube.
What the lab does when it performs the PT or aPTT test is to add calcium to the
citrated blood or plasma sample. This will permit a clotting reaction to occur. In addition to this calcium, the lab also adds in a clotting activator substance that will initiate the clotting cascade and formation of fibrin in a manner
that favours either the intrinsic pathway reaction (aPTT) or the extrinsic pathway
reaction (PT) such that each can be measured independently. When the lab wants to
measure the aPTT, it adds a contact activator (e.g. similar to the collagen exposure
needed to initiate the intrinsic pathway) and some platelet phospholipid to the sample
and times the sample to see how long it takes for fibrin strands to appear. If you
look at the intrinsic path diagram, you'll see how a contact activator (e.g. collagen exposure)
and platelet phospholipid are required in order for this pathway to proceed. When the lab wants to
measure the PT, it adds tissue-factor-like substance to the sample and times the sample to see how long it takes for fibrin strands to appear. If you look at the extrinsic path diagram, you'll see how tissue factor is required in order to initiate this pathway.
6e) Laboratory testing - rodenticide detection testing.
Although rarely done in practice, it is possible for certain labs to run tests on animal
vomit and blood in order to determine the exact type of anticoagulant that might have been consumed (e.g. warfarin versus bromadiolone). Detecting a specific anticoagulant in blood or vomitus not only gives the veterinarian definitive proof of what is causing the animal's bleeding problem, it also gives the veterinarian a vital clue as to how long to treat the pet with vitamin K1 for. Second generation anticoagulant rodenticides need to be treated for
longer.
6f) Blood smear.
A blood smear is a routine, in-house procedure performed by most veterinarians and
diagnostic laboratories as a means of visually examining the cells that make up an animal's blood: the red blood cells, white blood cells and blood platelets.
Lots of blood disorders, metabolic disorders and infectious disease disorders can be detected or hinted at through the careful examination of a blood smear (e.g. immune-mediated hemolytic anemia,
thrombocytopenia, ITP, Babesia, Ehrlichia, feline infectious anaemia, liver pathology, sepsis).
In the case of rodenticide toxicity, a blood smear usually provides no real proof
of diagnosis. There is no one change that may be seen in a blood smear that is 'proof'
of rodenticide toxicity. The blood smear can, however, still be helpful in these cases, because a number of other diseases that present very similarly to rodenticide poisoning
(e.g. disseminated intravascular coagulopathy (DIC), immune mediated thrombocytopenia (ITP))
can be determined with the aid of a blood smear.
In ITP and DIC, there is normally an almost complete absence of blood platelets visible
in the smear. In the case of rodenticide poisoning, however, the blood platelet numbers
are usually normal or only mildly reduced and can still be detected on the smear. The only time that platelet numbers fall dramatically in rodenticide toxicity is when
the animal is bleeding excessively and severely and the platelets are being consumed
rapidly as they desperately attempt to plug up the holes in the vessel walls. Even then, the complete absence of platelet numbers is very unlikely (unlike the situation with
DIC and ITP where the platelet count is typically exceptionally low).
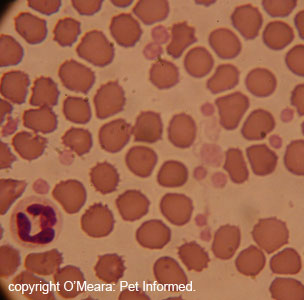
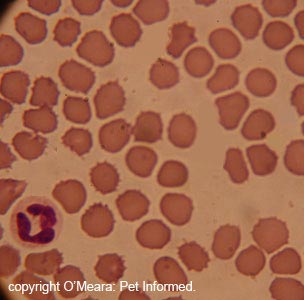
Image: The first image is of a normal blood smear. The platelet numbers are normal (platelets
are the smallest, irregular, pale pink fragments in the image). This is the kind of
blood smear that might be seen in a case of rodenticide poisoning.
Image: The second image is the same as the first image, but with the platelets removed
(ah, the wonders of photoshop). This is the kind of image that might be seen in a case of DIC or ITP.
6g) PIVKA (Proteins Induced by Vitamin K Antagonism or Absence) testing (also called the Thrombotest).
I will not go much into PIVKA testing on this page because it is not generally used all that often in veterinary medicine (it was originally designed as a more sensitive form of
PT testing to monitor the clotting times of humans on warfarin therapy). The PIVKA test or Thrombotest is run very similarly to a PT test: a clotting activator substance is added
to a citrated blood or plasma sample in order to initiate the blood clotting cascade and formation of fibrin in a manner that favours the extrinsic pathway reaction.
The sample is monitored and timed following the addition of the activator substance to see just how long it takes for fibrin strands to appear in the sample.
The test is thought to be more sensitive than the PT test for the detection of vitamin K antagonism or vitamin K deficiencies (e.g. as occurs in rodenticide poisoning).
It is also thought to be better able to detect subtle changes in an animal's extrinsic
blood clotting cascade, because the test is performed over a longer time span (longer
clotting times are expected with this test). This ability to detect very subtle clotting
abnormalities is what makes this test useful in the monitoring and fine-tuning of anticoagulant
medication therapies in people (and maybe cats on warfarin therapy too).
Like PT testing, PIVKA testing is not specific for rodenticide toxicity or vitamin
K deficiency. Any process that affects the activity and/or availability of the clotting
factors in the extrinsic clotting cascade (factors VII, X, II) will prolong PIVKA. These include: DIC, end-stage liver failure, congenital factor VII deficiency and
dilution coagulopathies.
6h) Treatment trial.
Another quick and easy way of adding to the diagnostic proof of rodenticide toxicity is
to treat for it. After all, treating animals with vitamin K1 is simple and poses an
extremely low risk of side effects. A few days of vitamin K1 therapy should normalise the animal's ACT, PT and aPTT times and result in a return to normal clotting function for the animal.
Although this treatment trial does not rule out other causes of vitamin K1 deficiency, it does
rule out a vast range of other clotting problems, including: end-stage liver failure, DIC (disseminated intravascular coagulopathy), consumptive coagulopathies, dilution coagulopathies and hemophilia.

7 Differential diagnoses of anticoagulant rodenticide toxicity in pets (other diseases that look like rat bait).
There are a number of bleeding disorders (termed coagulopathies: "coagulo" = blood clotting or blood coagulation and "pathy" = disease or disorder) affecting dogs and cats and other animals than can closely mimic the clinical appearance of rodenticide toxicity. Even specialist veterinarians with years of practice are unable to tell for sure exactly what an animal's particular bleeding disorder is being caused by without doing some form of diagnostic testing (e.g. the ACT, PT, aPTT and blood smear tests described in section 6).
The basic rule is: do not assume that any dog or cat that presents with a bleeding disorder must be rat bait only (unless you actually know the dog or cat consumed rodent bait or a deceased rat or mouse 2-5 days ago).
Do not self diagnose and do not attempt to self medicate your animal.
There are many diseases that cause bleeding problems and any excessive or prolonged bleeding
that won't stop must be seen by a vet. These are not cases where waiting until the next
day is appropriate - excessive, unceasing bleeding is an emergency.
Diseases of cats and dogs that can present as excessive bleeding and bruising tendencies
and an inability to clot the blood:
Snakebite (e.g. brown snake, black snake, tiger snake) - venomous snakes often contain toxins in their venom that disrupt the normal blood clotting
functions of the blood, resulting in excessive bleeding. Snakebite is diagnosed on the
additional symptoms shown by the animal (stiff gait, drooling, dilated pupils etc.);
on the owner's history (e.g. dog was walking in farmland) and on the results of snakebite detection kits.
Hemophilia A (factor VIII deficit), Hemophilia B (factor IX deficit), Hemophilia C (factor XI deficit) - these are individual blood clotting factor deficiencies
that are present within the animal from the time of birth. The affected animal is usually a young animal of a specific, susceptible breed (e.g. German Shepherd). Generally,
the aPTT is prolonged and the PT is normal.
Factor X deficiency - similar to hemophilia, but the PT and aPTT
are both prolonged.
Liver failure - these are generally very sick animals with other obvious clinical symptoms (jaundice, wasting, vomiting, pale faeces etc.) and very abnormal liver panels and liver function tests.
Vitamin K malabsorption - many diseases
and nutritional problems are capable of causing vitamin K deficiency in animals,
including: biliary obstruction (e.g. pancreatitis, bile or gall stones blocking
the bile duct) leading to maldigestion of Vitamin K1; poor diet (e.g. certain all-fish diets (esp. diets high in salmon or tuna) have an anti-vitamin K factor
in them that can cause vitamin K deficiency in cats); EPI (exocrine pancreatic insufficiency) which can be secondary to chronic pancreatitis and IBD (inflammatory bowel
disease). Usually cats with IBD and EPI have long history of diarrhoea, which is useful
to know from a diagnostic perspective.
Von Willebrand disease (vWD) - vWD is a congenital disease
restricted to certain breeds of dog (e.g. the dobermann, scottish terrier) that is normally discovered
by vets at surgery when the animal won't stop bleeding or at home when cuts won't stop bleeding. It has also been diagnosed in a cat before. These animals do not tend to spontaneously bleed
like the rodenticide animals do and diagnosis is made by testing for von Willebrands factor levels in the animal's blood.
Vitamin K responsive coagulopathy in Devon Rex cats - this is a congenital bleeding disorder that responds to vitamin K supplementation,
which generally manifests itself in Devon Rex cats from 5 months to 2 years of age.
Platelet deficiencies (e.g. immune mediated thrombocytopenia - IMT or ITP) - immune mediated thrombocytopenia is an immune system attack on the blood platelets
or bone marrow megakaryocytes (platelet precursor cells), resulting in a complete lack of blood platelets and lack of a platelet plug. The absence of platelets also causes
disruption to the blood clotting cascade because chemicals released by the platelets
are needed for it to function (e.g. platelet phospholipid, clotting factor XIII). Diagnosis
is made on the basis of a blood smear (no platelets) and a normal PT and aPTT.
Platelet function defects - certain breeds of dog and cat can be born with defects in their platelets and a loss of normal platelet
function (e.g. Smoke-blue Persian cats with Chediak Higashi Syndrome).
Drugs and medications that interfere with platelet function -
certain medicines (e.g. Beta blockers, calcium channel blockers, colloidal fluids, non-steroidal anti-inflammatory drugs (NSAIDs)
such as aspirin) can interfere with normal platelet function. Generally animals
that display an increased bleeding tendency with these products have some other bleeding
disorder going on as well which needs to be diagnosed (i.e. the drugs just tip them over
the edge, but they are not the main cause of the issue).
Clotting factor dilution (dilution coagulopathies) - this bleeding disorder usually occurs in dogs that have been given excessive intravenous
fluid volumes and multiple packed red blood cell transfusions. The excessive fluid given by the vet dilutes out the clotting factors in the animal's blood, making them inefficient and the animal likely to show excessive bleeding tendencies.
DIC (disseminated intravascular coagulopathy) - DIC is normally a secondary complication of severe, whole-body-affecting diseases or conditions such as: massive infection (e.g. severe parvovirus, severe pneumonia, peritonitis, pyometra); snakebite; blood transfusion reactions; cancer or body-wide inflammatory diseases (e.g. severe pancreatitis in cats, immune mediated diseases). Both the platelets and the clotting factors are wiped out. Animals with DIC have normally been very unwell for other reasons prior to the onset of excessive bleeding tendencies.
Bone marrow destructive diseases - bone marrow invasive
diseases such as cancer (e.g. leukemia, multiple myeloma, mast cell neoplasia) damage the bone marrow cells, resulting in a lack of platelet production. In the cat, these cancers can often be secondary to viruses such as FIV or FeLV.
Immune mediated diseases that damage the bone marrow - certain immune mediated diseases (e.g. systemic lupus erythematosis or SLE) damage
the bone marrow cells, resulting in a lack of platelet production. In the cat, these immune mediated diseases can often be secondary to viruses such as FIV or FeLV.
Certain drugs can also trigger immune mediated or toxic damage to the bone marrow cells, including: chloramphenicol, griseofulvin, albendazole, cephalosporin drugs and phenobarbitone
among others. Infectious diseases such as Ehrlichia can also inhibit platelet production in the bone marrow.
Drugs that cause bone marrow suppression - certain drugs are capable of suppressing
bone marrow function and platelet synthesis as part of their normal function. These include:
azathioprine, cyclophosphamide, cisplatin, carboplatin and certain other chemotherapeutic drugs.
In addition to the blood clotting disorders (coagulopathies), there are also many possible diagnoses
that might be made besides rat bait when an animal haemorrhages into a certain region of
its body. Obviously, diagnostic testing will determine if that animal has a blood clotting disorder
that is causing the issue, however, prior any specific diagnostic tests being run, when all that has been discovered is that there has been a hemorrhage, a number of differential diagnoses are possible for each site of bleeding.
Example 1: bleeding into the heart sac (pericardium) - animals can hemorrhage
into their pericardial sac as a result of a blood clotting disorder (any of those coagulopathies
mentioned above), however, bleeding into the pericardial sac can also be caused by a range of
other, non-coagulopathy disease processes too. It can be caused by trauma to the chest (e.g. a car or motor vehicle accident), by ruptured tumours growing on the heart (see image) and by a range of idiopathic causes (spontaneous
bleeds into the heart sac that we can not determine the cause of).

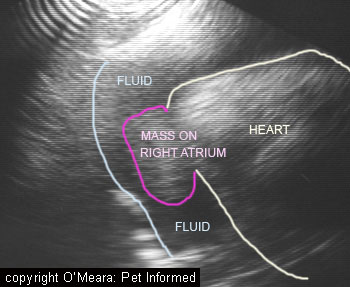
Image: This is an ultrasound image of a pericardial sac haemorrhage. In this case, the
animal did not have a bleeding disorder. It actually had a cancer or tumour growing from
the wall of its right atrium (a chamber of the heart). This tumour had ruptured and haemorrhaged
blood (labeled FLUID) into the sac around the heart.
Example 2: bleeding into the abdomen - huge abdominal bleeds, whereby the animal's belly becomes bloated looking and distended with blood, can be caused by a number of disease processes including: blood clotting disorders, trauma, rupture of a large tumour (e.g. a spleen or liver cancer) or rupture of a fragile, friable organ (e.g. a major cause of spontaneous abdominal bleeding in cats is liver fragility and rupture caused by invasion of liver tissue with amyloid:
a condition called amyloidosis).
Example 3: bleeding into the upper intestinal tract and the production of black stools - upper
intestinal haemorrhage can be associated with a range of disease conditions including:
bleeding disorders; intestinal, esophageal or stomach cancers; intestinal or stomach inflammation diseases (e.g. IBD), stomach ulcers secondary to mast cell cancers;
gastric ulcers secondary to certain drugs; ulcers secondary to renal failure or liver disease and the digestion of blood-filled foods (e.g. raw meat, liver).

