Veterinary Advice Online: How Do Vaccines Work?
An owner-friendly article designed to improve your understanding of vaccines and how they work.
The following article discusses the mechanisms by which vaccinations protect pets from
disease and examines the types of vaccines used in cats and dogs (and other animals) to prevent the major disease-causing organisms that can infect our pets. The article
discusses the pros and cons of the live, killed and intranasal vaccines and explores the situations in which they
are most applicable.
This article contains the following information about vaccines:
1) What is contained in a vaccine?
2) How does a vaccine work? - a basic summary.
3) How do vaccines work? - a detailed description of how the immune system induces
a protective response against infectious organisms:
3a) Some basic definitions.
3b) The naive immune system of young animals - why unvaccinated animals are at risk of disease.
3c) The importance of colostrum in young animals prior to vaccination.
3d) The cells of the immune system: how they respond to foreign antigens (including vaccines)
that they have never been exposed to before.
3e) How vaccination protects animals against future disease threats.
4) Frequently asked questions about vaccination.
5) Live attenuated vaccines.
6) Killed vaccines and subunit vaccines.
7) The pros and cons of live versus killed vaccines.
8) Different routes of administration of vaccines (e.g. intranasal vaccines).
WARNING - IN THE INTERESTS OF PROVIDING YOU WITH COMPLETE AND DETAILED INFORMATION, THIS SITE DOES CONTAIN MEDICAL AND SURGICAL IMAGES THAT MAY DISTURB SOME READERS.

1. What is contained in a vaccine?
 When an animal (or human) is vaccinated, a veterinarian injects a small amount of a virus or bacteria (or other infectious agent) under the skin of the animal. This organism that gets injected
is generally a non-harmful strain of the virus or bacteria that we are protecting our pets from
(live vaccine) or a killed form of the actual wild-type, disease-causing virus or bacteria. The injection may contain live organisms (termed a live vaccine); inactivated organisms, incapable
of replicating in the body (termed a killed vaccine) or just little bits of the organisms: specific proteins or sugars (termed antigens) that the immune system will recognise as foreign to the body
(vaccines made of bits of an organism are termed a subunit vaccines and are a form of killed vaccine). As will be discussed in the killed vaccine section, killed vaccines and subunit vaccines
are generally less immune-stimulatory (less capable of inducing immune reaction) than live vaccines
and so additives (termed adjuvants) which enhance the immune system's response to the vaccine
are generally added to the killed vaccines to improve their effect.
When an animal (or human) is vaccinated, a veterinarian injects a small amount of a virus or bacteria (or other infectious agent) under the skin of the animal. This organism that gets injected
is generally a non-harmful strain of the virus or bacteria that we are protecting our pets from
(live vaccine) or a killed form of the actual wild-type, disease-causing virus or bacteria. The injection may contain live organisms (termed a live vaccine); inactivated organisms, incapable
of replicating in the body (termed a killed vaccine) or just little bits of the organisms: specific proteins or sugars (termed antigens) that the immune system will recognise as foreign to the body
(vaccines made of bits of an organism are termed a subunit vaccines and are a form of killed vaccine). As will be discussed in the killed vaccine section, killed vaccines and subunit vaccines
are generally less immune-stimulatory (less capable of inducing immune reaction) than live vaccines
and so additives (termed adjuvants) which enhance the immune system's response to the vaccine
are generally added to the killed vaccines to improve their effect.

2. How does a vaccine work? - a basic summary.
The mechanism by which vaccination works is complex and involves many chemical and cellular reactions within and between the immune system cells of the body. Basically, the role of vaccination is to expose the naive immune system (immune system
that has not yet been exposed to the foreign proteins/sugars - termed antigens - contained on attacking organisms) to viral and bacterial antigens contained within the vaccine so that, in the future, if the body gets attacked by a related virus / bacteria the immune system will recognise (remember) the antigens contained on these infectious disease organisms and activate very quickly (within hours as opposed to weeks with an
unvaccinated, inexperienced immune system) to kill them. By having a large, mature immune response activate more rapidly, the hope is that the invading disease-causing organisms will be neutralised more quickly (before they get to replicate or invade deep into
the body), thereby resulting in only mild, if any, clinical disease.