8) Treatment of non-clinical rodenticide poisoning: What do I do if my pet has just eaten anticoagulant rat bait, but has no symptoms?
A lot of the phone calls we get at the emergency vet clinic come from owners who have just witnessed their pet eating rodent bait or who have just come home to find torn up
bait packets and are wanting to know what to do next. The animal is typically bright and
well and has no symptoms of rodenticide poisoning. It is usually bouncing all around the house
feeling very pleased about the nice green treat it has just eaten.
The 'good' thing about anticoagulant rodenticide toxicity (I highlight anticoagulant
because the same good thing does not apply to the other rodenticides out there), if there is a good
thing about it, is that it is not the kind of rush-to-the-vet-at-200-miles-an-hour type emergency that many of the other common household and farmland poisons are (e.g. snail bait, 1080, cholecalciferol, strychnine, ANTU).
It normally takes 2-3 days before any symptoms of anticoagulant rodenticide poisoning will occur and, if you can start treating the animal with vitamin K1 supplement tablets at any time prior to this (even starting a whole day after the bait has been consumed), the animal is unlikely to suffer from any bad side effects. As long as you supplement
the animals with active vitamin K1, the liver can produce the Vitamin K dependent clotting factors and the clotting of the animal's blood will occur as normal. Even if some or most of the anticoagulant poison does get absorbed into the animal's body, we vets have an effective antidote to that poison and can prevent the onset of any bleeding
signs. So, for those of you who only the discover the torn-up anticoagulant bait box the next day or who
have to travel many hours to a vet after witnessing the consumption of bait or who have to
wait until the next day to see a vet because of a lack of night service or because of the excessive
costs of an emergency night service, take heart and don't panic. Your pet is unlikely to show symptoms within 36 hours of eating anticoagulant ratbait; can be easily treated
with tablets and most likely will be completely fine and symptom free.
Having said that, if you do discover your pet in the act of eating bait or know that your
animal friend has eaten bait within the last few (3-4) hours, it is still best that you do take him or her to the vet, even if it is the middle of the night. You can drive at the speed limit. The reason for this is that your local vet can make the animal vomit and bring up the bait in its stomach, which will thereby reduce the amount of bait absorbed into the animal's body and may go some way towards reducing the length of time that you have to treat the animal with costly vitamin K1 (particularly with the second-generation baits that may persist in the body and need treatment for up to 6 weeks). Your vet can also start your pet immediately on the
vitamin K1 (the true name is phytomenadione) antidote, greatly reducing the risks of symptoms of toxicity developing.
8a) Making pets vomit in the vet clinic.
 If possible, it is always better if you take a pet to a vet clinic in order to
make it vomit. In my experience, most owners tend to find trying to make pets vomit at home an
unrewarding experience that often just wastes precious time in which a pet could be taken to a vet clinic and made to vomit. Vets have excellent drugs at their disposal to make pets vomit and tend to get much more reliable results.
If possible, it is always better if you take a pet to a vet clinic in order to
make it vomit. In my experience, most owners tend to find trying to make pets vomit at home an
unrewarding experience that often just wastes precious time in which a pet could be taken to a vet clinic and made to vomit. Vets have excellent drugs at their disposal to make pets vomit and tend to get much more reliable results.
Substances and medications used to make pets vomit in the veterinary clinic:
Washing soda crystals (Lectric Soda Crystals) - washing soda crystals are crystal chunks of sodium carbonate that froth up in
the animal's stomach acids and induce it to vomit. They are easily purchased and easy
to use and do not cause sedative side effects. They can be used in both cats and dogs.
IMPORTANT: washing soda crystals contain sodium carbonate and they are NOT the same as washing powders or detergents. Such substances can cause severe mouth and throat burns to dogs and cats and are very dangerous.
Apomorphine tablets - apomorphine tablets are tiny, grey, powdery tablets that can be diluted in sterile water and given to an animal by injection or
placed whole underneath the animal's lower eyelid, where they will absorb through the conjunctiva
and into the bloodstream of the animal, inducing it to vomit. The drug is very effective,
however it can be very respiratory and cardiovascularly depressant in small dogs and cats (it
can drop their heart rate a lot). I advise having your animal monitored by the vet
for a good few hours after successful apomorphine vomiting in case the animal's heart rate
drops. I have seen small dogs require atropine (a heart rate stimulator) after apomorphine emesis.
Dose rate for dogs: 0.08mg/kg subcutaneous injection.
Dose rate for cats: apomorphine is not generally given to cats because morphine-related opiate drugs can tend to make them manic. A dose of 0.04-0.08mg/kg intramuscular injection
apomorphine has been suggested by Rand (reference 7,45). Washing soda crystals are preferred.
3% Hydrogen peroxide - 3% hydrogen peroxide (H2O2), given at rate of 1-5ml/kg orally will make cats and dogs vomit. It is recommended that cats be given no more than 10ml total dose and dogs not more than 50ml total dose [ref 11]. I have no personal experience with its use.
Morphine - similar in affect to apomorphine, high doses of morphine (between 0.2mg/kg and 1mg/kg) will induce vomiting in both cats and dogs [ref 11]. I would tend to avoid its use, however, because these high doses can cause excessive sedation and heavily sedated animals that vomit are
at risk of inhaling their vomit and choking or developing aspiration pneumonia (lung infections).
Xylazine - Xylazine is an alpha-2 agonist drug that has often been used to make cats vomit. It is usually given at a dose of 0.44mg/kg intramuscularly to cats [ref 45]. Personally, I would tend to avoid its use or be very careful in its use, however, because this drug can cause excessive sedation of cats and heavily sedated cats that vomit are at risk of inhaling their vomit and choking, experiencing laryngospasm (an acute reaction whereby the cat's sensitive upper airway,
laryngeal cartilages spasm and slam shut, blocking the animal's upper airways) or developing aspiration pneumonia (lung infections). A good thing about Xylazine is
that it can been reversed after it has had its desired effect - there is an effective, rapid-acting antidote for this drug.
 What if you have more than one pet who could have eaten the bait? Do you take them all in to the vet?
What if you have more than one pet who could have eaten the bait? Do you take them all in to the vet?
If you do have more than one pet in your household and are unsure which of them ate the poison (whatever the poison is), it is always best that you take all of the animals to the vet to make them vomit. The reason for this is that you might be able to get all of your animals to vomit at home and, seeing a lot of bait in the vomit of one,
falsely, assume that it is the only animal to have consumed the bait. Just because you can't see bait in the vomit of the other pets does not mean that the other pet/s in the family have definitely not consumed a little of the poison. Small amounts of bait can vanish and dissolve in stomach contents really well. I have seen many cases (especially with snailbait) where an owner has assumed that only one animal ate the bait (even 'proved it' on vomiting) and taken it to the vet for treatment, only to come home later and find another pet nearly dead from seizures related to the consumption of a smaller, less obvious, amount of bait. It is best and safest to take all exposed pets (especially dogs - they like to fight over bait scraps) to the vet clinic for vomit induction, assessment and monitoring.
8b) Tips and cautions on making pets vomit at home.
 Making pets vomit in order to remove ingested poisons is only really helpful if the
animal is made to vomit within the first 2-4 hours of ingesting a poisonous substance. In the hours after this period, although some poison residues may still be brought up
if vomiting is induced, the vast majority of the poison load will have either been absorbed into the animal's body or moved on through the stomach to the intestines, where vomiting won't remove it.
Making pets vomit in order to remove ingested poisons is only really helpful if the
animal is made to vomit within the first 2-4 hours of ingesting a poisonous substance. In the hours after this period, although some poison residues may still be brought up
if vomiting is induced, the vast majority of the poison load will have either been absorbed into the animal's body or moved on through the stomach to the intestines, where vomiting won't remove it.
Taking this information and the information presented below into account, you, as an owner, have to weigh up the pros and cons of at-home vomiting induction and decide whether it is worth the time delay that you might cost your pet in trying and failing to make it throw up at home with at-home remedies. As mentioned in section 8a, most owners tend to find trying to make pets vomit at home an unrewarding experience that often just wastes precious time in which a pet could be taken to a vet clinic and made to vomit. Vets have much better drugs at their disposal with which to make pets vomit and they tend to get much more reliable results.
Situations where making your pet vomit at home may be appropriate (always ring your vet first before proceeding):
1) You live in the middle of nowhere, many hours from the nearest emergency centre
or veterinary clinic, and you need to remove a non-corrosive, non-acidic poison from a pet that
is fully alert and bright and has complete control over its throat (i.e. the animal is not
depressed, flaccid, limp, tremoring, fitting or comatose). Examples of poisons that can be removed by induction of vomiting include: anticoagulant rat poisons, cholecalciferol poisons, 1080 (not if the animal is fitting or tremoring), chocolate, bromethalin (not if the animal is fitting or tremoring), strychnine (not if the animal is fitting or tremoring) and snail pellets (not if the animal is fitting or tremoring).
There are many other poisons too - ring your vet for details on which poisons are safe to remove by making pets vomit.
2) Your pet has eaten a poison very recently and it is going to take you well over 2 hours to reach your nearest vet. Vomiting as a means of
preventing and reducing poison absorption is only really effective within the first 2 hours of consumption of a poison.
3) Your pet has eaten a really really nasty poison and you want to try something to get the pet started with vomiting (even if he or she vomits in the car) while you rush to the vet. A good example of this is seen with 1080 poison. Animals should be
made to vomit immediately upon ingestion of this stuff. It is lethal.
4) You simply can not afford to visit a night or after hours service for veterinary treatment and want to try something to get some of the poison out of your pet. As I mentioned before, with rat bait the risk of having a pet bleed to death within the first 36 hours of poison consumption is very unlikely and, generally, it is fine if
pets are taken to the vet the next day to start their Vitamin K1 treatment, regardless of
whether they have vomited or not.
With nastier poisons such as snailbait, 1080, strychnine, ANTU, vitamin D analogues and bromethalin, I strongly suggest taking your pet to a vet immediately for best chances of pet
survival and comfort. However, if this is absolutely not possible, then attempting to make a pet vomit at-home may be all that you can do to try to help the pet not develop severe, life-threatening clinical signs. Remember, however, that, if your pet does go on to develop severe symptoms (fitting etc.) of poisoning, even after having vomited at home, you do need to rush that pet to a night clinic for help, even if this help is only to put the pet out of its misery. Not doing so would be very cruel.
Situations when you should never attempt to make a pet vomit at home:
1) Your pet has eaten a highly acidic, caustic or corrosive poison (e.g. bleach, caustic soda). These kinds of substances burn on the way down, ulcerating the animal's mouth
and oesophagus, and they will burn just as badly coming up again, should you attempt
to make that animal vomit!
2) The pet has eaten a petroleum compound (petrol, oil etc).
3) Your pet has eaten a sharp or cutting object. Pets that have eaten razors or glass or kebab sticks or wire or any other sharp objects should not be made to vomit. These items will cut the animal's stomach and esophagus when the stomach contracts vigorously in the process of vomiting.
4) The pet is showing severe neurological signs. Animals that are seizuring or which have uncontrollable, violent muscle tremoring should never be made to vomit and certainly not without close veterinary supervision
(animals with very mild, early-onset muscle tremors will sometimes be made to vomit by veterinarians - removing the poison may stop the tremors from progressing and
becoming more severe). Animals with such severe neurological signs may not have good throat and swallowing control and may potentially inhale their vomit and choke. In a similar way, animals that are unable to swallow for various
neurological reasons should not be induced to vomit either.
5) The pet is comatose or non-responsive or severely depressed. A pet that is this depressed is unable to swallow whatever you give it and is at high risk
of inhaling either vomit-inducing medication given or the vomit that results. A pet that is
this unwell really needs urgent vet attention, not useless, ineffective stuffing around at home.
6) The pet has vomited or defecated and there is blood in the vomit or stools and/or the animal's faeces are black in color.
Many over-the-counter remedies used to make pets vomit at home (e.g. salt, washing soda crystals)
contain irritant properties that can ulcerate the throat, esophagus and stomach of the animal. Given that animals with blood in their vomit or stools already have some degree of ulceration of their stomach or intestinal tract, giving such emetics may potentially make this
ulceration much worse. Severe ulcers of the intestine can be life-threatening.
7) The pet is a cat. Although I have listed several
ways of making cats vomit at home (washing soda, Syrup of Ipecac, 3% hydrogen peroxide etc.), in my experience cats are very difficult to make vomit compared to dogs and may not respond to most at-home vomiting attempts. In addition to this, cats can sometimes develop
severe, life-threatening bronchospasm following vomiting induction. It is better to take cats to the vet for vomit induction.
8) The pet is a rat or horse. Rats and horses are not capable of vomiting and should not be made to.
Substances that can be used to make pets vomit at home:
Syrup of Ipecac - Syrup of Ipecac is an emetic
(vomit-inducing agent) that is available at most pharmacies and can be picked up from a night pharmacy in times of emergency. It should be in the cupboard of every pet owner and can be given to both dogs and cats to induce vomiting.
Dose rate cats: 3-6ml/kg, diluted 1:1 with water before administration (reference 45). The Veterinary Drug Handbook [ref 43] recommends giving cats a dose of 3.3ml/kg of ipecac syrup and doubling the resultant volume with water before dosing (to make a total dosed volume of 6.6ml/kg). This dilution (1:1) is important because cats find it non-palatable.
Dose rate dogs: 6.6ml/kg [Ref 18]. The Veterinary Drug Handbook [ref 43] recommends giving dogs a dose of 1-2.5ml/kg. The lower dose is probably a safer dose to start with.
If vomiting does not occur within 15 minutes of giving the Syrup, an additional dose can be given, but no further doses after that.
Note the used-by-date of the Syrup in your cupboard and throw it out after this date has
been passed (it is never ideal to use out-of-date pharmaceuticals).
3% Hydrogen peroxide - 3% hydrogen peroxide (H2O2), given at rate of 2ml/kg orally will make cats and dogs vomit. I have no personal experience with its use.
Salt paste - at a pinch, salt and water can be
mixed together to form a thick, salty paste (toothpaste consistency) and force-fed to the
suspect animal in order to make it vomit. You do not want to overdo it: you only need a few tablespoons at most for a large dog and much less for a small dog or a cat.
Author's note: many veterinarians and text writers advise against using salt paste to make pets vomit. If the pet fails to vomit after being given salt paste,
there is a risk of pets developing hypernatraemia (excessive blood salt levels)
and even gastric ulceration from the sand-like, irritant salt sitting in the bottom
of the stomach. If you do elect to give salt, I advise that you only give a single dose
to your pet. I would avoid salt pastes completely in any animal with medical issues,
particularly electrolyte and water balance issues (e.g. animals prone to renal disease, liver disease, diabetes mellitus, Addison's disease, diabetes insipidus, constipation,
Cushing's disease). I would also avoid the use of salt paste in any animal with a history of gastric ulceration, IBD (inflammatory bowel disease) or blood in the vomit or stools. Animals over 8 years old and under 4 months of age probably shouldn't be given salt paste.
Washing soda crystals (Lectric Soda Crystals) - washing soda crystals are crystal chunks of sodium carbonate that froth up in
the animal's stomach acids and induce it to vomit. They are easily purchased and easy
to use and do not cause sedative side effects (because they do not cause sedation or depression, there is less risk of the animal inhaling its vomit when washing soda
crystals are administered). They can be used in both cats and dogs.
Dosing: the animal is 'tableted' with 4-5 medium crystals of washing soda
(or given a handful of smaller, more powdery crystals). Most animals will vomit in 3-5 mins (10 minutes at most) of the crystals being given. If no vomiting occurs, do not repeat the dose, but instead give the animal 10mls of water orally. The water will make the crystals fizz and bubble and thereby induce nausea and vomiting. If nothing happens
despite the water being given, the dose of crystals can be repeated, but only once (excessive use of soda crystals can potentially lead to severe stomach ulcers). Repeating the dose is not really advisable if the animal has not vomited: there is concern that the extra dose could just sit there with the first dose and erode the stomach wall. If the animal does vomit, then the dose can be repeated to get any extra out poison out, however, if any blood is seen in the vomit, do not repeat the dose.
Washing soda crystals need to be "fresh" to work: they can get stale and become less effective over time (I would not keep an open packet for over 12 months).
IMPORTANT: washing soda crystals contain sodium carbonate and they are NOT the same as washing powders or detergents. Such substances can cause severe mouth and throat burns to dogs and cats and are very dangerous.


Image: people have been asking what the washing soda packet looks like - well here it is
(this is the Australian product anyway). These are washing soda crystals, also called Lectric Soda Crystals, and they contain the active ingredient: sodium carbonate. (NOTE - this product is different to sodium bicarbonate, otherwise known as bicarb soda).
Image: The washing soda crystals themselves look a bit like ice chunks.
8c) Gastric lavage?
 Gastric lavage or "stomach pumping" is the process whereby an animal that has eaten a
poison within the last 3 hours is placed under an anaesthetic and the poison washed out of its stomach
manually. Don't panic. No surgery is needed to do this. A medium to large diameter stomach tube is simply slid
down the animal's throat and into its stomach. Water is drenched down the tube to semi fill the animal's stomach and then this water is allowed to passively drain back out of the stomach via this same tube (or a second, larger tube) into a bucket, hopefully carrying the poison out of the stomach with it.
Gastric lavage or "stomach pumping" is the process whereby an animal that has eaten a
poison within the last 3 hours is placed under an anaesthetic and the poison washed out of its stomach
manually. Don't panic. No surgery is needed to do this. A medium to large diameter stomach tube is simply slid
down the animal's throat and into its stomach. Water is drenched down the tube to semi fill the animal's stomach and then this water is allowed to passively drain back out of the stomach via this same tube (or a second, larger tube) into a bucket, hopefully carrying the poison out of the stomach with it.
Gastric lavaging is really important, particularly for really aggressive, nasty poisons such as snail bait and vitamin D analogue poisons, because it helps to get that last 20-30% of the poison
out of an animal's stomach that was not removed by induced vomiting (or most of the poison out
if the animal didn't vomit at all). In the case of anticoagulant rodenticide toxicity, veterinary opinion on the matter of gastric lavaging seems to be divided. The poison is so easy to treat with medication that many vets don't feel a need to go to the added costs of putting the animal under a GA (general anesthetic) and manually washing out the poison from its stomach. Typically, these veterinarians tend to just make the animal vomit and then send it home on vitamin K1 medication. Many of the veterinary textbooks, on the other hand, do advise the lavaging of animals that have eaten anticoagulant rodenticide.
Before I started really researching in detail the information available on rodenticide toxicity in order to
write this page, I was formerly of the first opinion. Make the pet vomit in the clinic (get out that 60-70%
of the poison) and then send the animal home on antidote medication. This opinion on
rodenticide treatment was held by me for many reasons:
1) many of our clients were not particularly financial and could not easily afford the costs of a gastric lavage at an emergency centre (the price was around AU $1000 in 2006),
in addition to the high costs of vitamin K1 therapy, 2) the clinic I worked in was a very busy facility and, 'unnecessary' gastric lavages took up a lot of time and space and staff that we could not easily spare,
3) gastric lavages and general anaesthetics are not 100% innocuous and, therefore, were the risks
entailed worth it given that the toxin was easily medicated for and
4) the toxin was really easy to treat for and not usually life-threatening provided that the owner kept up with the vitamin K1 treatment.
The only animals that had eaten anticoagulant rodenticide poison that generally got lavaged were those patients where money was no issue for the owners and where the animal had failed to vomit
after being given the usual veterinary emetic remedies (it was very rare for us not to succeed in making a pet vomit, I must say).
Having read more on the matter, particularly with regard to the pharmacokinetics
of rodenticide toxicity (how long the poison remains in the body, how it gets excreted from the
body etc.), I have to admit that my veterinary opinion on the matter of gastric lavage has changed. Some of these anticoagulant poisons, particularly the second generation
rodenticides such as brodifacoum and bromadiolone, have huge half-lifes (i.e. time taken for half of the poison
to leave the body) and persist in the animal's body tissues for ages (sometimes well over 100 days). This long biological half life occurs because the second generation rodenticide poisons are tightly bound to the animal's body fats (i.e. instead of being rapidly excreted from the body via the urine and bile in the first few days, these
poisons distribute all over the body and imbed themselves in the animal's fat); they are tightly bound in the liver cells (they stay in the liver longer, thus affecting clotting
factor production longer); they are poorly broken down by the liver's drug-metabolism
enzymes; they bind to the vitamin K epoxide reductase enzyme for longer (i.e. inhibit
vitamin K1 reactivation for longer periods) and they undergo enterohepatic recycling (i.e. rodenticide that is excreted into the intestines via the bile gets reabsorbed by the intestine into the body again, instead of being lost in the feces).
The amount of poison that actually gets absorbed by the intestines in the first instance
(i.e. after consumption by animal) has a lot to do with this half life too. The more poison that is absorbed initially, the longer it is going to hang around in the body and impede the formation of effective clotting factors. Also, the more poison that is absorbed
initially, the greater the chances are of a toxic dose being absorbed by the animal and symptoms of
toxicity appearing if vitamin K1 is not provided. What this means is, although we vets do say that animals with second-generation rodenticide intoxication should be fine after 4-6 weeks
of vitamin K1 therapy, it is, in reality, theoretically possible for animals
that have eaten a massive amount of the poison to exhibit blood clotting defects requiring
vitamin K treatment well past this time. This has been proven in several cases of human poisoning (people deliberately trying to poison themselves with second generation baits), where vitamin K1 treatment needed to be given to the patient for many months before the person's clotting function was returned to normal.
On the matter of gastric lavaging of anticoagulant rodenticide patients, I now believe
that it is probably ideal to lavage the stomachs of all cases should the rodenticide have
been consumed by the animal within the last 3 hours. If finances are a huge concern
for the owner, I think you could still get away with not having to lavage an animal that ate a
first generation rat poison (the half life is hours, not days) because this poison type
is expected to clear from the body quickly, even after massive poison absorption (most likely, treatment will only require 1-2 weeks of vitamin K1). In the case of a second generation poison ingestion, I strongly advise stomach lavaging to reduce the amount of poison absorbed into the pet's body. Financially speaking, you could argue that the costs of lavaging the animal now may well save the owner the high costs of treating the animal with costly vitamin K1 for the full 4-6 weeks or even longer.
When not to lavage:
There is no point lavaging if the animal has eaten the rodent bait more than 4 hours ago
(note, some animals will still have bait in their stomachs for up to 6-8 hours after ingestion, however, 4 hours is the usual cut-off time used by most vets).
Do not lavage an animal that is showing symptoms of a bleeding tendency. By the time
clinical signs of anticoagulant rodenticide toxicity are seen, the bait has already
well and truly left the animal's stomach. Lavaging will also cause trauma that will exacerbate haemorrhaging.
Not all poison types can be removed by gastric lavage. With some poisons, e.g. extremely caustic and acidic poisons, it is even considered unsafe to lavage affected animals, just as it is considered unsafe to make these patients vomit.
Author's note: gastric lavaging is an effective technique for removing many poisons
from the stomach, particularly fine diameter, granular poisons such as pellets and grain meal. This technique may be less effective at removing much of the poison from an animal that has eaten a big meal recently (the chunks of food constantly block up the lavage tube) and it may not be particularly helpful at removing huge chunks of poison (e.g. large
wax blocks).
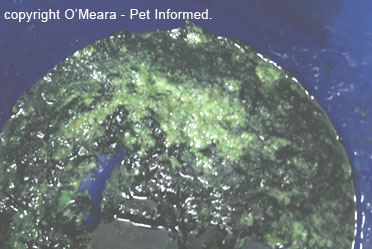
Image: green snailbait pellets coating the bottom of the collection bucket following a gastric lavage procedure. Better out than in. The same process can be used to remove rodent poison (rodenticide) from the stomach.
8d) Enemas:
Any poison that has been eaten tends to come out the back end eventually. Washing out the poison-containing
faeces from the rectum by manual enema not only reduces the chances of the rectal lining absorbing the poison back into the body, but manual emptying of the bowel also stimulates intestinal motility. Stimulating the intestines to move acts to push the poison along and out of the alimentary tract quicker.
This reduces the amount of time the poison remains in the intestines and, thus, lessens the time available over which the poison can be absorbed into the body. This results in less poison uptake into the body overall. Manual enemas are often performed
under a general anesthetic and are usually performed at the same time as the animal is having a gastric lavage


Images: This are images of a dog undergoing a manual enema to remove a poison (in this case it was
snailbait, but rodent poison would have looked very similar). The vet or nurse is washing the
rectum gently with warm water to make the bait-laden faeces come out. See how the poo on the wash trough grid contains green flecks - this are the pellets of snail bait (or rat bait)
coming out in the faeces. In the second image, the water coming out of the animal's rectum
is bright green: this is the dye used in the poison.
8e) Adsorbents and cathartics:
Once a pet has been made to vomit up the rodent poison and/or after it has undergone a gastric
lavage and enema, the veterinarian usually drenches the animal orally with an adsorbent product and a cathartic product.
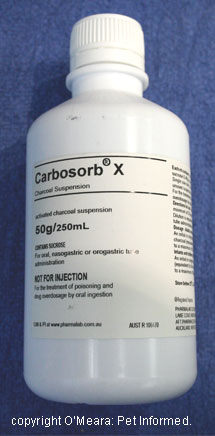 An adsorbent is a finely granular, high surface area product (normally given as a powder or liquid slurry or crushed tablet) that is designed to bind up any remaining poison in the animal's intestines and stomach and, thus, make that
poison unavailable for the intestines to absorb into the patient's body. Charcoal, available as a powder, slurry or tablet, is the adsorbent most commonly used by veterinarians.
An adsorbent is a finely granular, high surface area product (normally given as a powder or liquid slurry or crushed tablet) that is designed to bind up any remaining poison in the animal's intestines and stomach and, thus, make that
poison unavailable for the intestines to absorb into the patient's body. Charcoal, available as a powder, slurry or tablet, is the adsorbent most commonly used by veterinarians.
Charcoal is given to reduce the intestinal absorbtion of a poison. It is normally
administered after vomiting has been induced and following any gastric lavage and
enema procedure that is performed. A liquid slurry of charcoal is often put down the gastric lavage tube into the animal's stomach at the very end of the lavaging procedure, just prior to the animal
being allowed to wake up from the anaesthetic. In patients where the induction of vomiting and/or gastric lavage are not indicated or safe or in situations where too much time has passed for lavaging or emesis (vomiting) to be useful (i.e. between 4 and 12 hours after poison ingestion), charcoal can often be of use in reducing intestinal uptake of the poison. Charcoal tablets or powder slurries (crushed tablets or
powder mixed in water) can even be given at home by owners.
There have been lots of dose regimens suggested in the various texts:
1) Doses mentioned range from 0.5-8 grams of charcoal/kg of animal as a capsule or powder.
2) For slurries (water + charcoal mixtures), including commercially-available slurries, doses are around 10ml/kg.
3) Nelson and Couto (reference 18) are a lot more specific about the process they use. They mix
up a slurry of 1 gram of charcoal per 5ml of water and drench this mix at a dose rate
of 10ml of solution/kg of animal. The Veterinary Drug Handbook [ref 44] also recommends this dose rate for charcoal slurry.
The drench or tablet/capsule dose is repeated up to 4 times, every 4-6 hours. This repeated dosing is
especially important for picking up those poisons that undergo enterohepatic cycling (i.e.
poisons that get excreted into the intestine via the bile duct and then get reabsorbed
by the intestines again).
I find that animals are often quite accepting of charcoal slurries that are syringed into their mouths a bit at a time, provided this is done slowly (you don't want to blast charcoal
fluid into the back of a animal's throat too quickly).
Be aware that not all poisons are effectively bound up by charcoal. Poisons containing heavy metals (e.g. Iron EDTA) are unaffected (unbound) by charcoal administration, as are many others.