3. How does a vaccination work? - a detailed description of how the immune system induces
a protective response against infectious organisms.
3a. Some Definitions:
White blood cell - a general term for any cell of the immune system.
Lymphocyte - a particular white blood cell line that exists in the body. There are
two main types of lymphocyte - T lymphocytes (also called T cells) and B lymphocytes
(also called B cells which, once mature and making antibodies, are termed plasma cells). T lymphocytes regulate immune system responses and are involved in activating other immune and inflammatory cells including B cells. B cells make antibodies against antigens that are foreign to the body. Importantly, both T and B cells (and the antibodies made by B cells) are antigen specific - they will only trigger immune-system attack against antigens that they recognise as being foreign (in this way, immune system responses can be targeted only to invading threats).
Antigen - a protein or sugar (carbohydrate) contained on the surface of a cell, foreign object or infectious organism that the immune system can recognise and decide
to attack. The immune system identifies antigens as being 'self' (normal to the body) or
foreign (not normally found in the body). In normal animals, the immune system only attacks foreign antigens (e.g. antibodies should only be produced against
foreign antigens).
Antibody - a protein made by a B cell that binds to a very specific antigen. Each different B cell
(plasma cell) makes only one type of antibody and this antibody is very specific for a particular antigen. When an antibody finds a foreign antigen, it binds to the antigen and then calls other inflammatory
cells over to kill it.
Virulent - when used to describe an infectious organism, it means that the organism
is able to cause severe disease particularly in the non-vaccinated animal.
Wild-type - when used to describe an infectious organism, this term refers to
the viruses and bacteria that exist in the environment naturally. In terms of this discussion, wild-type viruses and bacteria are those that the animal encounters in the environment
and which have the potential to cause disease. These are the organisms that we are protecting animals against when we vaccinate.
3b. The naive immune system - why unvaccinated animals are at risk of disease.
When an animal is born, its immune system has all of the components contained in the
immune system of an older animal, except that it is very naive (has never been exposed
to any foreign antigens before). The consequence of this is: should such an animal
be exposed to a really virulent strain of infectious disease, its immune system (having never been exposed to the antigens present on the surface of this organism before)
will take ages (up to 2 weeks) to mount a defensive response against the disease. The
disease will potentially get a 2 week head-start on the animal without being opposed
by its immune system (after all, it takes time for immune cells to divide and build
up their forces and start producing protective antibodies). Thus the animal may develop really severe illness and could even die (with distemper, parvovirus and rabies the chance of death is really high).
3c. The importance of colostrum in young animals prior to vaccination.
It is important to make a mention of colostrum here: the main reason why most
puppies and kittens do not die of infectious disease shortly after birth is that
most of them drink their mother's colostrum. This colostrum contains antibodies to
the major infectious disease organisms (including organisms that the bitch / queen
was vaccinated against) and these antibodies circulate around the puppies' /
kittens' immune systems, defending the young animals from infection. Puppies and kittens that fail to get their colostrum are very susceptible to infection shortly after birth.
3d. The cells of the immune system: how they respond to foreign antigens (including vaccines)
that they have never been exposed to before.
The immune system of the young animal contains many different cell types. For the purpose of
this discussion, these can be broken up into two main groups:
1) Those cells that are non-antigen-specific in their responses. After being
called into an area of infection by chemical messages sent out from antigen-specific cells and antigen-specific-antibody-reactions (see following section), these cells come into a region of infection
in large numbers to do battle. They do battle by either gobbling up any infectious organisms or tissue debris in the area or by releasing nasty chemicals that pretty much blast everything in the local region, including healthy tissue. The non-antigen-specific cells include the pus-forming white blood cells (neutrophils, macrophages) and other inflammatory cells (mast cells, basophils etc.)
Note that some of these cells do have some ability to identify certain infectious organisms and mount an attack against them, regardless of the presence of an antigen-specific immune response: this ability
may allow animals with a very naive immune system (esp. animals that didn't get colostrum) to fight against some infectious organisms to some degree.