Image: This is a mixture of charcoal powder and water being poured into the gastric lavage tube's funnel at the end of a gastric lavage procedure.
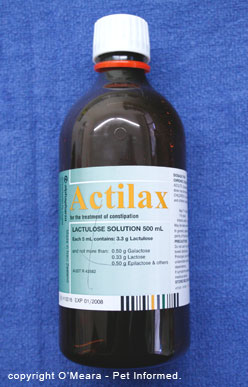 A cathartic is a substance that is designed to speed up the gastrointestinal transit time of the poison-containing intestinal contents. Put simply, a cathartic increases and stimulates intestinal motility. It stimulates
the intestines to move and push the intestinal contents, including any poisons, through more quickly so that there is less time available for the intestine to absorb
the poison into the body.
A cathartic is a substance that is designed to speed up the gastrointestinal transit time of the poison-containing intestinal contents. Put simply, a cathartic increases and stimulates intestinal motility. It stimulates
the intestines to move and push the intestinal contents, including any poisons, through more quickly so that there is less time available for the intestine to absorb
the poison into the body.
A number of cathartics are available:
Sorbitol
Sorbitol seems to be the most favoured of the veterinary cathartics. Some commercial
preparations of charcoal even contain sorbitol mixed into them for ease of use and, in
this way, adsorbent and cathartic are given to the patient at the same time.
When sorbitol is given separately to the charcoal, it is generally administered orally
at a dose of around 3ml/kg (70% sorbitol solution) [ref 11,45]. It is normally given 20-30 minutes after the charcoal has been given.
Sodium sulfate
If sorbitol is unavailable, the next most favoured cathartic is sodium sulfate or Glauber's salts. According to speakers at a recent vet conference (ICU Sydney 2008), a 40% solution of sodium sulfate can be administered orally, at a dose of 1g/kg, 30 minutes after the charcoal. Reference 45 states that sodium sulfate can be given at a rate of 1/2 teaspoon/kg, diluted in tepid water.
Lactulose (trade names include Duphalac, Actilax)
If both sorbitol and sodium sulfate are unavailable, then lactulose, a commonly-used
liver failure, hepatic encephalopathy and constipation-relief medication, can be given instead. Most clinics have access to lactulose.
Extra points on cathartic use:
Cathartics are not side-effect free and should always be administered under strict veterinary guidance and instruction. These are not at-home, self-medication drugs. Excessive use of cathartic drugs can lead to severe dehydration of the patient.
If the cathartic is to be given separately to the charcoal, most texts advise waiting
a little (around 20-30 minutes) before then administering the sorbitol or sodium sulfate or lactulose cathartic.
Cathartics should only be administered to the patient a single time. Repeated dosing of cathartics should be avoided because overuse can cause severe dehydration in an already potentially unwell animal. For this reason, commercially available charcoal/sorbitol mixed preparations should also only be used once and subsequent charcoal doses should comprise charcoal-only slurries (e.g. charcoal and water slurries).
8f) Prophylactic vitamin K1 (?)
There are two schools of thought on the treatment of animals with prophylactic (preventative)
vitamin K1 after the animal has been made to vomit, been given the lavage etc. The first advises
us to: "treat the animal with vitamin K1 anyway because this will definitely prevent any signs of bleeding from occurring if toxic poison levels have been absorbed." The second school
of thought suggests: "we have made the animal vomit and have gotten most of the poison out, so perhaps the animal has not managed to absorb a toxic dose. Let's just test the animal's PT time in 2, 3 and 5 days to see if it is prolonged and only treat the animal with vitamin K if it is."
My feeling is that both opinions and treatment plans are valid and are entirely dependent on the individual veterinarian and on the individual case at hand (e.g. how much rat poison came up?, does it look like all of the poison came out (e.g. a whole wax block)?, how long ago did the animal eat the poison bait?, has enough time passed for poison to be absorbed into the animal?, does the owner have financial concerns?, is the owner
likely to be reliable in getting PT testing done? and so on). I can make no comment as to which of the two options is the best plan because every case is different. The opinion
of your consulting veterinarian is your best guide.
Option 1 - Using vitamin K1 prophylactically:
Prophylactic vitamin K1 (phytomenadione) is generally administered twice daily to pets in the form
of oral tablets at doses that range from 1.0 - 2.5 mg/kg twice daily.
The dose and duration of vitamin K1 supplementation is often decided empirically by the vet, based on the active ingredient of the bait and also on how much was thought to have been eaten. For example, first generation rodenticides (warfarin, Fumarin, coumatetralyl, pindone etc.) are normally treated for only 1-2 weeks at lower vitamin K1 doses because of the short half-lives of these poisons and their poorer ability to bind to vitamin K1 epoxide reductase in the liver. The second
generation products (brodifacoum, bromadiolone, diphacinone and chlorophacinone), however, persist in the patient's body for ages and bind strongly to vitamin K1 epoxide reductase and, thus, they are normally treated with higher doses of vitamin K1 for 3-4 weeks and, often, up to 4-6 weeks.
Some veterinarians, regardless of the type of anticoagulant toxin eaten (first or second generation), will opt
for a treatment path that is somewhere between the two options. This is particularly the case if they think that poison absorbtion has been minimal. These clinicians will treat the animal with vitamin K1 for a week and then, at days 2,3 and 5 after the week's course has stopped, they will test to PT to see if any ongoing blood clotting disturbance remains. Ongoing treatment plans will depend on the test results. A prolonged
PT is indication to keep giving the vitamin K1.
My opinion is that, regardless of how long the course of vitamin K1 is given (1 week or 6 weeks), the animal should always have a PT test done at days 2, 3 and 5 after treatment has stopped,
just to be sure that the correct duration of vitamin K1 course has been administered.
Hints for good vitamin K1 administration:
Tablets are better absorbed if given crushed up in food.
Be watchful - make sure the animal actually eats all of its food and gets its full dose.
Vitamin K1 absorption is enhanced by giving the tablets with a fatty meal (note - be cautious in giving extra fat to animals that can not tolerate fatty meals such as dogs with pancreatitis, Schnauzers with hypertriglyceridemia, animals with diabetes, animals with Cushing's disease, animals with sensitive tummies).
The liquid injection preparations of Vitamin K1 can be given orally to animals that won't take tablets, but this is a much more costly way of doing it.
Do not give Vitamin K3 - this will not treat rodenticide poisoning.
Option 2 - Using the PT time to guide treatment:
Some vets, particularly if they suspect that very minimal absorption has occurred
or that only a tiny dose might have been eaten (e.g. a large dog that is thought to have eaten only
a couple of pellets), will opt not to treat with vitamin K1 and will, instead, opt
to monitor the animal's blood clotting parameters (especially the PT).
The best method of monitoring these parameters is for the animal to be taken to the vet on days 2, 3 and 5 after rodenticide consumption and for the PT time to be tested. The PT usually changes first (before aPTT and ACT do) and often will increase above the normal
range before any major bleeding problems are seen (plenty of time to start vitamin K1). Any prolongation of the PT is an indication that toxic levels of bait were consumed and that vitamin K1 therapy needs to start.
Even better, if the PT is taken on the day that the animal ate the rodenticide, this
result can be used as a baseline to tell the vet what that animal's normal PT should be. Thus, any trending upwards of the PT time (even before it gets to the level that is above the normal reference range)
may be an early indicator that toxicity is occurring.
I would tend to avoid using the ACT and aPTT to monitor an animal's clotting ability.
By the time problems are noticed in the ACT and aPTT, the animal has already lost its intrinsic, extrinsic and common pathways of blood clotting and is at high risk of having
a significant bleed.
Author's note: on a personal note, I tend to be a follower of option 1, mostly because I like to err on the side of caution. I'd rather spend a client's money on vitamin K1 treatment, perhaps unnecessarily, than have a patient bleed to death
from a cause that was so easily prevented (e.g. there is always a chance that an owner might
forget to return for the PT recheck at day 5). This is particularly the case if I suspect that any potential for extensive absorption has occurred or if the product eaten
was a second-generation product (remember, the dose that will cause
signs of toxicity is very low for second generation products such as brodifacoum, particularly
in the dog - the LD50 is only 0.25-1mg/kg in this species).

9) Treatment of clinical anti-coagulant rodenticide toxicity - the bleeding dog or cat:
9a) How to stop bleeding at home (e.g. bandaging, pressure).
Most cases of rodenticide toxicity present at home with problems that the owners of
the animal can not do an awful lot about, besides getting their pet to the nearest vet or emergency centre ASAP: coughing up blood, vomiting blood, collapsing on the floor,
having trouble breathing etc.
Sometimes, however, the first sign an owner will notice is that their pet will not stop
bleeding from an inflicted wound on the skin or mouth. In these situations, owners can attempt
to staunch the bleeding (whilst heading to their nearest clinic) by applying firm pressure to the wound with a towel or a handful of tissues or a shirt (anything available really). Pressing
firmly on a bleeding wound squashes the bleeding blood vessels closed, reducing the amount
of blood that is able to pass through the hole in the blood vessel and out of the animal.
Once firm pressure has been applied, owners should avoid the temptation to keep lifting up the pressure pad in order to see if the bleeding has stopped. With rodenticide toxicity and
many other bleeding disorders, the patient is unable to clot its blood and the blood will, thus, continue to flow every time the pressure on the blood vessel/s is relieved. Once pressure is placed, leave it there. The vet can have a look under the pad once the vet clinic
has been reached.
Animals that are bleeding from a lower limb or foot wound can be aided by placing a firm bandage
on the limb. Not too tight - you don't want to completely constrict the blood supply to the animal's foot -
just tight enough that a thick pad of swabs or tissues or towelling can be held against the wound with
moderate pressure.
Animals that are haemorrhaging from broken claws or excessively-trimmed nails can be helped
by dragging the end of the bleeding claw through a bar of soap (the thick soap will seal the bleeding end), or by painting over the bleeding end in nail polish to seal it. Pressure may work, but dogs and cats are
usually reluctant for pressure to be placed on a bleeding nail bed because these
areas are very painful and sensitive.
9b) PART 1: How we stop bleeding in the veterinary clinic - short-term manual and chemical techniques.
Vets have many techniques at their disposal for stopping or reducing bleeding in
pets. How and which of these techniques are administered or performed depends a lot on the individual
case and on the site and severity of the bleeding (e.g. animals in shock will not benefit
from a drug that drops their blood pressure further; animals with severe arterial bleeds
will not benefit from a dab of adrenaline and so on - it is all case and site
dependent).
Skin bleeds can generally be helped in one of four ways:
1) Pressure - just like at home, firm bandaging of a limb or foot may be enough to stop an animal from bleeding, particularly if the blood is coming from small, easily
compressed blood vessels.
2) Adrenaline - adrenaline is a drug that induces potent, local blood vessel constriction
in wound beds where it is applied. The constriction of the blood vessels supports the formation
of any clot that is trying to occur and reduces the amount of blood flowing past and through a hole in a blood vessel wall.
3) Drugs that reduce blood pressure - vets have access to some nice sedative drugs (e.g. acepromazine). These act to reduce an animal's blood pressure, thus reducing the amount and pressure of blood that is trying to flow through a hole in a blood vessel wall. These drugs are useful for bright, alert, hyperactive pets that just need calming down. They are also useful for some animals in respiratory distress
(animals that are finding it harder and harder to breath because they are panicking).
They should not be used on animals with any signs of shock (or likelihood of developing signs of shock) or anaemia or other medical issues (e.g. liver disease) precluding their use.
4) Clamping - large bleeds can sometimes only be stopped by placing a clamp (hemostat) over
the bleeding vessel to physically stop it from bleeding. In shocky, depressed animals, this procedure can be performed with the animal awake (they are not so responsive), but very alert, excited animals may need to have a strong sedation or a general anaesthetic to allow this to be done. Severely bleeding mouths and tongues often have to be clamped
if sedation alone does not work because it is very difficult to apply pressure and/or adrenaline to a tongue.
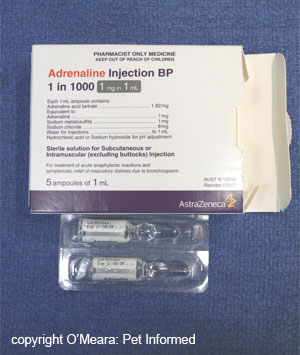
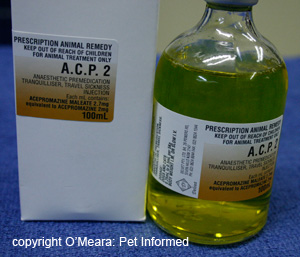
Image: adrenaline can be placed on bleeding wounds to induce local blood vessel
constriction and, thereby, reduce haemorrhage.
Image: Sedative drugs like acepromazine (ACP or ACE) can be used to reduce an excited animal's
blood pressure and thus reduce the pressure of the blood trying to haemorrhage out of
a wound site.
Nail bleeds:
Nail bleeds can generally be helped using some of the above methods - pressure, adrenaline, blood pressure drugs. They can also be stopped using cautery (a special hot iron
that burns and seals the blood vessels in the nail wound), various astringent powders and tissue glue (a special super glue that is used to seal wounds).
Internal bleeds:
Internal bleeds are much harder to control than external bleeds, particularly if the
animal does not have a good blood clotting system. Unlike a single torn abdominal
vessel in an otherwise normal animal, that can often be treated by supportive care and, in severe cases, by operating and finding and tying off that bleeding vessel, animals with blood clotting disorders are likely to bleed from multiple places, particularly if one tries to perform surgery on them! Needless to say, surgery on an animal with a bleeding disorder is not advised!
Pressure bandaging the abdomen:
Abdominal bleeding can be reduced or slowed by putting pressure on the abdomen: wrapping a
tight bandage (called a 'belly bandage') around the abdomen. This bandage stops the abdomen from expanding/distending further with blood loss and also acts to increase the pressure within the abdominal cavity, increasing the abdomen's resistance to further abdominal bleeding. The same technique can not be applied to
the chest (e.g. for thoracic bleeds) because the rigidity of the animal's rib cage does not allow for compression.
Methods like reducing the animal's blood pressure to stop bleeding can be used, however
there is a high risk that these animals may lose enough blood to go into shock. The
additional drug-induced drop in blood pressure might be dangerous for them. This is particularly the case for animals with lung, chest cavity, abdominal, retroperitoneal (around the kidneys)
and gastrointestinal bleeding (they can lose a lot of blood).
9b) PART 2: How to stop bleeding in the veterinary clinic - treating the coagulopathy.
Animals that are bleeding excessively due to rodenticide toxicity can be helped to stop
bleeding if their clotting factor levels return to normal. After all, their entire problem is
being caused by a lack of clotting factors II, VII, IX and X. Replace these factors and,
no matter where in the body the animal is bleeding (internal or external), the holes in
the blood vessel walls will clot and the bleeding will stop.
There are two main ways of replacing an animal's blood clotting factors:
1) Giving the animal plasma (see section 9e) and
2) Giving the animal vitamin K1 (see section 9c)
Plasma starts working as soon as it is administered. Vitamin K1 takes 8-12 hours to even start working because time is needed in order for the liver to start producing functional
clotting factors again.
9c) Vitamin K1.
 The use of vitamin K1 (doses, duration of treatment, ways of optimising absorption at home etc) has been thoroughly discussed in section 8f and much of the information provided in
that section pertains to this section also.
The use of vitamin K1 (doses, duration of treatment, ways of optimising absorption at home etc) has been thoroughly discussed in section 8f and much of the information provided in
that section pertains to this section also.
When an animal is first presented to a vet with clinical signs of rodenticide toxicity, the veterinarian
will often give that animal high doses of vitamin K1 (around 2.5mg/kg twice daily) for the first few days, regardless of the bait eaten (first or second generation anticoagulant bait), to load the animal's body up with vitamin K1 and enhance the production of clotting factors. Doses excessively higher than this are not considered to be any more effective and can, with excessive overdose, be detrimental to the animal's health (e.g. cats can develop Heinz body anaemia from overdose with vitamin K1).
The initial doses of vitamin K1 are normally administered by subcutaneous injection or by oral tablet. Intramuscular injections should be avoided because they can cause painful hematomas (severe bruises
in the muscles) and intravascular (e.g. intravenous) injections should be avoided because they can cause severe, even fatal, allergic reactions.
I have always tended to go with subcutaneous vitamin K1 injections (using a small needle to reduce the risk of needle-site bleeding) because of a belief that absorption of the vitamin would be enhanced and to reduce the risks of abrading the animal's oesophagus with harsh tablets (thus causing haemorrhage). Several texts, however, state that oral absorption of vitamin K is as good as, if not better than, injectable treatment and
that the injectable, liquid vitamin K1 preparations can be administered orally to good effect. Thus, both routes of administration (oral and subcutaneous injection) should be considered to be valid options. The latter (oral route) would certainly pose no risk
of causing severe injection site hemorrhage.
I would still avoid oral vitamin K1 in animals that are vomiting (they might not get
their full dose) or that are passing blood in the vomit or stools (their intestines
may be ulcerated and unable to absorb the vitamin properly). Animals with chronic intestinal
digestion problems (e.g. EPI, IBD, biliary disease, liver disease) may also be better off if treated initially with injections.
The effect of vitamin K1 is not instantaneous. It takes 8-12 hours for the PT to start to improve
after administration and up to 12-48 hours for it to normalise. Bleeding may still occur within this lag period.
Once the animal has recovered, regained its normal blood clotting function and is at the point whereby it is safe to send home, it will normally go home on oral vitamin K1 tablets
(or syrup). Vitamin K1 tablets are generally administered twice daily to pets in the form
of oral tablets or syrup at doses that range from 1-2.5 mg/kg twice daily.
The dose and duration of vitamin K1 supplementation is often decided empirically by the vet, based on the active ingredient of the bait and also on how much was thought to have been eaten. For example, clinical cases of first generation rodenticide toxicity are normally treated for 1-2 weeks. Higher doses are usually given for the first few days to 'load the animal up' with vitamin K1 (as mentioned above), but
these doses can generally be tapered down into the lower levels (e.g. 1mg/kg twice daily)
once the animal's blood is clotting normally. In contrast, the second
generation products (brodifacoum, bromadiolone, diphacinone and chlorophacinone), persist in the patient's body for ages and bind strongly to vitamin K1 epoxide reductase. These cases are normally treated with vitamin K1 at higher doses (e.g. 2.5mg/kg twice daily)
for 3-4 weeks and, often, up to 4-6 weeks.
Upon finishing the course of vitamin K1, regardless of how long the course of vitamin K1
has been (1 week or 6 weeks), the animal should always have a PT test done at days 2,3 and 5 after treatment has stopped, to be sure that the correct duration of course has been administered.
Hints for good vitamin K1 administration:
Tablets are better absorbed if given crushed up in food.
Be watchful - make sure the animal actually eats all of its food and gets its full dose.
Vitamin K1 absorption is enhanced by giving the tablets with a fatty meal (note - be cautious with animals that can not tolerate fatty meals such as dogs with
pancreatitis, diabetes, Cushing's disease, Schnauzers with hypertriglyceridaemia and animals with sensitive tummies).
The liquid injection preparations can be given orally to animals that won't take tablets, but this is a much more costly way of doing it.
Do not give Vitamin K3 - this will not treat rodenticide poisoning.
9d) Intravenous Fluid Support.
Animals that develop severe haemorrhage, whether it be internal (into their body cavities) or
external (bleeding into their faeces or vomit or out of their skin), can often experience
a severe drop in their blood pressure. Basically, there is simply not enough blood volume
present within the animal's blood vessels, after severe hemorrhage, to maintain adequate blood pressure and deliver adequate oxygen and nutrient supplies to all
of the tissues of the animal's entire body.
The body initially responds to this acute drop in blood pressure by sacrificing the non-vital regions of the body. The blood vessels supplying non-essential regions of the body
such as the limbs, skin and gastrointestinal tract (termed peripheral tissues), constrict, greatly reducing the blood supply to these organs. This sacrificing of the peripheral tissues acts to redirect the remainder of the animal's blood to the very important organs of the body: the kidneys, heart, liver and brain. The aim of this is to keep these vital tissues alive until the animal is able to regain its normal blood volume (e.g. through the reabsorption of blood from internal sites of bleeding) and the sacrificed tissues are once again able to be permitted their rightful and much needed blood supply.
It is this drop in blood pressure and restriction of blood flow to the animal's peripheral tissues that causes the signs of shock seen in these patients. The animal's extremities are cold and pale (because they are getting less blood); the animal's rectal temperature drops
(because less warm blood is reaching the rectum from the body's core); the animal is
depressed (less blood pressure is reaching its brain) and the animal has a very rapid heart rate (when blood pressure falls, the heart is made to work harder and beat faster in an attempt to improve the animal's blood pressure).
The trouble with this mechanism, designed to save the vital organs whilst sacrificing those
of lesser importance, is that it is not able to save the animal if blood loss is too severe
(a loss of greater than 20% of an animal's blood volume is likely to result in death) and nor
is it able to last forever. If something isn't done quickly to restore the animal's circulating blood volume and normal blood pressures, the animal will rapidly begin to decompensate
and head towards death. For example: the intestine, starved of oxygen and blood for many hours, will start to degenerate, allowing nasty intestinal bacteria to access the bloodstream
where their toxins will cause signs of severe septic shock and death. The kidneys, starved of blood pressure, will start to degenerate, leading to acute renal failure. In addition to this, eventually the constricted peripheral blood vessels of the body will become exhausted and be forced to relax their muscles and widen once again, resulting in an acute, catastrophic drop in the animal's blood pressures and death.
The basic thing to understand from all of this is that severe blood loss, low blood pressures and signs of shock, if left untreated for too long, will eventually result in the death of the animal because its own mechanisms of staying alive (blood vessel constriction, increased heart rates etc.) may not be enough to save it.
The most readily-available means that we veterinarians have of restoring an animal's blood
volume and thus its blood pressure is by the administration of intravenous fluids (i.e. a drip).
There are many types of fluids that can be given by the intravenous route, the main ones being:
crystalloids (basic fluids such as saline), colloids, plasma and blood.
1) Intravenous Fluids: crystalloids.
Animals with severe signs of shock are often initially placed onto a high-flow-rate (shock-rate) intravenous drip containing fluids such as 0.9% saline or Hartmann's solution. In appearance, these fluids look like water, however, they are very salty and they contain no cells or
large molecules. They are termed crystalloids. They are administered to animals for many
reasons including: to restore a shocked animal's blood volume and blood pressure
rapidly; to provide intravenous water to animals with moderate to severe dehydration or haemorrhage
and to restore an animal's blood salts (electrolytes), if they are out of balance.
Author's note: sometimes, animals come into the vet that are so shocky and collapsed, with such severely low blood pressures (severe shock signs), the veterinarian can't get an intravenous drip into the animal's leg veins. The blood vessels in the patient's legs have shrivelled down to such tiny, thin tubes that no intravenous catheter will thread up them. In these cases, the vet will sometimes be forced to insert a catheter into the pet's jugular (the large vein in the neck) or insert a needle into the bone marrow of the animal's thigh (femur) or upper arm (humerus) to administer the fluids. Don't be alarmed to see your vet do this: it looks brutal, but these techniques are perfectly acceptable ways of giving lifesaving fluids to animals in severe shock.
In the case of an animal that is bleeding from rodenticide toxicity, intravenous crystalloid fluids are
useful for their ability to initially boost that animal's blood volume and blood pressure, however, these fluids are not the only type of fluids that you would want to rely on in these patients. Only giving an animal with rodenticide toxicity water-based fluids is not ideal for several reasons:
A) The fluid will dilute out the animal's remaining platelets and clotting factors even more, resulting
in worsening bleeding tendencies
B) The fluid will dilute out the animal's blood protein levels, especially the albumin (protein is lost from the body when an animal haemorrhages). See the next section on
colloids for more about the importance of albumin in these patients.
C) The crystalloid fluids do nothing to treat the animal's bleeding disorder and
D) The crystalloid fluids do not replace important things that the bleeding animal
is losing, such as platelets and red blood cells and blood protein (esp. albumin).
2) Special intravenous fluids - colloids:
Animals with severe bleeding (especially external bleeding) can lose massive
amounts of blood cells and blood proteins (blood contains lots of protein) from
their blood circulation. Over a matter of hours to days, these losses can accumulate, resulting in a massive drop in the animal's overall blood protein levels, a deficit that is further exacerbated should the animal then be given large volumes of crystalloid fluids that act to dilute out the blood proteins further.
When dogs and cats lose excessive amounts of protein through severe, acute bleeding or through
more chronic, longer-term bleeding, their overall blood protein levels can plummet. Of particular importance is a protein called albumin. Severe drops in blood albumin levels can have severe repercussions for the animal's health, body-functions and survival. Albumin has a large number of essential functions within the body,
one of the most important being the maintenance of colloid-oncotic pressure (COP). Colloid-oncotic pressure (COP) is a force that is exerted by the charged particles (e.g. blood salts) and heavy molecules (e.g. albumin) that drift in the bloodstream, which acts to keep
the watery fluid part of the blood (the plasma) within the blood vessels. Without this COP force
(e.g. if albumin protein levels become critically low as a result of haemorrhage), the blood's fluid will leak out of the blood vessels, resulting in a severe drop in the animal's blood pressure (i.e. not enough blood for the organs) and the infiltration of watery fluid into areas of the body where it is not wanted (e.g. into the lung and the brain!)
When albumin is lost during severe bleeding and/or overly-diluted through excessive crystalloid administration, there is a risk of the animal's colloid-oncotic pressure falling to dangerously low levels (i.e. and for fluid to then start leaking out of the vessel walls). Veterinarians manage and treat this situation by either:
1) giving the patient special, synthetic, intravenous fluids, which contain heavy molecules that mimic the COP
effects of albumin (these special fluids are termed colloids) or
2) by replacing the lost albumin with real albumin by giving the patient a plasma transfusion (see next point - 9e).
Colloids can also be indicated for pets that come in to the vet clinic with severe signs of shock and low blood pressure, regardless of their blood protein levels. Because colloids act to rapidly increase the colloid oncotic pressure inside the animal's blood vessels, they can act to draw fluid into the animal's blood vessels from other areas of its body, thereby boosting the animal's blood pressures rapidly whilst the animal is being properly and concurrently hydrated with other fluids. They are a really good way of rapidly improving an
animal's status for the short term when an animal presents to a vet in severe hypovolemic
shock (shock that occurs because an animal doesn't have enough blood volume).
In the case of an animal that is bleeding from rodenticide toxicity, intravenous colloids are
very useful for their ability to initially boost an animal's blood pressure rapidly, however, as with the crystalloids, they are not the only type of intravenous fluid that you would want to rely on in these patients. Only giving an animal with rodenticide toxicity colloid fluids would not be ideal for several reasons:
A) The colloid fluid will dilute out the animal's platelets and blood clotting factors even more, resulting
in worsening bleeding tendencies
B) Colloids are contraindicated in animals with very low platelet numbers because they can reduce platelet activity (they affect the 'stickiness' and plug-forming ability of platelets). Although animals with blood clotting factor disorders such as rodenticide toxicity initially do have normal platelet numbers, once the animal starts bleeding, the platelet levels in the body will fall secondarily, as a result of the platelets trying in vain to plug the bleeding holes in the absence of any clotting factors and a stabilising blood clot. Colloids will act to make any platelet efforts less effective.
C) The colloid fluid will dilute out the animal's blood protein levels, particularly albumin. Although the colloids will replace the albumin's COP effect, they can not replace the other functions and roles of natural blood albumin (e.g. drug and hormone transport).
D) The colloid fluids do nothing to treat the bleeding disorder and
E) The colloid fluids do not replace important things that the bleeding animal
is losing, such as platelets and red blood cells.
Colloids are great products, but they don't come without risks. They are artificial synthetic substances and, as
such, they have the potential to cause allergic and anaphylactic reactions in patients
given them. Colloids also have the potential to instigate bleeding problems in animals that have low blood platelet levels and they can sometimes cause an animal's blood pressure to become too high, which greatly adds to an animal's bleeding risks if
there are only weak platelet plugs attempting to block holes in the blood vessels.
9e) Special intravenous fluids - plasma:
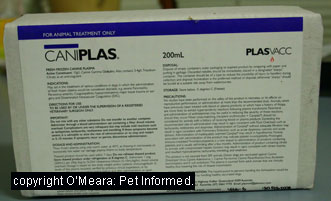 Plasma is the fluid that remains when you remove all of the cells from blood. It contains
many helpful substances and properties that can really make a huge difference to the survival chances of rodenticide affected pets. It is the first choice intravenous fluid for treating animals with rodenticide toxicity which haven't yet lost enough blood cells
to require a blood transfusion (see section 9f).
Plasma is the fluid that remains when you remove all of the cells from blood. It contains
many helpful substances and properties that can really make a huge difference to the survival chances of rodenticide affected pets. It is the first choice intravenous fluid for treating animals with rodenticide toxicity which haven't yet lost enough blood cells
to require a blood transfusion (see section 9f).
Helpful properties of plasma include:
1) Clotting factors II, VII, IX and X - these clotting factors remain stable in frozen plasma and can be administered, via plasma infusion, to rodenticide affected animals in order to clot and stop any bleeding which is actively occurring. By replacing the factors that the rodenticide-affected liver is unable to make, plasma transfusions are able
to provide the right factors to complete the blood clotting cascade and thus, clot the blood. This effect begins as soon as the plasma transfusion starts to be given (i.e. it is able to
start work whilst the vitamin K1 is taking effect).
2) albumin - as mentioned before, albumin is responsible for maintaining colloid oncotic pressure within the bloodstream of animals so that their blood vessels
don't start leaking. Albumin is also responsible for many other functions within
the body, including the transport of certain hormones, antibiotics and therapeutic drugs through
the bloodstream. Plasma contains albumin.
3) Ability to restore blood pressure - like colloids and crystalloids, plasma is a fluid that contains a lot of water and fluid volume. It can be administered to shocky animals to boost their circulating blood volume, just as the crystalloids and colloids can. Because it contains albumin (which acts to increase COP), plasma is more closely related to the colloids than to the crystalloids. Like a colloid, plasma is able to rapidly draw fluid into the patient's blood vessels from other areas of its body, thereby boosting the animal's blood pressure rapidly whilst the animal is being properly and concurrently hydrated with other fluids. It is a really good way of rapidly improving an animal's cardiovascular status for the short term when a rodenticide-affected animal presents to a vet in severe hypovolemic
shock (shock that occurs because an animal doesn't have enough blood volume).
Author's note: a lot of plasma (many bags of it) needs to be given to a large dog
to generate any noticeable shift in its overall protein and albumin levels. Several bags over several hours may also need to be given to restore and maintain the animal's normal blood clotting ability whilst the vitamin K1 is starting to have its effect on the liver's ability to make its own clotting factors (this can take over 12 hours). The need for
repeat transfusions over time may be necessary because the clotting factors given through plasma transfusions are used up quickly by an actively bleeding animal. This can get expensive.
Cautions: Also note that plasma, like the synthetic colloids, is not without risk. It is a
proteinaceous substance being given intravenously. Consequently, there is the possibility that a plasma transfusion could cause allergic or anaphylactic reactions in some patients,
particularly if the patient in question has received plasma, blood or tick or snakebite antiserum
previously.
9f) Special intravenous fluids - blood:
 Some patients lose so much blood as a result of rodenticide toxicity haemorrhage that they
can actually become severely anemic (i.e. they don't have enough red blood cells left in their body) in addition to losing blood volume and dropping in blood pressure. The role of these red blood
cells is to transport oxygen around the animal's body. Animals that do not have enough
red blood cells (anemic animals) are unable to supply oxygen to all of their tissues and, as a result, the tissues, particularly the highly-oxygen-dependent tissues such as the brain, kidney
and heart, can start to become damaged and die, resulting in the death of the animal.
Some patients lose so much blood as a result of rodenticide toxicity haemorrhage that they
can actually become severely anemic (i.e. they don't have enough red blood cells left in their body) in addition to losing blood volume and dropping in blood pressure. The role of these red blood
cells is to transport oxygen around the animal's body. Animals that do not have enough
red blood cells (anemic animals) are unable to supply oxygen to all of their tissues and, as a result, the tissues, particularly the highly-oxygen-dependent tissues such as the brain, kidney
and heart, can start to become damaged and die, resulting in the death of the animal.
Red blood cells can be replaced by giving the patient a blood transfusion. Blood is normally
available for transfusion in two forms: packed red blood cells and whole red blood cells.
A third form, auto-transfusion is also possible.
Packed red blood cells are highly-concentrated bags of red blood cells that are created by removing most the plasma (fluid portion of the blood) from around the blood cells and only
placing the blood cells and a much smaller amount of plasma into the transfusion bag. Packed cell
transfusions are able to deliver large numbers of red blood cells to the patient in a much smaller volume of blood (this is because you are not giving the patient as much of the non-cellular fluid portion of the blood). Packed cell transfusions are especially useful when the patient has a condition that results in a loss of red blood cells, but no loss of plasma or fluid from the body (e.g. animals with diseases that specifically
target and destroy the red blood cells without harming or depleting the animal's blood plasma - e.g. IMHA - immune-mediated hemolytic anemia, onion poisoning). Packed cells do not provide
the patient with living platelets nor with much plasma or plasma-contents (e.g. clotting factors and albumin).
Whole blood is blood that is taken freshly from a donor animal and which contains all of the blood cells, proteins and plasma contents of a normal animal's blood. It is the best form of blood transfusion for an animal with severe internal or external haemorrhage
because it replaces exactly what the animal has lost: red cells, protein, plasma and platelets.
It does contain some clotting factors (though not as much as frozen or fresh plasma) and can help with
blood clotting restoration in rodenticide patients.
Auto-transfusion is where the animal's own haemorrhaged blood is removed from a large site of internal bleeding (e.g. removed
from the chest cavity or abdominal cavity) and retransfused back into the animal. i.e. you are draining out haemorrhaged blood and putting it back into the patient's own blood vessels. It is a solution of last resort (i.e. you desperately need to put blood back into the animal's veins, but have no donor animal or packed cells) and should only be used when you are absolutely certain that the bleeding has not been caused by cancer (otherwise there is the risk of transfusing cancer cells into the animal's bloodstream). It is risky to drain blood out of an animal's chest or abdomen when the animal has a blood clotting issue because the act of inserting a needle into the animal's chest or belly can initiate further bleeding.
Caution: Please note that blood transfusions, like synthetic colloids and plasma, are not without risk. Blood is a proteinaceous substance being given intravenously. Consequently, there is the possibility that a blood transfusion could cause severe (even fatal) allergic or anaphylactic reactions in some patients (particularly cats), particularly if the animal
in question has received plasma, blood or tick or snakebite antiserum previously.
Generally, most dogs can receive a first blood transfusion from any canine donor without
the need for cross-matching of blood. Subsequent transfusions can also be given
without cross-matching, provided they are given within 36-48 hours of the first one. Cross-matching is required for any blood transfusion given 48 hours or more after the first transfusion.
Cats must be blood typed before any blood transfusion, even the first one. Cats have very specific
blood types (A and B and AB) and must only receive blood of the correct type. In an emergency (i.e. if a cat donor can not be found), a one-off transfusion of canine
blood can be given to a cat. It is risky though.
9g) Therapeutic draining of blood?
Sometimes an animal can bleed into an area of the body so severely, that the sheer presence of
all that fluid in the body cavity causes severe discomfort or disability to the animal. The four main areas of the body that come to mind are major bleeds into the abdomen, chest cavity, pericardial sac (sac around the heart) and the small space between the skull and brain (e.g. subdural hematoma).
The abdomen:
Major bleeding into the abdominal cavity can be very uncomfortable for the animal. The belly balloons
out to a massive size and the animal finds it painful to move, lie down and breath. The pressure exerted by that fluid on the animal's diaphragm may make it difficult for that
patient to breathe normally.
The chest cavity:
Major bleeding into the chest cavity is a very dangerous situation for the animal. The fluid (blood) between the rib cage and the lungs compresses the lungs, making them unable to expand with air. This is not just distressing: animals with severe lung collapse can even die from an inability to draw enough oxygen into their lungs. Thus, the draining of fluid from the chest cavity is not only therapeutic and aimed at improving the
animal's comfort levels, it can often save the animal's life.
The pericardial sac:
Major bleeding into the pericardial sac is also a life-threatening situation for the
animal. The chambers of the heart, compressed by blood in the outer sac, are unable to pump blood around the animal's body properly and this can lead to severe shock and organ damage from a lack of normal blood flow.
The skull cavity:
Major bleeding into the space between the skull and the brain is extremely problematic
and life-threatening for the patient. The blood presses on the brain, causing symptoms
of increased cranial pressure and brain disturbance (seizures, rigidity, coma). If bleeding
pressure increases to a certain, critical point, the brain can sometimes herniate
out of the back of the skull, resulting in the death of the patient.
When faced with these kinds of life-threatening situations, the veterinarian may have to manually drain blood from the animal's chest, heart sac, abdomen or skull cavity in order to save that animal's life and/or relieve its severe discomfort. This is not without considerable risk. It is never ideal to stick a large needle
or catheter into the chest or abdomen of an animal with a clotting abnormality because there is always the risk of making the animal's bleeding worse (the animal may bleed and bleed from
the needle stick). It is possible to cause severe bleeding that may worsen the animal's condition
and clinical presentation. At the same time, not doing anything may also result in the animal's death.
This goes doubly so for patients with haemorrhage inside the skull cavity. There is massive
risk entailed in drilling a hole into an animal's skull in order to relieve the pressure
on its brain.
Aside from drainage of the pericardial sac and skull cavity (where we aim to remove as much of the blood as possible), we do not aim to remove all of the blood from the chest or abdominal cavity. With the chest and abdomen, we only aim to take as much fluid out as is needed to resolve the animal's discomfort and breathing difficulties. The reason is that, any blood left inside the animal will eventually be reabsorbed by that animal back into
its bloodstream. Leaving some hemorrhage fluid behind will eventually be of use to the patient because the animal will auto-transfuse that blood back into itself, thereby resolving its anaemia and hypotension (low blood pressure).
9h) Tips on feeding and diet:
There is nothing too special about the diet that we feed an animal with rodenticide
poisoning aside from a couple of key points.
Animals with bleeding disorders should be feed a very soft, non-abrasive food (e.g. no kibble or bones) until their blood clotting has normalised. Feeding abrasive, hard foods
to an animal with a blood clotting defect can be life-threatening. Bones that pierce the gums or tongue and hard biscuits that abrade the throat and oesophagus can lead to haemorrhage and this can end up life-threatening to an animal that can not clot its blood.
Animals with bleeding disorders are best fed a diet high in protein and iron content
(e.g. fresh mince products, high protein prescription canned pet foods) to replace the iron and protein that is lost through hemorrhage. Please note, however, that this recommendation depends very much on the cause of the bleeding disorder. High protein and iron diets may be contraindicated in some conditions (e.g. animals with renal disease). Talk to your vet about it.
Animals with anticoagulant rodenticide poisoning, regardless of whether the animal is bleeding or not, should be given their vitamin K1 tablets crushed into a fatty meal. Fat in
the meal greatly increases the uptake of vitamin K1 into the animal's body. Note, however, that owners with pets who are prone to intestinal and pancreatic disorders (e.g. pancreatitis)
exacerbated by high fat content in their food, should not change their pet's diet to something fat-filled. Fatty diets or sudden changes in diet can exacerbate nasty intestinal and pancreatic conditions such as pancreatitis and inflammatory bowel disease and upset metabolic diseases such as diabetes, hypertriglyceridaemia and Cushing's disease
(Hyperadrenocorticism). Again, ask your vet if you are unsure.