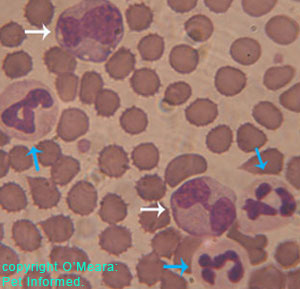
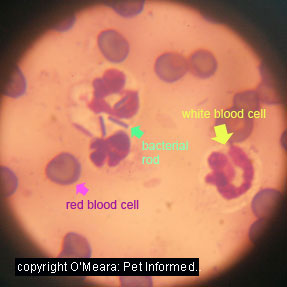
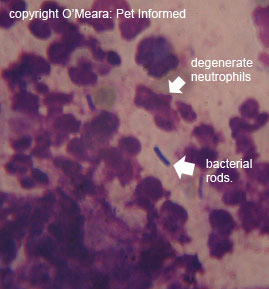
Image 1: White blood cells in blood (blue arrows neutrophils, white arrows macrophages).
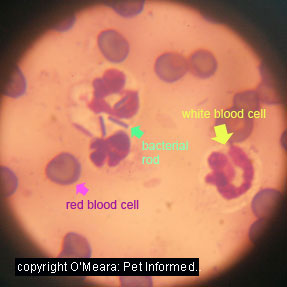
Image 2: Infected urine smear. White blood cell (yellow arrow) is a neutrophil. Another neutrophil has 'eaten' several bacterial rods (green arrow).
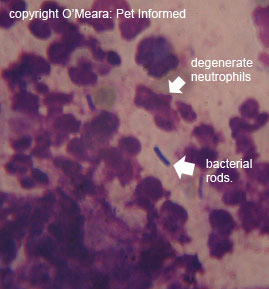
Image 3: Infected anal gland smear. Note the indistinct appearance of the white blood cells in the image. These are degenerate
neutrophils which have disintegrated in the process of releasing toxic chemicals into the area to kill the bacterial rods.
 2) Those cells that are antigen-specific in their responses. Certain lines of cells are designed to only mount a response against certain specific, recognised antigens that are present on
the surface of organisms, foreign bodies and other invaders and that are different (foreign) to antigens
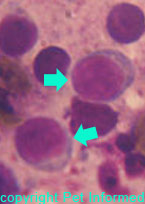
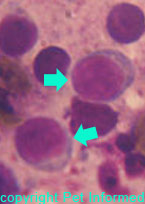
present on the body's own cells. Termed T lymphocytes and B lymphocytes (see definition section and image opposite), large populations of each of these antigen-specific cell types are present in the body at birth.
During the young animal's time in utero, every one of these cells is carefully screened by the embryonic immune system, to ensure that they recognise the antigens present on the body's cell surfaces as 'self' (and thus not attack them) and to ensure that they can detect the differences between these 'self' antigens and the 'non-self' antigens present on foreign invaders (these antigens are sufficiently different from the 'self'
antigens contained on the body's cells that the lymphocytes will bind to them and
induce an immune system attack against them). It is these cells - the lymphocytes - that are of most importance when talking about vaccination.
2) Those cells that are antigen-specific in their responses. Certain lines of cells are designed to only mount a response against certain specific, recognised antigens that are present on
the surface of organisms, foreign bodies and other invaders and that are different (foreign) to antigens
present on the body's own cells. Termed T lymphocytes and B lymphocytes (see definition section and image opposite), large populations of each of these antigen-specific cell types are present in the body at birth.
During the young animal's time in utero, every one of these cells is carefully screened by the embryonic immune system, to ensure that they recognise the antigens present on the body's cell surfaces as 'self' (and thus not attack them) and to ensure that they can detect the differences between these 'self' antigens and the 'non-self' antigens present on foreign invaders (these antigens are sufficiently different from the 'self'
antigens contained on the body's cells that the lymphocytes will bind to them and
induce an immune system attack against them). It is these cells - the lymphocytes - that are of most importance when talking about vaccination.
When the animal is first born, although there are lots of lymphocytes (both
T cell and B cell varieties) present in the young body, each individual lymphocyte
is only able to recognise and bind to a very particular antigen (i.e. just one possible
protein or sugar molecule combination among the many millions of foreign antigen combinations
present in the environment). Among the many millions of lymphocytes present in the body at birth, the desire is that at least a few among them will have the right combination of surface
protein molecules (termed T-cell markers) needed to recognise and bind to any particular antigen that the body might
encounter. The significance of this is: when an infectious organism that has
not been encountered by the body before attacks, although there will be T lymphocytes and B lymphocytes present in the body which are capable of recognising and establishing an
immune response against the organism's particular antigens, there will not be that many of them. In the presence of the infectious organisms, the small group of lymphocytes bearing the right antigen-recognition
proteins will need to multiply to large numbers before they will be able to mount enough of
an immune response (calling in the non-specific inflammatory cells, making enough antibodies etc) to defeat the infection. Thus (particularly in the absence of maternal antibody), the initial immune response to the infection will be weak, allowing the infectious disease
to get a head start and make the animal clinically unwell.
When the T cells and B cells bearing the right antigen-recognition proteins (T-cell markers)
do eventually get to sufficient numbers, they are instrumental in defeating infectious organisms
(far better than just the non-antigen-specific cells alone are). This is because they have so many mechanisms at their disposal for killing foreign organisms.
The T lymphocytes:
When exposed to foreign antigens, the T lymphocytes bearing the correct antigen-recognition
proteins become activated and multiply to large numbers. These activated cells bind to the foreign antigens present on the surface of the infectious organism and release chemical messages that regulate the rest of the immune system response (i.e. tell the other cells what to do). These
chemicals (termed interleukins):
1) stimulate the B cells bearing the correct antigen-recognition markers to multiply and to develop into plasma cells that secrete antibodies. B cells can not become activated to do their job without the T cells.
2) induce the 'cytotoxic T cells' to multiply and kill cells and organisms
bearing the foreign antigens. See note below on Cytotoxic T-cells.
3) activate other T cells - amplifying the response.
4) activate the non-antigen-specific white bloods cells (e.g. macrophages, neutrophils)
calling them into the region to kill off the invading organisms. These cells will
eat up infectious organisms that have been 'tagged' with antibodies (i.e. organisms that
have antibody proteins bound to their antigens) and they will release chemicals of their
own, which inflict damage upon organisms and cells in the region.
The Cytotoxic T cells:
These are a subset of T lymphocytes that have the ability to kill organisms and body cells that contain organisms (e.g. cells containing viruses). When these cytotoxic cells bind to the foreign antigens present on the organism or cell containing the organism,
they activate (in the presence of the chemical messages made by other T cells) and either:
1) release chemicals that destroy the cell / organism or
2) release a chemical that puts holes in the membrane of the foreign organism or
foreign-antigen-bearing cell. The holes let fluid flow into the cell and the cell ruptures.
Unlike some of the non-antigen-specific white blood cells (e.g. neutrophils) which
die after releasing their toxic chemicals, the cytotoxic T cells remain alive for months
and are able to inflict injury on many cells and organisms. The cytotoxic T cells are
very important in destroying viruses which hide out inside the body's cells.
Overall, the immune system response directly attributed to the T cells and the cytotoxic
T cells is termed Cell Mediated Immunity (we will come back to this term when discussing the
effectivity of the live versus the killed vaccines).
The B lymphocytes and plasma Cells:
When exposed to foreign antigens in the presence of chemical messages produced by
the T cells, the B lymphocytes bearing the correct antigen-recognition proteins become activated and multiply to large numbers. These activated cells develop into mature
B cells termed plasma cells and start making antibodies. Antibodies are proteins that
specifically bind to certain foreign antigens (the exact same foriegn antigens that the B cell and T cells
specifically reacted towards) contained on the surface of infectious or foreign body organisms
and cells containing infectious organisms. There are 5 different types of antibodies (you
have probably heard of IgG antibodies and also IgE antibodies - which are involved in anaphylactic reactions such as peanut allergies in children and vaccine anaphylaxis in pets)
and, although they do vary somewhat from each other, for the purposes of this discussion they all have the following roles:
1) because each antibody can bind at least two molecules of the same antigen-type
to itself, each antibody molecule is able to link to more than bacterium or organism at a time. Many
antibodies can bind many organisms together in a clump, making them unable to move and
invade anything.
2) antibodies can bind to the surface of organisms (bound at the antigen sites)
and obstruct the areas of the organism which are responsible for the toxic effects
of the organism (e.g. the site where a bacterial toxin would be released)
3) some antibodies can induce a cell or organism to destroy itself
4) most antibodies activate a series of enzymes (termed complement) contained within the
body, which react, resulting in the formation of certain immune proteins at the site of infection.