Prevention of Rodenticide Poisoning:
I have divided the prevention of rodenticide toxicity into two separate sections. The first section (section 10) provides you with tips on preventing mouse, rat and rodent infestation and some lethal and non-lethal alternatives to the use of rodent poisons in and around your home. Avoiding the use of poisons in and around the home altogether is by far the best way of preventing a pet from becoming inadvertently primarily or secondarily poisoned with any form of rodenticide. The second section (section 11) is tailored towards the less-than-ideal situation: how to make poison use as safe as possible
when the use of poisons is simply unavoidable. We understand that sometimes the reality of rodent management is such that poisons do need to be used and that it is often impractical for us veterinarians just to say, "don't put out the poisons".

10) Tips on mouse and rat control without pet-toxic rodenticides:
The very best way to prevent pets from becoming poisoned by rodenticides is by not laying poisons out in and around your property at all. There are many
rodent control and prevention techniques and many rodent-killing or rodent-capturing products now available that do not pose a risk to pets and children in your family. These methods can all be used in combination with each other for maximum rodent control and are as follows:
10a) Making your property less attractive to rodents looking for a home.
Obviously, it is far easier to control a rodent problem before it actually begins than it is to try to remove a rodent problem that is already well established in your home
or shed or yard. Animals, including rodents, need certain home comforts to be provided
before they will establish themselves in an area and breed. They need shelter, warmth, bedding, food and, in the case of rats, a fresh water supply (mice will drink water if
it is available, but will often get enough hydration out of the food they eat). Preventing mice and rats from gaining access to these essential things will prevent them from setting up a population in your premises and thus negate the need for poisoning or the placement of other rodent removal products. The following is a list of tips and hints for preventing
mice and rats from setting up in your premises (this list is not exhaustive: think about what mice
and rats need in order to survive and breed and then use your imagination to find ways to deprive them of these necessities):
Rodent-proof your house and shed:
Mice and rats love to nest in the ceilings, floor spaces and wall spaces of houses. Human
houses are a rich source of warmth, soft bedding and nesting material (e.g. insulation material, mattress stuffing, couch stuffing), food and water - everything a mouse or rat could ever want. Making sure that these animals can not physically get into your house in the
first place will go a long way towards preventing a rodent problem from developing.
Small cracks under walls, between roofing tiles, between house bricks and in ceilings and roof eaves should be found and sealed. Plastic seals (skirts) can be affixed to the bottoms of doors to prevent rodents from
squeezing under them. Broken window panes and fly screens should be replaced. Don't forget to
check water pipes, sewage pipes and hot water systems - rodents can enter a house via sinks
(e.g. kitchen and bathroom sinks) and toilets. Basically, any
hole larger than the diameter of a pencil can admit a mouse: you need to go over your house from
top to bottom looking for such holes in the walls, floors and roof and take steps
to seal them up and stop rodents from getting in.
Non-removable fillers, such as concrete or plaster reinforced with copper mesh, can be used to
plug up the holes. Any rodent holes found can be filled with copper wire mesh and cemented or plastered over.
The same principles of rodent-proofing (sealing roofs and filling in spaces under walls and floors etc.) could theoretically be applied to food and grain storage sheds too, however a lot more effort is required to keep mice and rats out of these places through building design alone - they are very attractive to rodents.
Clean up after yourself:
Leaving food and crumbs out on bench tops and floors will convince mice and rats that your
place is a good place to stay. Make sure that food scraps are not allowed to gather underneath the oven
and fridge (you might not see them, but mice and rats love them). Similarly, leaving dirty plates and cooking utensils in the sink overnight will also provide such pests with a nice nightly meal stop. Mice and rats will not linger if there is nothing to feed on after hours.
Make sure that all dry food is placed in rodent-proof, sealed containers:
Storing biscuits, cereals, rice, pasta and seed-matter in boxes and plastic bags is asking mice to dinner. These animals have a great sense of smell and can easily detect the food items stored inside such packaging. They have an even better set of teeth!
They will nibble holes in boxes and plastic packaging (usually at the back where you can't see it)
to get at rice, noodles, cereals and other such foody things. Placing cereals and biscuits etc. into sealed, airtight plastic, ceramic or stainless steel containers makes it very difficult for mice and rats to access your food. They won't stay around.
If you have aviaries, make sure that they are mouseproof:
Aviaries and chookyards are a huge issue when it comes to attracting mice and rats
to your home. Mice and rats dine out on fallen seed and will nest in bird boxes
and hollow logs that you have set up for your birds. Design your
aviaries and chookyards so that mice and rats can not get in to access seed and bedding. Mice will tunnel through floors made of dirt - floors made of concrete or wire mesh are better.
They will squeeze through holes in aviary wire that are large enough to admit them - make sure that
your aviary wire is very fine gauge (the holes should ideally be less than a pencil width in diameter), even
if the birds are big). Mice and rats will easily chew through fabrics such as tarp and shade cloth - avoid making walls out of these materials.
Make sure that bird feeders are placed in the middle of the aviary so that fallen seed does not fall outside of the aviary for the mice and rats. Any seed that does spill outside of the
aviary should be cleaned up often and whenever it is noticed.
Avoid leaving food out for wild animals and birds:
Everyone loves bird houses and leaving bowls of seed and bread and the like out for wild animal visitors. Unfortunately, mice and rats also love your generosity and, like
the wild birds and squirrels that you are trying to attract, they will hang around so long
as you keep the food available for them.
Animal feeds (e.g. bird seed, horse and livestock feed) should be placed in
rodent-proof, sealed containers:
Similar to the situation with human foods, mice and rats are very attracted to the grains and cereals
used to feed birds and livestock. These foods should be placed in sealed food-bins made of stainless steel or heavy-duty plastic that the mice and rats can't access. Never leave grains or pellets in the canvas-type bags that they normally come in because mice and rats will chew holes in these.
Do not leave dirty dog and cat food bowls out for rodents to access:
Dog and cat foods are attractive to mice and rats and other rodents. Bowls with pet food
residues should not be left out after the pet has eaten. Bowls should be washed after
each use so that food residues do not remain to attract rodent pests (and ants).
In a similar fashion, feed bins used to feed horses and livestock should also be emptied and
cleaned after each use. Left over grains and chaff in feed bins are an excellent source of
nutrition for hungry rodents.
Seal up compost heaps:
Compost heaps with their vegetable offcuts should be kept in sealed compost bins. Mice and rats find compost heaps an excellent source of food matter and the warm, fermenting vegetable matter and soft soil in and around the compost heap makes a nice home for mice and rats to dig a hole, build a nest and rear their young.
Reduce unnecessary garden clutter:
Keeping your yard and gardens as bare as possible (i.e. with minimal leaf clutter and litter) can also help to reduce mice and rat activity because such prey animals do not like to have to run across a lot of open ground in order to move from place to place.
Making sure that your yard and shed do not contain excessive clutter also reduces
the availability of places that mice and rats can nest in. Mice and rats will nest in
fallen logs, woodpiles, abandoned car bodies and old furniture (mattresses, couches). They will take full advantage of badly stored boxes (e.g. boxes full of old toys) and
piles of paper (e.g. old stacked newspapers). Get rid of these cluttering things if you do not have a need for them, or store them out of reach of rodents.
10b) Natural mouse and rat repellants:
There are a number of natural, home-made and commercially-available remedies around designed to repel mice and rats and discourage them from setting up homes on your property. Some of these solutions that I have listed come from anecdotal testimonies of people who have tried them and liked them. I can not vouch for any of these products or techniques personally, not having used them myself, but I have listed those that seem to be logical and I consider them to be worth a try as part of a combination, pet-safe, rodent-prevention strategy. At the very least, most of them are inexpensive and worth a go (if they don't work, they haven't cost you much).
Please note that this not an exhaustive, all-inclusive list: plenty of "better mouse repellants" and "this works" anecdotes will always keep coming onto the market
so long as there are rats and mice in the world to repel.
Predators:
Mice and rats generally will not set up homes and populations in areas where there is a large number of predators actively hunting them. Non-venomous rodent-eating snakes such as pythons can be allowed to have free range in sheds and outdoor areas (so long as your guests are aware of it!) My family used to have a large monitor lizard (a goanna type animal) that regularly entered our roof space chasing after
mice (it probably would have been better if we'd just sealed up the large holes that the goanna
and thus the mice were entering through, but there you have it). Encouraging other predators
such as owls and hawks and other birds of prey to take up residence around your house (e.g. providing them with large trees to nest in etc.) can also reduce your rodent problem.
Cats and certain breeds of dogs (especially terrier types) can become excellent ratters
and mousers, particularly if you keep their body-weight normal to slightly underweight and do not offer them ad libitum pet food to eat (animals that are overfed do not bother themselves with catching rodents). Be aware, however, that allowing pets to hunt mice and rats does pose a risk to them and
to you as the owner. Rats and mice carry horrible bacterial and viral diseases in their
bites, which might be passed on to your pet, and the urine from rodents often carries
Leptospirosis: a nasty, potentially fatal, kidney- and liver-affecting bacteria, which your
pet can catch and pass on to you. Also, many of the parasites that affect dogs and cats (e.g. Spirometra tapeworms) can be caught through the consumption of rodent prey. For all of these reasons, I am not a big advocate of using domestic pets as mouse traps, however, a lot of people are and so I have mentioned it here for you.
Plants:
Certain plants with strong, noxious (to rodents) odors and/or bitter tastes are thought to repel mice and rats and can be planted in garden beds to stop mice and rats from setting up nesting sites in soil, tree trunks and compost heaps. For the imaginative
among you, borders of such plants may even be planted around aviaries and houses and other
places to try to dissuade mice and rats from entering. Plants to consider include:
Mint - this can be planted in the garden as fresh, whole plants or scattered as dried leaves
throughout attics and sheds and other places where rodents are unwanted.
Holly leaves - dried holly can be scattered throughout attics and sheds and other places where rodents are unwanted.
Bulbed plants of the Narcissus group of plants (e.g. jonquils, daffodils) - these plants contain noxious alkaloids that may repel mice and rats, but be careful with their placement as
they are also poisonous to pets that decide to eat them.
Lavender - again, this can be planted in the garden as fresh, whole plants or scattered as dried leaves
and flowers throughout attics and sheds and other places where rodents are unwanted.
Plants of the family Scilla (e.g. squill and wood hyacinth) - these plants may repel mice and rats and some species even contain a toxin that has been used commercially in the production of the rodenticide: Red Squill. Be careful with their placement as the plants in this group are also poisonous to pets that decide to eat them.
Catnip, also called Cat Mint.
Plants of the family Euphorbia, commonly referred to as "spurges" (e.g. poinsettia) - these plants may repel mice and rats and many of them make pretty garden plants. Be careful with their placement as the plants in this group are also poisonous to pets that might choose to eat them.
Plants of the family Sambucus, commonly referred to as elder or elderberry plants.
Camphor plants otherwise known as camphor laurel - this plant contains a pungent chemical called camphor that repels rodents and insects and which is, additionally, one of the main ingredients in commercial mothballs. The same effect can be achieved by using mothballs (only ever use camphor mothballs though because
the naphthalene mothballs are highly toxic and carcinogenic and illegal in many countries).
Plants of the family Allium - this is a group of bulbed plants that contains such commonly
grown and eaten garden plants as onions, shallots, leeks, garlic and chives. Their oniony
smell repels rodents and other vermin. Be careful with their placement as the plants in this
group are also poisonous to pets that might eat them (e.g. onion toxicity in dogs and cats).



Image: The catmint (catnip) plant. Cats love it, but rodents hate it.
Image: Poinsettia is a pretty garden plant that may repel rodent pests.
Image: Onions have a noxious smell that rats and mice dislike and keep away from.
Common household products that may repel rodents:
Aside from plants, there are other pungent-smelling products commonly available in most households that can be applied to rodent-attractive surfaces and compost heaps in order to repel unwanted rodents and dissuade them from nesting.
Black and red pepper can be mixed into food scraps destined for the compost heap in order to reduce their attractiveness to ravaging mice and rats.
Tabasco sauce, wasabi and other highly-spicy products such as chili powder and chili paste
can also be applied to the bases of plants and to compost and soil that you don't want rodents to nest in. These substances can be applied to surfaces (e.g. wood panels, electrical cord casing and plastic piping) that mice and rats have been found to be gnawing on in order to discourage this gnawing activity. Hot spices have long been a technique used to stop dogs and cats from chewing hoses and eating their own droppings and may well have the same repellant effect on mice and rats.
Mothballs - similar to the effect described with the planting of camphor-containing plants
(e.g. camphor laurels), mothballs containing camphor may also be used to deter mice and rats. Be careful with their placement because mothballs may be poisonous to pets that eat them. They
should never be placed near food or plants intended for human consumption.
Cat litter - soiled cat litter can be scattered in areas where rodents have shown signs of activity and
added to gardens and compost to repel mice and rats. The smell of feline urine and faeces
convinces the rodents that there are many predators around and they vacate the region.
Pet fur - the fur of dogs and cats can also be scattered in areas where rodents have shown signs of activity and added to gardens and compost heaps to repel mice and rats. As with the faeces and urine, the rodents think that there are predators around and vacate the region.
Ammonia is another smell that can deter mice and rats from establishing in households. Ammonia is one substance that gives dog and cat urine much of its smell and using it
as a rodent deterrent is similar to the effect of putting predator urine around the place (only a lot cleaner). Ammonia can be wiped onto surfaces or soaked into old rags and left in areas that mice and rats are not wanted. The smell should keep them away.
Note, however, that ammonia is a noxious, irritant substance that releases irritant gasses. It should be used in well ventilated areas that humans don't spend much time in.
Commercial rodent repellant products:
Several products have been brought onto the market that are designed to repel rodents and
discourage them from setting up homes in your premises. These include the following:
Ropel - Ropel is a non-toxic, bitter-tasting, pest repellant that is designed for outdoor use. It can be applied to the outside of houses, trees, garden plants (not ones destined to be eaten by people), wooden posts and other surfaces to prevent mice and other vermin from chewing them and nesting in them. It is not toxic to pets and may last for up to a year with one application.
Shake-Away Rodent Powder - "Shake-Away" is the name given to a range of products that contain bobcat and/or fox urine mixed into a powder-like carrier substance. The powder is sprinkled around bird feeders, aviaries and the inside and outside of buildings and the smell of the urine contained in the powder suggests to rats and mice that there are predators about. This reduces their willingness to
nest and breed in 'powdered' premises. I haven't used the product myself, but the idea
behind it certainly has merit. A recent (2008) Australian study in Tasmania found that dingo urine sprayed around new trees greatly reduced the amount of damage caused to those trees by the dingo's natural prey, the kangaroo. It may offer a humane alternative to poisoning in Tasmanian regrowth projects.
Ultrasonic rodent repellers (e.g. PestChaser® Electronic Rodent Repeller) -
Ultrasonic rodent repellers are auditory assault products, designed to emit frequencies of sound that are above the range of hearing for humans and domestic pet animals (not pet rodents though). These repellers are audible to rats and mice and the sound that they admit is persistent enough, loud enough and noxious enough to these animals that it will force them to move away from your home and not set up an infestation in your house. That's the theory anyway.
Opinions on the effectiveness of these products are varied and probably dependent upon
the ultrasound repeller brand itself and also on what can realistically be expected from the units by consumers. Ultrasound beams do not go through walls, ceilings or floors and nor
do they bend around corners. Consequently, if house owners only place a low number of repeller units in their house (e.g. in just a couple of rooms) this can result in the mice and rats avoiding the places where the units have been placed and continuing to live and breed in the acoustically shadowed regions (places where the ultrasonic beam does not reach). Of course, mice and rats forced to move about in the acoustically shadowed regions of the house may then be more likely to
stumble upon other rodent traps and poisons if these are placed in those acoustic shadows (hence a multi-pronged approach to rodent control is always best). For best results, a large number of ultrasonic repeller units need to be purchased and placed around the house
(e.g. one in each room, several to cover a very large room, several to cover a room that is not shaped in a simple, square or rectangular shape). Mice and rats may also become accustomed
to the noise of the unit if it remains at the one, constant pitch or is not emitted (pulsed) at high intervals.
One would expect a product to be more annoying to rodents and less adapted to by them if it alternates its pitch regularly (e.g. the PestChaser alternates its sound frequency through 32-62kHz) and emits its sound with maximum regularity (for example, according to the PestChaser
website, some repeller units only emit a noise once every few seconds, whereas the better units
emit their noises many times per second - this is more annoying to rodents).
10c) Non-chemical, commercial, lethal mouse and rat control products.
There is a huge range of mouse and rat control 'appliances' available on the consumer market
these days, all aimed at being "the better mousetrap". Some of these products are considered humane (e.g. flip traps) and some of them are considered inhumane (some are even condemned
by certain animal welfare organizations because they cause the vermin animal to die slowly).
Note that the definition of a "humane trap" varies from organization to organisation
and person to person. Some people and groups consider any trap that kills an animal
to be, by definition, inhumane. Other people and groups consider certain lethal traps
(e.g. snap traps and electronic rodent killers) to be humane so long as they kill the
animal swiftly. All of the traps listed in this section (10c) are lethal traps (the description
of each trap includes information about whether they are considered humane or not according to "rapid-kill" criteria). Non-lethal humane traps are discussed in section 10d.
Snap traps (e.g. spring-loaded snap traps and jawed "T-Rex" type traps):
There are many types and brands of "snap trap" available on the market for the control of both mice and rats. Most of these traps operate on the principle of a spring-loaded bar or "jaw" that slams down over the rodent's neck or mid back when a food-baited trigger or switch is disturbed by the hungry animal. The rodent dies almost instantly from a broken back or neck or crushed skull.
Although these traps are considered inhumane by some people because they are designed to
kill rodents, not capture them, their rapid speed of kill, when they do work as
planned, does make them one of the more humane rodent killing devices available. The major drawback to these traps from an animal welfare perspective is that they can sometimes meet with a timid or oddly-postured mouse or rat, resulting in that animal being
caught alive (and painfully) by a tail or leg or lower body. Animals caught in this way
will die slowly and painfully if the trap is misplaced or not regularly checked on and animals discovered alive will have to undergo the added stress and pain of the trap's
owner trying to dispose of them. (My advice, should you happen to find a live, injured
mouse or rat in a trap, is to take the animal and trap to a vet or shelter for humane euthanasia - drowning the poor thing or whacking it on the floor is not kind.)
The main problem with snap traps from a practical rodent control perspective is that they are not really efficient or effective at controlling large mouse and rat infestations. One reason for this is that you can only capture one mouse or rat at a time. Another reason is that rodents will often discover what they are and learn to avoid them
(they will learn this lesson quickly if they see a trap go off and take out another rat or mouse or if a trap happens to go off close by them).
For best effects, large numbers of snap traps should be set up, unloaded, with their lures in place for a week or two before arming them (setting the spring). This allows the mice and rats to get used to these new additions to their territory and to happily trust them and move about on them. This lack of "trap shyness" will increase the number of rodents killed when the traps are finally set. One reference even suggests rubbing
tasty-smelling food oils over your hands (e.g. oil of anise, bacon grease) before
handling the traps so that the smell of "human" doesn't put the rodents off going near them.
When the time comes to set the traps, set all of the traps at one time. Good food lures for mice and rats include: pumpkin seeds, bacon, peanut butter, dried fruit and cheese (I personally find bacon or peanut butter to be very good lures).
Traps should, ideally, be placed in "rodent thoroughfares": places and paths where mice and rats travel. You can scatter talcum powder in rodent frequented areas to detect the direction
and path that they travel in (follow the trail of powder). Trails of faeces and urine
can also give you an idea where and in which direction they travel. Traps should be placed against walls, in corners and darkened, narrow gaps of rooms, because mice and rats rarely run out into the open spaces of rooms. Be aware of trap placement: bacon and
other smelly foods may attract household pets who could set them off and/or become injured by the traps
(especially the big rat traps - ouch!).
Snaps traps must be checked twice daily to ensure that any live-catches are not left to suffer.
Important safety note: The urine of rodents contains many nasty diseases
that are infectious to people (e.g. Leptospirosis). When disposing of mice and rats caught in traps, be sure to wear disposable gloves, goggles and a facemask when handling the traps so that aerosols from the animal's urine can not contaminate your hands, eyes or respiratory passages.
Some diseases (e.g. Hantavirus, Lassafever, Haemorrhagic Fever) can be caught by breathing in dust that is contaminated with rodent droppings and urine. When placing traps in enclosed, poorly-ventilated, dusty sites such as sheds, attics and floor spaces, wear gloves, goggles and a face mask to avoid dust exposure.
Sticky Traps or glue traps:
These traps basically comprise of thick, non-drying glue spread thickly on a rigid piece of cardboard or
wooden board. Mice and rats run onto them, get stuck in the glue and then die from
starvation or from drowning in the glue. These traps are considered to be quite cruel and
many welfare organisations do not recommend them.
If you are using these traps, better results are experienced if the traps are placed in
non-dusty regions of your shed or house (dust coats the glue, making it non-sticky), in places that are nice and dry and not prone to excessive moisture (wet mice don't stick). Food lures can be placed in the very centre of the glue board to encourage mice and rats to walk onto the glue. These traps are better suited towards reducing a mouse problem than a rat problem
because some rats are strong enough to extricate themselves from the glue.
Important safety note: The urine of rodents contains many nasty diseases
that are infectious to people (e.g. Leptospirosis). When disposing of mice and rats caught in traps, be sure to wear disposable gloves, goggles and a facemask when handling the traps so that aerosols from the animal's urine can not contaminate your hands, eyes or respiratory passages.
Some diseases (e.g. Hantavirus, Lassafever, Haemorrhagic Fever) can be caught by breathing in dust that is contaminated with rodent droppings and urine. When placing traps in enclosed, poorly-ventilated, dusty sites such as sheds, attics and floor spaces, wear gloves, goggles and a face mask to avoid dust exposure.
Electronic rodent killers (e.g. Electronic Rat Trap by Victor):
A range of electronic rodent killers have been invented that work by electrocuting
mice and rats. The mouse or rat runs through the trap, which is normally shaped like a tunnel, and, as it does so, its body completes an electric circuit. An electric current surges through the animal, killing it instantly.
I have no personal experience with these devices, however, if they do work as quickly and effectively as they claim to, then this is probably a very acceptable, humane
means of killing rodent pests.
Best results are probably expected if these devices are used and placed in a manner
similar to snap traps: place many around, let the rodents get accustomed to them for a few weeks before arming them, use appropriate lures, place them in areas of the house
where mice and rats travel (rodent pathways) etc.
Important safety note: The urine of rodents contains many nasty diseases
that are infectious to people (e.g. Leptospirosis). When disposing of mice and rats caught in traps, be sure to wear disposable gloves, goggles and a facemask when handling the traps so that aerosols from the animal's urine can not contaminate your hands, eyes or respiratory passages.
Some diseases (e.g. Hantavirus, Lassafever, Haemorrhagic Fever) can be caught by breathing in dust that is contaminated with rodent droppings and urine. When placing traps in enclosed, poorly-ventilated, dusty sites such as sheds, attics and floor spaces, wear gloves, goggles and a face mask to avoid dust exposure.
10d) Non-lethal, humane rat and mouse catching alternatives.
I have put the non-lethal, humane mouse and rat traps (catchers) in a separate section to the other commercial
products because a lot of people are specifically looking for these products and information
about them. Many animal lovers favour these traps over most of the other rodent control options
mentioned so far because they do allow rodent animals to be caught alive and non-painfully. This
thereby gives the trap's owners the choice of releasing the captured animal/s somewhere else, far from their property, or having them humanely euthanased at a vet.
Please be aware that releasing mice and rats elsewhere, although it sounds on the face of it to be the nicest thing to do, may well create a problem for someone else who didn't have a previous rodent problem. Also be aware that releasing such rodents into forests and reserves can be devastating to native wild animal populations (most rats and mice are feral and, in most countries, they are a major, overpopulated pest which can devastate wild bird populations and displace native mammals). Humane euthanasia of feral, pest rodent species is, in my opinion, the best option for dealing with these creatures
if you have captured them in humane, live-capture traps.
Important legal note: In some places it may actually be illegal to use live traps because
releasing the mice and rats just moves the vermin problem on. You need to check with your
local council what the rules are before using these traps.
Flip traps:
Flip traps are traps that operate by rapidly 'flipping' a mouse or rat into an interior
compartment of the trap without actually killing the animal. They are excellent
products because, not only do they usually not hurt the animals (note, occasionally animals will die or become injured after being caught the wrong way in the flipping mechanism), but they also reset
automatically, allowing a number of rodents to be captured by the one trap. The smell of the
other mice or rats within the trap is thought to even encourage new mice and rats to investigate the
traps and become caught.
Again, as with the snap traps, best rodent capture results are likely to be achieved if these traps are used and placed similarly to the snap traps: e.g. place many traps around, let the mice and rats become accustomed to them for a few weeks before activating them, use good lures, place the traps in places where mice and rats regularly travel (rodent pathways) etc.
Important safety note: The Centre for Disease Control in the USA does not advocate
the use of live traps for rodent control. These traps scare the rodents caught within them and scared
rodents are apt urinate in them. The urine of pest rodents contains many nasty diseases
that are infectious to people (e.g. Leptospirosis). When disposing of mice and rats caught in traps, be sure to wear disposable gloves, goggles and a facemask when handling the traps so that aerosols from the animal's urine can not contaminate your hands, eyes or respiratory passages.
Some diseases (e.g. Hantavirus, Lassafever, Haemorrhagic Fever) can be caught by breathing in dust that is contaminated with rodent droppings and urine. When placing traps in enclosed, poorly-ventilated, dusty sites such as sheds, attics and floor spaces, wear gloves, goggles and a face mask to avoid dust exposure.
Important legal note: In some places it may be illegal to use live traps because
releasing the mice and rats just moves the vermin problem on. You need to check with your
local council what the rules are before using these traps.
Names of some of the humane, live-capture products available (this not an exhaustive list):
Trapper 24/7 Humane Mouse Trap
Repeater or Tin Cat Clear Top
Corner Cat Multiple Mouse Trap
JT Eatons Wind-Up Mouse Trap
Mouse Master
Protecta MC
Ranger # T231 Rat/Squirrel/Small Rodent Live Trap
Havahart traps
Multi Mouse Humane Mouse Trap
Big Cheese - Trip Trap
Live Capture Multi Catch Humane Mouse Trap
Automatic Humane Mouse Trap
Live Animal Cage Trap - for larger rodents such as squirrels.
10e) Natrocell's EradiBait: An alternative, safe pellet rodenticide?
Natrocell has brought out a rodenticide that is, according to trials and company data, both effective as a rodenticide and non-toxic to domestic pets or people. The rodenticide, called EradiBait and also known by the names
of EradiMouse and EradiRat, is based on a natural plant extract and is biodegradable with minimal risks of environmental contamination or secondary poisoning. It works by interfering with the rodent's ability to absorb water via its intestines: the rodent
animal dies after 2-5 days from dehydration.
According to the company, it is "safe to use around birds, fish, pets, farm animals and humans when used as instructed." The pellets are also quoted as being "safe to use when used as instructed, even around human foodstuffs - such as in restaurants, hotels, food factories etc. Due to their specific mode of action there is minimal risk of non-target poisoning of other species ..." Note, however, that even though the product is safe
to use around pets, it should still be protected from non-target animals. After all, if your pet animals eat all the bait, what will the rats and mice get to eat?.
The rodenticide is intended for use as an alternative feed source by mice and rats
(the product works best when mice and rats consume it regularly over a period of days, gradually
depriving them of water uptake) and, therefore, works best when other sources of food are removed from the rodents (i.e. you need to remove alternative food sources, such as open bins, spilled foods and unlocked compost heaps to get the best effect). Alternative food sources (baits) should not be used as lures to attract rodents to the EradiBait.
Like most rodenticides, Eradibait works best when placed in dry areas (moisture ruins it) where rodent activity is known to be high. Good places include: places with visible rodent droppings, rat thoroughfares, building access points, rodent nesting sites and burrows, rodent watering holes, mouse holes, places close to livestock feed stores and aviaries (note, effectiveness may be reduced in places like feed stores
due to the abundance of alternative food sources) and sheltered places like attics, the underneath of porches and the backs of pantries.
Author's note: The product certainly sounds good. I have no personal experience with the use of this product, however, if it does act as effectively as the company claims it does, then this kind of product
may potentially be a big future player in the rodenticide marketplace. The claims of pet safety have to be a big plus with regard to the veterinary world.

11) Prevention of rodenticide toxicity - when you are using baits:
Section 10 was a discussion of useful alternative rodent control methods
that might be used instead of poisonous rodent baits or used concurrently with them to reduce the amount of such pet-unfriendly toxins placed by householders. This section (section 11), gives useful suggestions and tips for reducing the likelihood of pet poisoning by rodent baits in situations where poison use is deemed to be unavoidable (e.g. large and persistent rodent populations).
11a) Choice of bait:
Use anticoagulant rodenticides:
The anticoagulant rodenticides are certainly not safe baits as this page will attest to, but they are infinitely safer than many of the other baits used to kill rodents (cholecalciferol, strychnine, 1080, thallium, zinc phosphide). This is because poisoned animals are easy to diagnose
and there is at least an antidote that can be used with reliability in cases of poison
ingestion. If EradiBait by Natrocell is as safe and effective as the manufacturers say it is (and it certainly sounds as though it might be), and it is available in your area, then I would choose this bait over all of the others, including the anticoagulant rodenticides.
Use only first generation anticoagulant rodenticides:
If warfarin resistance (first generation anticoagulant resistance) is not a known issue in your parts or if the rodent problem you have is only small, I would advise putting down only first generation rodenticides (warfarin, coumatetralyl, Fumarin).
These will not cause secondary pet poisoning, contaminate the environment with long-lasting poison residues, accumulate in native, wild animal predators or need to be treated with the vitamin K1 antidote for anywhere near as long, should your pet or child become poisoned.
Use only wax blocks:
Wax blocks are easier to tie down (anchor down) in areas that are out of the reach of pets, whereas
small pellets can always spill and scatter across a wide area. Pellets are more likely to be carried around by rodents, making it more likely for poison pellets to end up in your pet's environment. Pellets, when ingested by pets, have a very large surface area: this greatly speeds
up the rate and amount of absorption of the poison into the animal's body should the pellets be inadvertently eaten. Wax blocks, on the other hand, have a lower surface area and digest much less readily: rapid induction of vomiting may potentially result in the entire block being brought up by the animal and, therefore, much less risk of large volume toxin absorption.
Use baits with a taste deterrent such as Biterex (Bitrex):
Although taste deterrents may not stop all pets from eating poison baits (I've never seen a
labrador deterred from anything edible), it may well stop more finicky pets such as cats and small dogs (and children) from eating misplaced baits and thus save their lives. Just remember that, even if a poison product does have a taste deterrent, some pets will still go ahead and consume the poison. Thus the placement of baits and choice of rodenticide active ingredient are still vitally important.
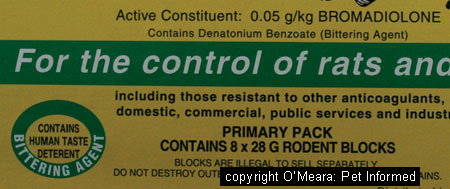
Image: Always look for labels that say the rodenticide has a taste deterrent.
11b) Placing baits:
Place the bait well out of reach of pets:
Baits should never be left at ground level, even if "out of reach" under a cupboard
or house, because pets are very imaginative and skillful when it comes to getting at them. Baits need to be placed well out of reach in ceilings, underneath pet-inaccessible floor spaces, in wall spaces and other such places where pets can not reach them. Inside and on top of cupboards and drawers is not enough - I have seen pets scale cupboards to reach baits perched on top of them.
Use tamper-proof bait stations:
Many brands of rodenticide now come with a specially-designed box or case that they can be placed or tied into, called a bait station. All rodenticides should be placed into a bait station
to reduce the chances of pets having easy access to them. As an added bonus, bait stations also promote rodent uptake of the poison too, because the vermin animals get to consume the poison
whilst hidden inside a darkened box, which is far more comforting for them (rodents don't feel safe eating baits placed out in the open).
If you have pets or kids around then the best bait stations to use are those that
are "Tamper-proof". This means that kids and pets who are determined to get into them
can not. Steel bait stations are probably better than plastic ones in the case of
pets because many large dogs will try to chew through items with a plastic covering
and may potentially access the bait through destruction of the station. Baits placed into
bait stations should ideally be in wax or block form as pellets may potentially be shaken
out of the stations by vigorous pets.
Tie baits down:
If using wax blocks and no bait station, make sure that the waxy baits are physically tied down with wire or non-chewable material so that mice and rats can not carry the baits away from where they have been placed. Mice and rats may
carry away baits that are not anchored down, potentially taking them within reach of
your pet. Be sure to check the bait blocks regularly, ensuring that the baits are still intact enough to remain safely tied in place.
Never place baits under the house:
Baits placed under the house are often forgotten and this can lead to poisoning of
pets when a new pet (one able to get under the house) is bought or when a new family comes to live at the house, bringing their pets with them.
When moving to a new house, you should always ask the previous owners or tenants whether they have put any baits down.
If you go to someone else's house with your pet, you should also think to ask them if they have any
poisons laid down that might be toxic to your pet.
Remove baits after use:
Once the baits have had their effect and you deem rodent numbers to be removed or
radically reduced, remove the baits and throw them away. This will reduce the risk of
baits being forgotten and found by pets later on.
11c) Avoiding secondary toxicity.
There are several things that can be done to avoid secondary toxicity of pets
when poisons are being used.
Use only first generation anticoagulant rodenticides:
These poisons do not tend to accumulate in vermin to toxic levels and thus they pose less risk of
secondary poisoning should a dog or cat consume poison-killed rodents. Other rodenticide
products such as cholecalciferol and zinc phosphide do not cause secondary toxicity either, however I would avoid their use because of the risk of primary pet poisoning.
Don't allow cats and dogs to catch and eat rodents when poisons are in use:
When baits are in active use, cats and dogs should be kept inside so that they are unable to hunt and eat sickly rodents that come out into the open looking for water.
Basket muzzles (see point 10d) can be placed onto the faces of outdoor dogs to reduce their ability to catch and consume rodent vermin.
Remove any rodent carcasses you find and dispose of them out of reach of pets:
This is pretty self explanatory. If you pick up all of the carcasses that you find, then there won't
be as many around for pets to find and eat. Make sure that you wear gloves when handling dead
rodents.
Keep cats and dogs well fed (this does not mean fat) and occupied:
Well fed and occupied (not bored) cats and dogs are unlikely to hunt for mice and rats or
feel a need to eat rodent carcasses. This reduces the risks of secondary poisoning.
Don't allow dogs and cats to consume the offal of deceased wild animals or livestock:
Never allow your pets to snack on the innards of any deceased wild animal or livestock animal that you find. You don't know what it died of! The animal could have died from a poison that your pet
might become secondarily affected by or it could have died from some horrible infectious
disease or carry a parasite that might infect your pet.
If you hunt game, do not feed your pet the offal of the animals that you kill. These organs
can contain poison residue build-up (which might poison your pet) if strategic poisoning has been
occurring in that reserve.
Always keep your pet on a lead when walking it in public areas or animal reserves. This
will prevent your pet from running off and consuming dead animals or animal baits (e.g. 1080 baits)
when you aren't looking.
11d) Extra tips regarding dogs that keep on getting access to ratbait.
I have not seen too many cats that keep on getting into ratbait supplies: most cases of
repeated rodenticide poisoning in cats are likely to be a result of secondary toxicity and the consumption of poisoned rodents. I have, however, seen many cases of repeated rodenticide poisoning in dogs, particularly farm dogs where extensive poison use is utilized to protect grain and hay stores.
In addition to the tips mentioned in previous sections, you can also consider the following
options for preventing dogs from becoming repeatedly poisoned:
Basket muzzles:
A basket muzzle is a loosely-fitting, mesh-like muzzle that fits over the face of the dog. It allows the dog to drink water and to open its mouth and pant and thus cool down, but it does
not allow the animal to consume anything (e.g. rat poison). A lot of people place these muzzles
on dogs to stop them from chewing all sorts of things, including: poisons, plants,
reticulation and rocks and also to stop them from attacking other dogs, domestic pets,
livestock and children. They are a useful means of stopping dogs from eating poisons.
Safety: I would never advise leaving a muzzle on a dog that was completely unsupervised. Muzzles can get caught in objects or on fences and potentially lead to choking. They are fine to use when the owner is at home and able to check up on the dog. When the owner
is away, the muzzle should be off and the animal placed in a confined yard or dog run
with no chance of accessing baited areas.