These 'complement protein products' produced from enzyme reactions have several roles:
A) some travel in the blood as messengers, calling white blood cells into the region to kill the invaders.
B) Some activate these incoming white blood cells (neutrophils, macrophages), inducing
them to swallow up the antibody-tagged organism (e.g. bacterium)
C) Some activate inflammatory cells such as mast cells, causing them to release
proteins such as histamine and heparin into the region. These products make the local blood vessels dilate
(more blood flow to region, bringing in oxygen and nutrients for the inflammatory cells
to use) and they make the local blood vessels leaky (this results in more white blood cells
and important immune proteins being able to migrate into the region) - resulting in
the redness and swelling seen at sites of infection or inflammation.
D) Some of the complement proteins bind to the foreign cell or bacterium, putting holes in
the membrane of the invader (thus killing it in a similar way to the cytotoxic T cells).
E) Some of them even make the surfaces of the organism more sticky such that they
will bind together (termed agglutination) and be unable to move and invade.
Overall, the immune system response directly attributed to the B cells and the antibody producing plasma cells is termed Humoral Immunity (we will come back to this term when discussing the
effectivity of the live versus the killed vaccines).
3e. How vaccination protects animals against future disease threats.
"Okay," I hear you ask, "but what about vaccination? Where does that fit in?"
Well as you can see, from the above discussion, it is going to take a lot of time for the cell mediated (T cell) and humoral (B cell) responses to reach their full effects. Not only do we need to go from a relatively small and minimally effective antigen-specific T and B cell
population to a massive population of these foreign-antigen-specific cells, but somewhere
in all of that, the cells need to find time to create messenger proteins, create toxic proteins,
activate complement enzymes, call in other inflammatory white blood cells .... it is a lot of work!
But what if the correct population of antigen-specific T cells and cytotoxic T cells
were already present in large numbers within the tissues? What if the correct
types of antibodies were already there, floating around the body? What if
the animal did not have to wait for the T and B cells to multiply and for the antibodies be made?
Well, what would happen is that the T cells and antibodies would start binding to the foreign
antigens (provided that the antigens were the correct ones that the T cells and antibodies coded for)
as soon as the organisms appeared (within hours). All of the effects of the T cells and antibodies
(explained in the above section) would occur within the day and the invading organisms (attacked by large numbers of inflammatory cells and inflammatory and toxic proteins)
would not have enough time to multiply or invade the body in any big way before being killed. Without severe damage being inflicted by the infectious disease-causing organisms, the
animal would be unlikely to show signs of clinical disease.
This is the situation we aim for when we vaccinate an animal: a large population of activated T and B cells and a large circulating level of antibodies - all of which are specific for the antigens contained on the surfaces of the common disease causing viruses and bacteria that we vaccinate against (e.g. distemper, parvo virus, adenovirus, feline herpes, feline calicivirus, feline leukemia virus, feline chlamydia etc.)
When we vaccinate a dog or cat, a small amount of viral or bacterial antigen
is injected under the skin of the young animal (which has an inexperience or naive
immune system). This antigen-containing injection can comprise a whole, live, replicating virus (live vaccine) which is not virulent enough to cause disease
in the immunologically naive animal, but which has many of the exact same antigens
on its surface as the nasty disease-causing organisms OR it can comprise a killed
version of the virulent strain of virus (unable to replicate and cause disease), which also contains the surface antigens required to induce the immune system to react.
The immune system attacks the antigens in a similar fashion to that described above and,
over 2 weeks, a large population of B cells, T cells and antibodies, which are specific to those injected viral and bacterial surface antigens, forms. Unlike the situation described before, where a virulent strain of organism infected an immunologically naive animal and caused
severe disease, the 2-week time period taken to build up the immune system defenses
is not an issue here because the organisms injected are either minimally-pathogenic (unable to cause severe disease) or they are killed (unable to replicate).
Following this initial exposure to the viral and/or bacterial antigens contained
in the vaccine, large numbers of B cells and T cells specific to these antigens will distribute themselves throughout the body's lymphoid tissues, ready to be there to
defend against an infectious organism, where ever it may appear. They will then go dormant
in these lymphoid tissues, until recognised antigens from an infectious disease-causing organism or a vaccine-organism come along to reactivate them. These B and T cells are termed 'memory cells' because they
effectively 'remember' the antigens that the body has fought before.