Image 1: This is a basket muzzle as viewed from the side.
Image 2: This is a basket muzzle viewed from above.
Prophylactic vitamin K1 therapy?
Some owners I know have such trouble stopping their pets from getting access to anticoagulant rodenticides that they regularly dose their pets with low doses of vitamin K1 to keep their levels up in case of poison consumption.
Are there issues with vitamin K toxicity if it is used in this way?
Although Vitamin K1 poisoning is rare, this substance is a fat soluble vitamin and, as such, can
be expected to be stored and recycled within the body for long periods of time. Extreme levels may, therefore, potentially be associated with vitamin K poisoning. I would
only ever advise that prophylactic vitamin K1 be given under strict veterinary assistance
and guidance (this way, monitoring for signs of toxicity can be done).
According to one reference, the phylloquinone form of vitamin K (called vitamin K1)
has not been associated with signs of toxicity, even at massive doses. The drug
phytomenadione used in veterinary medicine is a synonym of phylloquinone and, thus, should theoretically have a high safety margin for use if used in a low-dose, prophylactic
capacity in dogs. Cats can get Heinz body anaemia with overuse of vitamin K1. Again, seek veterinary advice if considering using vitamin K1 in dogs or cats.
The drug, menadione, (also known as vitamin K3) has been found to have toxic
side effects such as hemolytic anaemia (rupture of the red blood cells) in dogs, Heinz body anaemia in cats and jaundice when used at 2-3x or more above the recommended doses. Menadione is banned in some countries and is no longer recommended for use.
11e) Natrocell's EradiBait: An alternative, safe pellet rodenticide?
Natrocell has brought out a rodenticide that is, according to trials and company data, both effective as a rodenticide and non-toxic to domestic pets or people. The rodenticide, called EradiBait and also known by the names
of EradiMouse and EradiRat, is based on a natural plant extract and is biodegradable with minimal risks of environmental contamination or secondary poisoning. It works by interfering with the rodent's ability to absorb water via its intestines: the rodent
animal dies after 2-5 days from dehydration.
According to the company, it is "safe to use around birds, fish, pets, farm animals and humans when used as instructed." The pellets are also quoted as being "safe to use when used as instructed, even around human foodstuffs - such as in restaurants, hotels, food factories etc. Due to their specific mode of action there is minimal risk of non-target poisoning of other species ..." Note, however, that even though the product is safe
to use around pets, it should still be protected from non-target animals. After all, if your pet animals eat all the bait, what will the rats and mice get to eat?.
The rodenticide is intended for use as an alternative feed source by mice and rats
(the product works best when mice and rats consume it regularly over a period of days, gradually
depriving them of water uptake) and, therefore, works best when other sources of food are removed from the rodents (i.e. you need to remove alternative food sources, such as open bins, spilled foods and unlocked compost heaps to get the best effect). Alternative food sources (baits) should not be used as lures to attract rodents to the EradiBait.
Like most rodenticides, Eradibait works best when placed in dry areas (moisture ruins it) where rodent activity is known to be high. Good places include: places with visible rodent droppings, rat thoroughfares, building access points, rodent nesting sites and burrows, rodent watering holes, mouse holes, places close to livestock feed stores and aviaries (note, effectiveness may be reduced in places like feed stores
due to the abundance of alternative food sources) and sheltered places like attics, the underneath of porches and the backs of pantries.
Author's note: The product certainly sounds good. I have no personal experience with the use of this product, however, if it does act as effectively as the company claims it does, then this kind of product
may potentially be a big future player in the rodenticide marketplace. The claims of pet safety have to be a big plus with regard to the veterinary world.

To go from this rodent poison page to the home page, click here.

References and Suggested Readings:
1) Gross KL, Wedekind KJ, Cowell CS et al. Nutrients. In Hand MS, Novotny BJ, editors: Pocket Companion
to Small Animal Clinical Nutrition, 4th ed. Topeka, 2002, Mark Morris Institute.
2) Raffe MR, Wingfield W, Hemorrhage and Hypovolemia. In Raffe MR, Wingfield W, editors: The Veterinary
ICU Book, USA, 2002, Teton Newmedia.
3) Green MT, Transfusion Medicine. In Raffe MR, Wingfield W, editors: The Veterinary
ICU Book, USA, 2002, Teton Newmedia.
4) Henson MS, Smith SA, Disorders of Hemostasis. In Raffe MR, Wingfield W, editors: The Veterinary
ICU Book, USA, 2002, Teton Newmedia.
5) walters JM, Rodenticides. In Raffe MR, Wingfield W, editors: The Veterinary
ICU Book, USA, 2002, Teton Newmedia.
6) Quesnel AD, Parent JMThe Cat with Seizures, Circling and/or Changed Behaviour. In Rand J, editor: Problem-based Feline Medicine, Sydney, 2006, Elsevier Saunders.
7) Abrams-Ogg A, The Bleeding Cat. In Rand J, editor: Problem-based Feline Medicine, Sydney, 2006, Elsevier Saunders.
8) Brooks M, Coagulopathies and Thrombosis. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
9) Cote E, Over-the-counter Pharmaceuticals. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
10) Nicholson SS, Toxicology. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
11) Haldane S, Update on Toxicology. In ICU in Sydney: The Critical Patient - PGF Proceedings 370, Sydney, 2008, Post Graduate Foundation in Veterinary Science.
12) Hatch RC,Poisons Causing Respiratory Insufficiency. In Booth NH, Mc Donald LE, editors: Veterinary Pharmacology and Therapeutics, 5th ed. Iowa, 1988, Iowa State University Press.
13) Hatch RC,Introduction to Veterinary Toxicology. In Booth NH, Mc Donald LE, editors: Veterinary Pharmacology and Therapeutics, 5th ed. Iowa, 1988, Iowa State University Press.
14) Hatch RC,Poisons Causing Nervous System Stimulation or Depression. In Booth NH, Mc Donald LE, editors: Veterinary Pharmacology and Therapeutics, 5th ed. Iowa, 1988, Iowa State University Press.
15) Hatch RC,Poisons Causing Abdominal Distress or Liver or Kidney Damage. In Booth NH, Mc Donald LE, editors: Veterinary Pharmacology and Therapeutics, 5th ed. Iowa, 1988, Iowa State University Press.
16) Hemostasis and Blood Coagulation. In Guyton AC, Hall JE, editors: Textbook of Medical Physiology, 9th ed. Sydney, 1996, WB Saunders Company.
17) Local Control of Blood Flow by the Tissues and Humoral Regulation. In Guyton AC, Hall JE, editors: Textbook of Medical Physiology, 9th ed. Sydney, 1996, WB Saunders Company.
18) Seizures. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
19) Rodenticides. Information pages from the EPA. Author not listed. http://www.epa.gov/opp00001/safety/healthcare/handbook/Chap17.pdf.
20) Anticoagulant poisons for rats and possums: Your questions answered. Information pages from the Northland Regional Council of New Zealand. Author not listed. http://www.nrc.govt.nz/upload/2268/Anticoagulant%20poisons%20(Feb%2007).pdf.
21) Marshall EF, A Common Sense Approach To Commensal Rodent Control. In: Wildlife Damage Management, Internet Centre for Great Plains Wildlife Damage Control Workshop Proceedings. Nebraska, 1981. http://digitalcommons.unl.edu/cgi/viewcontent.cgi?article=1138&context=gpwdcwp.
22) Murphy MJ,Anticoagulant Rodenticides. In Gupta RC, editor: Veterinary Toxiciology: Basic and Clinical Principles. 2007, Elsevier Inc.
23) Tasheva M,Environmental Health Criteria for Anticoagulant Rodenticides. 1995, World Health Organisation. http://www.inchem.org/documents/ehc/ehc/ehc175.htm#SectionNumber:5.1.
24) Hamilton RJ, Sanchez M, Oral Anticoagulation Management. Anticoagulation Management Centre, New Orleans, date unknown, Jobson. http://www.uspharmacist.com/oldformat.asp?url=newlook/files/feat/oralanticoagulation.htm.
25) Fournier-Chambrillon C, et al. Evidence of Secondary Poisoning of Free-ranging Riparian Mustelids by Anticoagulant Rodenticides in France:
Implications for Conservation of European Mink (Mustela lutreola). In: Journal of Wildlife Diseases. 40(4), 2004, pp. 688-695.
26) Prater MR, Acquired Coagulopathy I: Avitaminosis K. In Feldman BF, et al. editors: Schalm's Veterinary Hematology. USA, 2000, Blackwell Publishing.
27) Watt BE, et al. Anticoagulant Rodenticides. In: Toxicological Reviews. 24(4), 2005, pp. 259-269.
28) Weitzel JN, et al. Surreptitious Ingestion of a Long-acting Vitamin K Antagonist/Rodenticide, Brodifacoum:
Clinical and Metabolic Studies of Three Cases. In: Blood. 76(12), 1990, pp. 2555-2559.
29) Anticoagulant Poisons. Information pages from the New Zealand Government. Author not listed. http://www.doc.govt.nz/upload/documents/science-and-technical/docts23b.pdf.
30) Curtin University of Technology (2008, June 18). Dingo Urine Offers Humane Solution To Kangaroo Cull. In. ScienceDaily. Retrieved July 9, 2008, from http://www.sciencedaily.com /releases/2008/06/080613143647.htm
31) Article on Menadione in www.answers.com. Author unknown. http://www.answers.com/topic/menadione?cat=health.
32) Article on Phytomenadione in www.answers.com. Author unknown. http://www.answers.com/phytomenadione.
33) Information on Ropel comes from the product website - http://www.nixalite.com/ropel.aspx.
34) Information on Eradibait comes from the product website - http://www.eradi-products.com/.
35) Long-Acting Anticoagulant Rodenticides. Author Unknown. Publication of the
Iowa Statewide Poison Control Centre. http://www.iowapoison.org/index.asp?pageID=150.
36) Rodenticide Poisoning: Introduction. In Merck's Veterinary Manual. New Jersey, 2008, Merck and Company Inc.
37) Information on Rabbait comes from the product website - http://www.animalcontrol.com.au/rabbit-bait1.htm.
38) The NRA Review of Pindone. In the NRA Review Series - National Registration Authority for Agricultural
and Veterinary Chemicals. Canberra. 2002. http://www.apvma.gov.au/chemrev/downloads/pindone2.pdf.
39) Final Risk Mitigation Decision for Ten Rodenticides. The US Environmental Protection Agency, 2008. http://www.epa.gov/oppsrrd1/reregistration/rodenticides/finalriskdecision.htm.
40) DuVall MD, et. al. Case Studies on Second Generation Anticoagulant Rodenticide Toxicities
in Non-target Species. In Journal of Veterinary Diagnostic Investigation. 1, 1989, pp 66-68.
41) Illegal Pesticide Products. The US Environmental Protection Agency, 2008. http://www.epa.gov/pesticides/health/illegalproducts/index.htm.
42) Harrell TW, et al. Anticoagulant Rodenticide Toxicosis in the Dog and Cat. The College of Veterinary Medicine, University of Georgia, 2003. http://www.vet.uga.edu/VPP/clerk/Harrell/index.php.
43) Ipecac. Plumb DC, Plumb's Veterinary Drug Handbook. usa, 2005, Blackwell Publishing.
44) Charcoal. Plumb DC, Plumb's Veterinary Drug Handbook. usa, 2005, Blackwell Publishing.
45) Abrams-Ogg A, The Cat with Acute Depression, Anorexia or Dehydration. In Rand J, editor: Problem-based Feline Medicine, Sydney, 2006, Elsevier Saunders.