For a period of time, following vaccination, antibodies produced in the response to that
first vaccination will also circulate throughout the body, ready to encounter and
protect against foreign disease invaders. With some vaccines, the amount of antibody
produced following that initial vaccination will be moderately low and the levels of
antibody (mostly IgM antibodies which are the shorter-lived antibody types generally made by plasma cells when they first encounter a new organism) circulating in the body will dwindle away quickly within a few months (not be long-lived).
It is when the second (and third) vaccinations are given (1 month and then 2 months later)
that the huge populations of 'memory B cells' activate and produce the massive levels of longer-lasting antibodies (IgG type) required to achieve year-long (up to 3-years duration with
some of the new immunizations) humoral protection. This is the main reason that puppies and kittens and older animals getting vaccinated for the first time generally receive a 'course' of two or three vaccinations 2-4 weeks apart: it is to build up their levels
of antibodies against the foreign pathogens such that these antibody levels will provide them with protection for at least a year to 3-years. It is also why we test antibody levels
when determining whether or not an animal requires re vaccination.

4. Frequently Asked Questions:
If the immune system is designed not to attack 'self' antigens contained on
normal body cells, how come the immune system kills tissue cells containing viruses?
The reason behind this is that the tissues of the body are quite smart. Many cells
will take antigen pieces of an invading organism (such as a virus) and present
them on the outer surfaces of their cell membranes. This foreign antigen sitting
on the surface of a cell notifies the immune system (especially cells such as
cytotoxic T cells) that the cell has been invaded and triggers the immune system
to kill it.
Some invading organisms leave their own antigens on the surfaces of cells when they invade (i.e. the mistake is made by the organism, not the cell). This results
in a similar situation - the immune system kills the invaded cells.
Note - some clever bacteria (e.g. some Streptococcus types, Rhodococcus, Mycobacteria) and viruses
avoid detection by the immune system by hiding out in cells, including some inflammatory cells, where the immune system can not detect them. This results in long-term, difficult to clear infections (a lot of antibiotics can not get inside cells).
 5. Live vaccines (also termed live virus, live attenuated and avirulent vaccines)
5. Live vaccines (also termed live virus, live attenuated and avirulent vaccines)
A live vaccine is vaccine containing whole, live viruses (and/or bacteria). These viruses are non-dangerous
strains of virus which are very closely related to the wild-type, disease-causing
viruses that we are trying to protect our pets against. These viruses have many of
the exact same antigens (proteins/sugars that the immune system must recognise as foreign to trigger an attack) present on their surface that the disease causing organisms do
and, as a result, the antibodies and memory T and B cells created following the vaccination will be able to protect the animal against the dangerous viral (and bacterial)
organisms that bear those same surface antigens.
When these vaccine viruses are injected into the animal, they multiply within the
cells and tissues of the animal, growing to large populations. It sounds terrible, but it is actually a good thing that they do multiply: greater numbers of viral
particles mean that the immune system will be exposed to greater volumes of viral vaccine antigens. A greater immune response will be triggered to 'kill' off these
millions of viral antigens and the end result will be higher levels of protective antibodies
floating through the blood and greater numbers of memory T and B cells waiting to
protect the body in the face of attack with a real, disease causing organism.
It is because of this greater immunoprotective response to the live vaccines, that live
attenuated vaccines are preferred over killed-type vaccines for immunizing normal
animals where possible. There are, however, times when a live vaccine is contraindicated
(unsafe to use) and organisms for which the creation of live vaccine is not possible or safe (see contraindications section below)..
The reason that the young animal with the naive immune system (immune system that has
never encountered the particular viral antigen before) does not get sick as a result
of the vaccination with live, infectious vaccine virus is that the viruses used in
the vaccines are avirulent strains. This means that, although they
can multiply and infect the cells of the cat or dog in a similar fashion to the
nasty forms of virus that exist in the environment, they differ enough in infectivity from their wild-type, disease-causing relatives that they are generally unable to cause severe disease signs in animals with a normal immune system. For example, the avirulent
viruses may not replicate as fast or they might not access cells as quickly as the wild-type viruses
and, thus, they will not have had as much chance to cause severe disease by the time
the immune system catches up (around 2 weeks for a naive immune system).
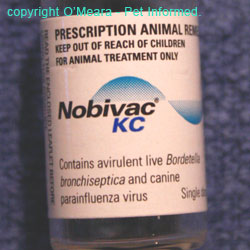

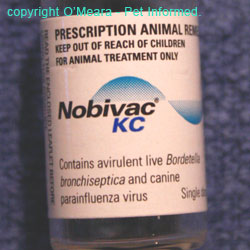
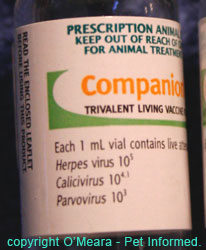
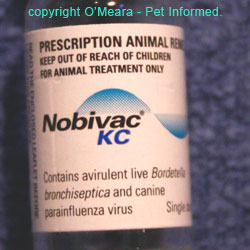
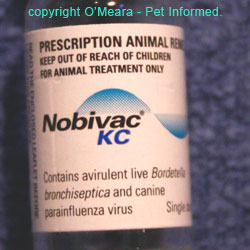
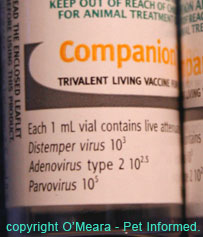
Images of various vaccine bottles, showing the terms used (avirulent, living, live etc.) to indicate live attenuated vaccines.
How do manufacturers make viruses non-harmful for the purposes of vaccination?
Scientists design these avirulent strains of virus for vaccines in many ways:
1) selecting strains that preferentially grow in (have adapted to) the cells of animal species different to the one we are vaccinating (e.g. using viruses
that like mouse cells more than dog cells) - i.e. they are less adapted to and
thus less able to cause disease in the dog cells.
2) storing the viruses for a long time (aged viruses are less adept at causing disease).
3) they can also now use fancy technologies such as putting parts of the DNA of the infectious-disease virus (the parts that code for the viral antigens that the immune
system needs to recognise to protect the body against wild-type viruses) into the
'body' of a different species of avirulent live carrier virus such that, the antigens of
the infectious disease virus will be produced (and exposed to the animal immune system)
by the carrier virus when it replicates.
Sometimes, just inoculating the animal with a live, semi-virulent virus in a site of the body that is different to the one the organism usually favours for replication, can result
in a protective immune response and minimal clinical side effects. For example, the feline respiratory viruses (feline herpes, feline calicivirus) preferentially infect the cells of the respiratory tract. When they infect these cells, they cause disease (cat-flu). If the viruses are placed in a vaccine and injected into the skin ( a site they would not normally attack), the immune system will attack them and acquire immunity towards the wild-type, disease-causing cat-flu viruses, but the cat should not exhibit signs of disease towards the vaccine.
What are the contraindications of live virus vaccines?
Because live virus vaccines do invade the cells of animals and replicate, it is possible for them to cause disease eventually, should the immune system not come along at some point to destroy them.
After all, endless viral replication, even of avirulent strains of virus, will eventually
prove harmful. As explained above, these viruses do cause cell damage during replication
in the body, it is just that they do it so much slower and less effectively than the wild-type viruses
do (consequently, the 1-2 week delay in immune response that occurs when a normal, but naive immune system first meets a live vaccine virus will not usually be a problem - the avirulent
viruses should not get a chance to do a lot of damage in this period of time).
Live virus and bacterial vaccines are considered unsafe in animals
in which an immune system response is unlikely to be forthcoming or normal. These include:
- animals with proven genetic immunodeficiencies (i.e. born without certain functional parts of the immune system).
- animals with acquired immunodeficiencies - this includes animals on chemotherapy; cats with FIV (no T cells) and animals with bone marrow suppression and low white blood cell counts.
- unwell animals. When an animal is vaccinated, lots of white blood cells are consumed in fighting
the vaccine 'infection'. These white cells (especially the non-antigen-specific 'soldier' cells)
are thus not available for use elsewhere in the body, should another infection arise somewhere. If an animal is unwell or brewing an infection somewhere, then all of its immune cells will already be invested in battling the infection or trauma already afflicting the animal. If you then go and vaccinate this animal, cells will need be to diverted away from the site of disease to the vaccine site. This
loss of 'troops' from the site of disease could well result in the disease becoming worse
due to there being less inflammatory cells available to fight it.