Pet Informed is not in any way affiliated with or opposed to any of the companies whose products
appear in images or information contained within this article. The images, taken by Pet Informed, are only used in order to illustrate certain points being made in the article.
Copyright July 17, 2008, www.pet-informed-veterinary-advice-online.com.
All rights reserved, protected under Australian copyright. No images or graphics on this Pet Informed website may be used without written permission of their owner, Dr. O'Meara.
Kaput is a registered trademark of Scimetrics Ltd Corp.
Contrac, Ditrac, Fastrac, Final, Tomcat, Liqua-Tox, Quintox, PCQ Rodenticide-CA, Talpirid Mole Bait, RodentRid, ZP,
Protecta MC and Trapper 24/7 Humane Mouse Trap are registered trademarks of Bell Laboratories Inc.
Gopher Bait 50 is a registered trademark of Control solutions incorporated.
JT Eaton, A-C Formula 90, Bait Block, Bait Blocks, Top Gun, Repeater (clear top
live catch trap), JT Eatons Wind-Up Mouse Trap, JT Eaton Answer are trademarks of J.T. Eaton and Co.
Generation, Maki, Rozol, BlueMax, Ground Force are trademarks of Liphatech.
Talon, Talon-G, Havoc, Klerat, Ratak, Ratak Plus and WeatherBlok are trademarks of Syngenta Group Company.
Bitrex is a trademark of Macfarlan Smith Ltd.
Adios, Mouse Killer, Gopher Killer, Mole Killer are trademarks of Adios Products.
Feratox, Feracol, RatAbate are trademarks of Connovation Ltd.
Ropel is a trademark of Nixalite of America Inc.
EradiBait, EradiMouse and EradiRat are trademarks of Natrocell Technologies Ltd.
Rabbait and MouseOff are trademarks of Animal Control Technologies.
Ratsak is a registered trademark of Arthur Yates and Co.
Racumin, Drat and Endox are registered trademarks of Bayer.
Bromakil is a registered trademark of Rentokil.
Coumadin is a registered trademark of the Bristol-Myers Squibb Company.
Marevan and Panadol are a trademarks of the GlaxoSmithKline Group of Companies.
Bromone is a trademark of Nu-Gro.
Storm is a trademark of BASF.
Frunax and Frunol Delicia are trademarks of Frunol Delicia.
RCO Mole and Gopher Patrol Bait, RCO Squirrel Patrol Bait, RCO Omega Gopher Grain Bait
RCO/R-M Vole Bait and RCO Mole Patrol Bait are products of RCO Pest Control Products.
Ramik is a Registered Trademark of Hacco, Inc.
Rampage is a Registered Trademark of Motomco Ltd.
Ortho Rat-B-Gone and Ortho Mouse-B-Gone are Registered Trademarks of the Scotts Miracle-Gro Company.
Trounce is a Registered Trademark of Virbac Corp.
Hot Shot and Sudden Death Mouse Killer are Registered Trademarks of United Industries Corp.
Lectric Soda Crystals are produced by Cedel. Pty. Ltd.
Carbosorb XS and Carbosorb are registered trademarks of Phebra Pty Ltd.
Adrenaline BP is a registered trademark of Astra Zeneca.
Actilax is a registered trademark of Alphapharm Pty Ltd.
Duphalac is a registered trademark of Solvay Pharmaceuticals.
The Caniplas product pictured is a product of Plasvacc.
A.C.P.2 is a registered trademark of Delvet Pty Ltd.
K-Mav Vit K1 Tablets is a registered trademark of Mavlab Pty Ltd.
Koagulon Injection is a registered trademark of Parnell Laboratories (Aust) Pty. Ltd.
Shake-Away is a registered trademark of Shake-Away.
PestChaser Electronic Rodent Repeller is a trademark of Sonic Technology Products.
The Electronic Rat Trap, Corner Cat Multiple Mouse Trap and Victor Tin Cat Repeating Mouse Trap are all products of Victor.
The Ranger # T231 Rat/Squirrel/Small Rodent Live Trap is a product of Lone Star Traps.
The trip Trap is a product of Big Cheese.
Havahart is a trademark of Havahart.com.
Please note: the aforementioned rodenticide treatment schedules and rodenticide
prevention guidelines and information on the rodenticidal poisoning of dogs and cats are general recommendations only. The information provided is based on published information and recommendations made available from the drug companies themselves; relevant veterinary literature and publications and my own experience as a practicing veterinarian.
The advice given is appropriate to the vast majority of pet owners, however, given
the large range of poison types and treatment and prevention protocols now available, owners should take it upon themselves to ask their own veterinarian what treatment and poison prevention schedules s/he is using so as to be certain what to do. Owners with specific circumstances (high poison
contamination in their environment, pregnant bitches and queens, newborn litters, breeders, high rodent burdens, sensitive surrounding wild animal populations etc. etc.) should ask their vet what the safest and most effective poison-choice, poison treatment and poison prevention
protocol is for their situation. Extra advice can be obtained by speaking with pest
control companies (they deal in these products every day) and with your local
government centres for vermin and pest animal control.
Any dose rates mentioned on these pages should be confirmed by a vet. Dosing rates for common
drugs are being changed and updated all the time (e.g. as new research comes in and as drug
formulations change) and information here may not remain current for long. What's more, although we try very hard to maintain the accuracy of our information, typos and oversights do occur. Please check with your vet before dosing any pet any medication or drug.
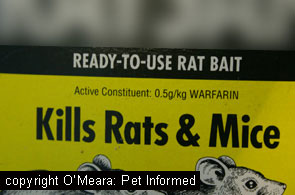 The first-generation anticoagulant compounds were the first of the coumarin-derived chemicals invented for controlling rodent pests. Less potent than the more recent, second-generation anti-coagulant poisons, these first-generation compounds require a mouse or rat to feed on them over a course of several
days, gradually accumulating a lethal dose of poison in their tissues, before they
will cause death in the pest animal. Although a single, large feed of a first-generation bait will sometimes poison a cat or dog, first-generation rodent poisons do not persist as long in the dog or cat's tissues and blood (i.e. they have a shorter biological half-life)
and, thus, much shorter courses of antidote medication (Vitamin K1) are required to treat these patients. Additionally, because the mouse or rat often has to feed for several days in order to obtain a dose of poison that is lethal to it (i.e. a cumulative dose that is usually too small to be lethal to a dog or cat predator), the chances of secondary poisoning, whereby the dog or cat becomes
poisoned by eating a dead or dying vermin animal, are very low with these compounds.
The first-generation anticoagulant compounds were the first of the coumarin-derived chemicals invented for controlling rodent pests. Less potent than the more recent, second-generation anti-coagulant poisons, these first-generation compounds require a mouse or rat to feed on them over a course of several
days, gradually accumulating a lethal dose of poison in their tissues, before they
will cause death in the pest animal. Although a single, large feed of a first-generation bait will sometimes poison a cat or dog, first-generation rodent poisons do not persist as long in the dog or cat's tissues and blood (i.e. they have a shorter biological half-life)
and, thus, much shorter courses of antidote medication (Vitamin K1) are required to treat these patients. Additionally, because the mouse or rat often has to feed for several days in order to obtain a dose of poison that is lethal to it (i.e. a cumulative dose that is usually too small to be lethal to a dog or cat predator), the chances of secondary poisoning, whereby the dog or cat becomes
poisoned by eating a dead or dying vermin animal, are very low with these compounds.
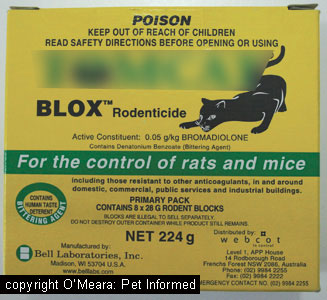 The second generation anticoagulant rodenticide compounds were the most recent coumarin-derived chemicals invented for use in killing rodent pests. They were developed because, in certain locations where widespread, intensive first-generation rodenticide use was occurring (e.g. Europe, USA),
many of the rats and mice were becoming resistant to the first-generation poisons, leading to
a failure of effective rodent control in these regions. Highly potent, the second-generation anti-coagulant rat poisons are easily able to kill a mouse or a rat after only a single feed of bait. A single feed of a second-generation rodent bait will, likewise, poison a cat or dog and, because these chemicals persist in the dog or cat's tissues (especially the animal's liver and fat) for a long time, long courses of antidote treatment (Vitamin K1) are required to effectively treat animals that have been inadvertently poisoned (around 5-6 weeks of treatment). Additionally, because the mouse or rat only has to feed once to obtain a lethal dose of poison (a single dose that may well exceed the minimum amount that would
have been needed to kill it) the chances of secondary poisoning of carnivorous pets are much higher with these compounds. In a single feed, a mouse or rat may be capable of consuming and storing in its tissues a dose of poison that is lethal for a dog or cat or wild animal predator.
The second generation anticoagulant rodenticide compounds were the most recent coumarin-derived chemicals invented for use in killing rodent pests. They were developed because, in certain locations where widespread, intensive first-generation rodenticide use was occurring (e.g. Europe, USA),
many of the rats and mice were becoming resistant to the first-generation poisons, leading to
a failure of effective rodent control in these regions. Highly potent, the second-generation anti-coagulant rat poisons are easily able to kill a mouse or a rat after only a single feed of bait. A single feed of a second-generation rodent bait will, likewise, poison a cat or dog and, because these chemicals persist in the dog or cat's tissues (especially the animal's liver and fat) for a long time, long courses of antidote treatment (Vitamin K1) are required to effectively treat animals that have been inadvertently poisoned (around 5-6 weeks of treatment). Additionally, because the mouse or rat only has to feed once to obtain a lethal dose of poison (a single dose that may well exceed the minimum amount that would
have been needed to kill it) the chances of secondary poisoning of carnivorous pets are much higher with these compounds. In a single feed, a mouse or rat may be capable of consuming and storing in its tissues a dose of poison that is lethal for a dog or cat or wild animal predator.
 Another common 'at-home' poisoning situation that I have encountered is the poisoning that occurs when
a person, normally a renter or new house-owner, moves into a new house for the first time, unaware that the previous tenant has put down rat poison. Generally, if the new owner or tenant
has explored his or her new house thoroughly, he or she will have removed any rodenticide boxes located in obvious areas like the corners of rooms and the inside of kitchen cupboards. However, there are many obscure places that people will commonly hide bait boxes. Places to also check include: garden sheds, the gap behind or alongside garden sheds, behind hot water systems (e.g. under the kitchen sink), behind doors (the space
behind the door that gets hidden when you open a door into a bedroom), inside walk-in-robes,
inside pantries, behind or alongside the fridge, under the house (beware of snakes and spiders if you check here though), under the oven, in the gap beside the
oven and bench or the oven and nearest walls, inside the ceiling space. Without a careful, step-by-step, systematic, house-and-yard hunt for these hidden baits, you may not even notice them, however, you can be very sure that your canine or feline friend's keen nose will discover them one day when you are out at work.
Another common 'at-home' poisoning situation that I have encountered is the poisoning that occurs when
a person, normally a renter or new house-owner, moves into a new house for the first time, unaware that the previous tenant has put down rat poison. Generally, if the new owner or tenant
has explored his or her new house thoroughly, he or she will have removed any rodenticide boxes located in obvious areas like the corners of rooms and the inside of kitchen cupboards. However, there are many obscure places that people will commonly hide bait boxes. Places to also check include: garden sheds, the gap behind or alongside garden sheds, behind hot water systems (e.g. under the kitchen sink), behind doors (the space
behind the door that gets hidden when you open a door into a bedroom), inside walk-in-robes,
inside pantries, behind or alongside the fridge, under the house (beware of snakes and spiders if you check here though), under the oven, in the gap beside the
oven and bench or the oven and nearest walls, inside the ceiling space. Without a careful, step-by-step, systematic, house-and-yard hunt for these hidden baits, you may not even notice them, however, you can be very sure that your canine or feline friend's keen nose will discover them one day when you are out at work.  Your house is broken into. Some baitings of pets (particularly the use of rapid-acting baits) occur because thieves are trying to rid themselves of a guard dog. The sudden death of a pet, shortly followed by a burglary, should always rouse suspicion that the pet was deliberately targeted.
Your house is broken into. Some baitings of pets (particularly the use of rapid-acting baits) occur because thieves are trying to rid themselves of a guard dog. The sudden death of a pet, shortly followed by a burglary, should always rouse suspicion that the pet was deliberately targeted. 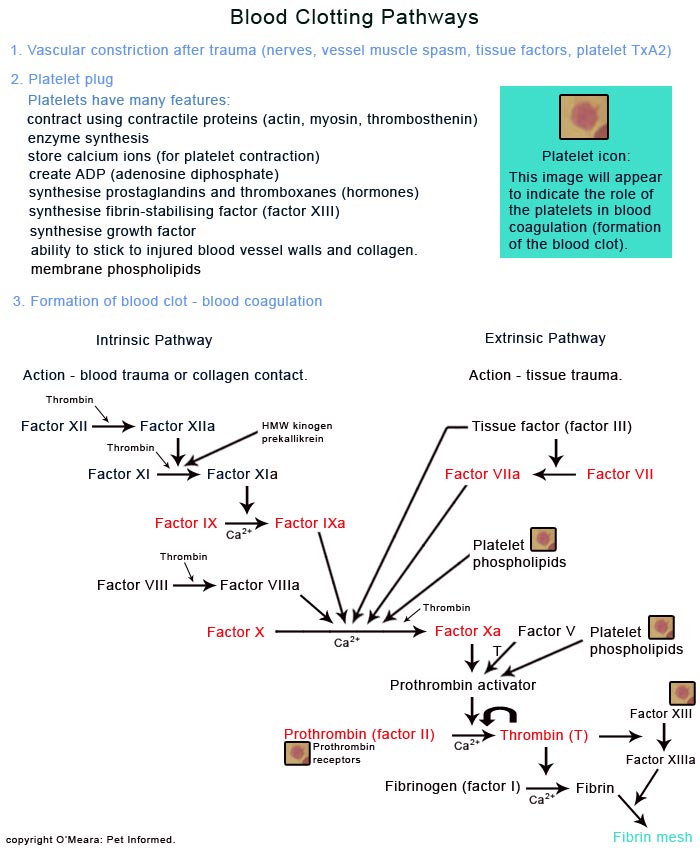
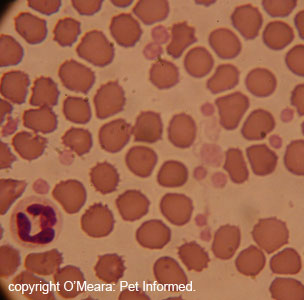
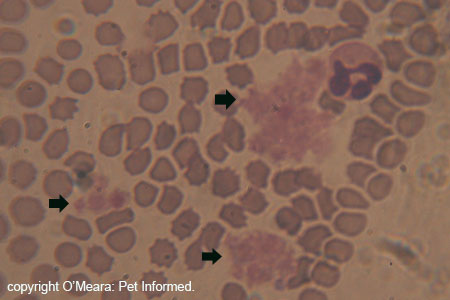
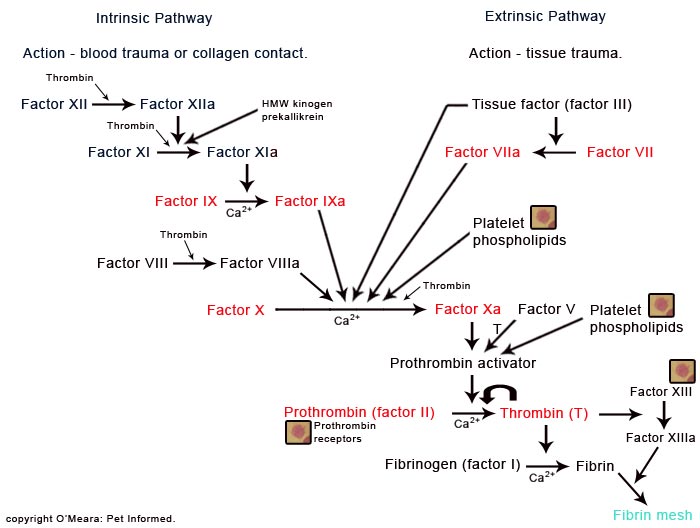
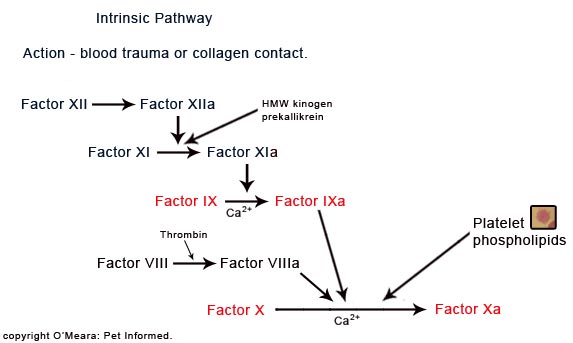
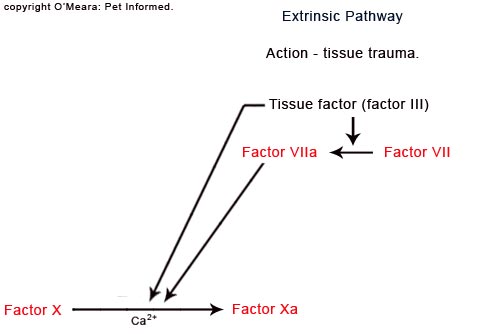
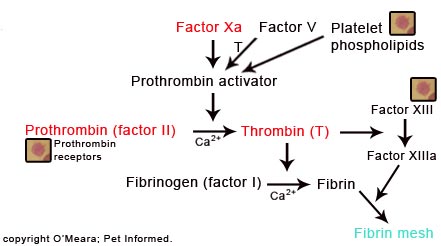

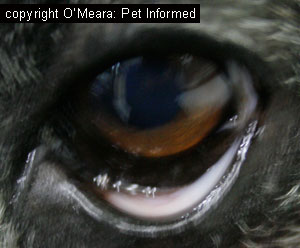

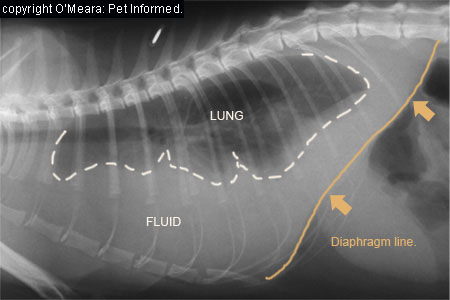

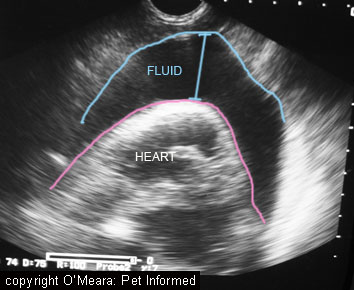
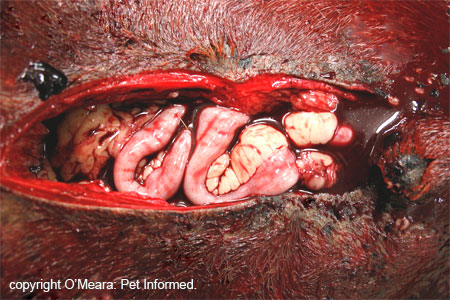



 In most cases of rodenticide toxicity it is the owners of the pet, not a wayward bird or nasty neighbour,
who have put down the rodent poison that has caused their pet to bleed. Thus, veterinarians
tend to get a very strong clue as to the cause of a pet's excessive bleeding simply by
asking the question: "Have you put down any rat bait lately?" Most owners will tell
the truth about this, even if they do feel a tad guilty, and this makes the vet's diagnosis and
treatment plan very easy. The only difficulty comes when owners will not admit that they have
put down a poison and the vet has to work-out what has gone wrong with the animal's blood. Such time delayed whilst a diagnosis is being sought may potentially cost a pet its life.
In most cases of rodenticide toxicity it is the owners of the pet, not a wayward bird or nasty neighbour,
who have put down the rodent poison that has caused their pet to bleed. Thus, veterinarians
tend to get a very strong clue as to the cause of a pet's excessive bleeding simply by
asking the question: "Have you put down any rat bait lately?" Most owners will tell
the truth about this, even if they do feel a tad guilty, and this makes the vet's diagnosis and
treatment plan very easy. The only difficulty comes when owners will not admit that they have
put down a poison and the vet has to work-out what has gone wrong with the animal's blood. Such time delayed whilst a diagnosis is being sought may potentially cost a pet its life.

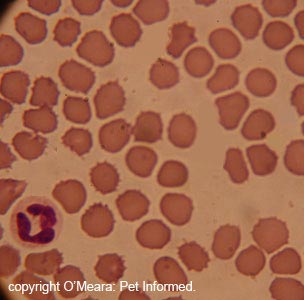

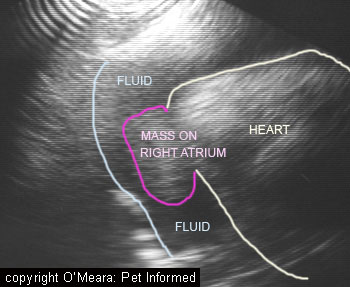
 If possible, it is always better if you take a pet to a vet clinic in order to
make it vomit. In my experience, most owners tend to find trying to make pets vomit at home an
unrewarding experience that often just wastes precious time in which a pet could be taken to a vet clinic and made to vomit. Vets have excellent drugs at their disposal to make pets vomit and tend to get much more reliable results.
If possible, it is always better if you take a pet to a vet clinic in order to
make it vomit. In my experience, most owners tend to find trying to make pets vomit at home an
unrewarding experience that often just wastes precious time in which a pet could be taken to a vet clinic and made to vomit. Vets have excellent drugs at their disposal to make pets vomit and tend to get much more reliable results.
 What if you have more than one pet who could have eaten the bait? Do you take them all in to the vet?
What if you have more than one pet who could have eaten the bait? Do you take them all in to the vet? Making pets vomit in order to remove ingested poisons is only really helpful if the
animal is made to vomit within the first 2-4 hours of ingesting a poisonous substance. In the hours after this period, although some poison residues may still be brought up
if vomiting is induced, the vast majority of the poison load will have either been absorbed into the animal's body or moved on through the stomach to the intestines, where vomiting won't remove it.
Making pets vomit in order to remove ingested poisons is only really helpful if the
animal is made to vomit within the first 2-4 hours of ingesting a poisonous substance. In the hours after this period, although some poison residues may still be brought up
if vomiting is induced, the vast majority of the poison load will have either been absorbed into the animal's body or moved on through the stomach to the intestines, where vomiting won't remove it. 

 Gastric lavage or "stomach pumping" is the process whereby an animal that has eaten a
poison within the last 3 hours is placed under an anaesthetic and the poison washed out of its stomach
manually. Don't panic. No surgery is needed to do this. A medium to large diameter stomach tube is simply slid
down the animal's throat and into its stomach. Water is drenched down the tube to semi fill the animal's stomach and then this water is allowed to passively drain back out of the stomach via this same tube (or a second, larger tube) into a bucket, hopefully carrying the poison out of the stomach with it.
Gastric lavage or "stomach pumping" is the process whereby an animal that has eaten a
poison within the last 3 hours is placed under an anaesthetic and the poison washed out of its stomach
manually. Don't panic. No surgery is needed to do this. A medium to large diameter stomach tube is simply slid
down the animal's throat and into its stomach. Water is drenched down the tube to semi fill the animal's stomach and then this water is allowed to passively drain back out of the stomach via this same tube (or a second, larger tube) into a bucket, hopefully carrying the poison out of the stomach with it. 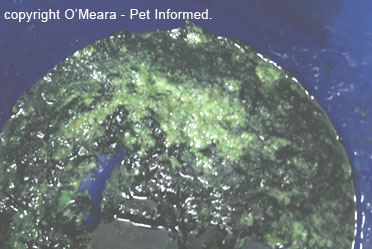


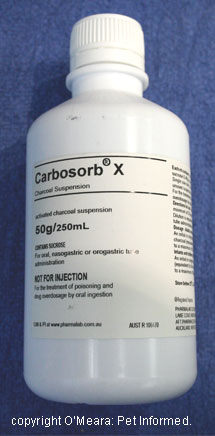 An adsorbent is a finely granular, high surface area product (normally given as a powder or liquid slurry or crushed tablet) that is designed to bind up any remaining poison in the animal's intestines and stomach and, thus, make that
poison unavailable for the intestines to absorb into the patient's body. Charcoal, available as a powder, slurry or tablet, is the adsorbent most commonly used by veterinarians.
An adsorbent is a finely granular, high surface area product (normally given as a powder or liquid slurry or crushed tablet) that is designed to bind up any remaining poison in the animal's intestines and stomach and, thus, make that
poison unavailable for the intestines to absorb into the patient's body. Charcoal, available as a powder, slurry or tablet, is the adsorbent most commonly used by veterinarians. 
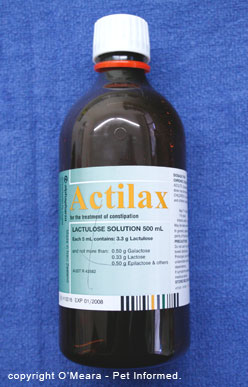 A cathartic is a substance that is designed to speed up the gastrointestinal transit time of the poison-containing intestinal contents. Put simply, a cathartic increases and stimulates intestinal motility. It stimulates
the intestines to move and push the intestinal contents, including any poisons, through more quickly so that there is less time available for the intestine to absorb
the poison into the body.
A cathartic is a substance that is designed to speed up the gastrointestinal transit time of the poison-containing intestinal contents. Put simply, a cathartic increases and stimulates intestinal motility. It stimulates
the intestines to move and push the intestinal contents, including any poisons, through more quickly so that there is less time available for the intestine to absorb
the poison into the body.
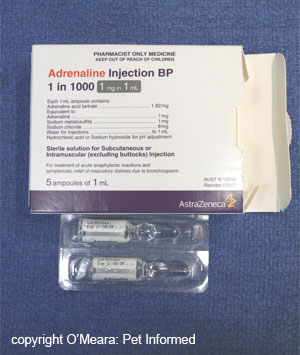
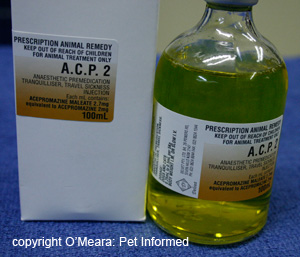
 The use of vitamin K1 (doses, duration of treatment, ways of optimising absorption at home etc) has been thoroughly discussed in section 8f and much of the information provided in
that section pertains to this section also.
The use of vitamin K1 (doses, duration of treatment, ways of optimising absorption at home etc) has been thoroughly discussed in section 8f and much of the information provided in
that section pertains to this section also. 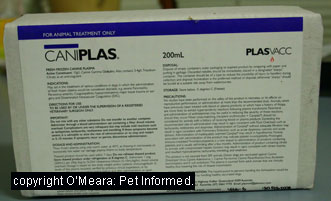 Plasma is the fluid that remains when you remove all of the cells from blood. It contains
many helpful substances and properties that can really make a huge difference to the survival chances of rodenticide affected pets. It is the first choice intravenous fluid for treating animals with rodenticide toxicity which haven't yet lost enough blood cells
to require a blood transfusion (see section 9f).
Plasma is the fluid that remains when you remove all of the cells from blood. It contains
many helpful substances and properties that can really make a huge difference to the survival chances of rodenticide affected pets. It is the first choice intravenous fluid for treating animals with rodenticide toxicity which haven't yet lost enough blood cells
to require a blood transfusion (see section 9f). Some patients lose so much blood as a result of rodenticide toxicity haemorrhage that they
can actually become severely anemic (i.e. they don't have enough red blood cells left in their body) in addition to losing blood volume and dropping in blood pressure. The role of these red blood
cells is to transport oxygen around the animal's body. Animals that do not have enough
red blood cells (anemic animals) are unable to supply oxygen to all of their tissues and, as a result, the tissues, particularly the highly-oxygen-dependent tissues such as the brain, kidney
and heart, can start to become damaged and die, resulting in the death of the animal.
Some patients lose so much blood as a result of rodenticide toxicity haemorrhage that they
can actually become severely anemic (i.e. they don't have enough red blood cells left in their body) in addition to losing blood volume and dropping in blood pressure. The role of these red blood
cells is to transport oxygen around the animal's body. Animals that do not have enough
red blood cells (anemic animals) are unable to supply oxygen to all of their tissues and, as a result, the tissues, particularly the highly-oxygen-dependent tissues such as the brain, kidney
and heart, can start to become damaged and die, resulting in the death of the animal.