- animals with a fever (some immune cells will not respond normally to an antigen in the presence of fever making
vaccination, at best, ineffective and, at worst, harmful).
- animals with a subnormal / low temperature.
- newborn animals that did not get their colostrum. Although live vaccines are fine for use
in animals over 4 weeks (which have a functional, though naive immune system) and newborn animals
protected by their mother's colostrum, newborn animals
(termed neonates) unprotected by maternal antibodies have a greatly reduced immune response
(not much better than the late-stage fetus) and live vaccines may produce disease in them.
Animals that have had previous allergic reactions to live vaccines should not be
given the same ones again.
Because many of these viruses like to replicate in rapidly-dividing cells, they will
tend to preferentially infect tissues where cells are dividing quickly. This includes the
dividing cells of fetuses. Live vaccines have the potential to cause birth-defects,
abortion and stillbirth and are contraindicated in pregnant bitches and queens.

6. Killed vaccines (also termed inactivated vaccines) and subunit vaccines:
Killed vaccines are vaccines comprised of whole viruses (often wild-type, disease causing viruses)
which have been inactivated (killed). They are unable to replicate in the body of the animal and unable to cause disease in the animal, but they contain all of the viral and/or bacterial antigens on their
surface that the immune system needs to recognise in order to protect the animal
against future encounters with wild-type, disease causing organisms.
Subunit vaccines are similar in function to killed vaccines (in fact, they are a form of killed virus vaccine).
With subunit vaccines, the scientists who design and manufacture vaccines study the wild-type disease-causing
viruses and bacteria in order to identify and isolate those areas of the virus (antigens) which either:
1) enable the virus to attack our pets (e.g. surface antigens used by the virus to attach to and invade cells of the body - antibodies made against this would bind up the antigen protein and
thus prevent a virus from invading) OR
2) which are found to trigger the greatest response by the animal's immune system
against the virus (some proteins/sugars on the surface of a virus are considered 'highly
antigenic' meaning that the presence of the protein triggers a strong immune
reaction against that protein/sugar from the body's immune cells).
The scientists replicate just those antigens of the virus/bacteria which have these desirable traits, package them all into a vaccine with some other immune-stimulating
additives and this is the 'killed subunit vaccine' we inject into your pet.
The principle of subunit vaccines (exposing the animal's immune system to the antigens of infectious organisms in order to induce a protective immune response) is the same as for the whole virus live and killed vaccines, only the technology is lot more targeted and precise. With the whole virus vaccines (live and killed), a lot of what is being injected is virus matter that will never be 'seen' by the immune
system. For the purpose of vaccination, it is 'junk'. After all, all we really need to expose the immune system to, in order to induce a protective immune response, are those particular surface antigens (shared by the wild-type viruses) that the memory cells and
antibodies must recognise and target in order to destroy wild-type viruses. By only
being comprised of those important viral antigens, subunit vaccines are essentially getting rid of the 'junk'. This reduces the amount of unnecessary foreign particles
being injected into the animal and, hopefully, reduces the risk of some of the side effects (e.g. anaphylactic reaction) commonly encountered with killed vaccines.
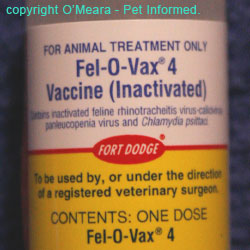
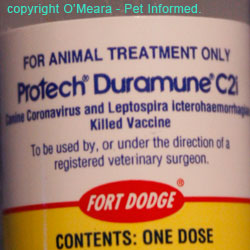

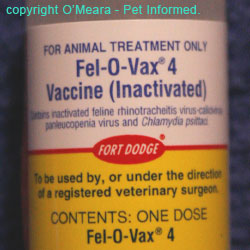
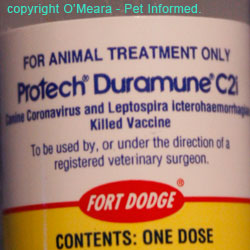
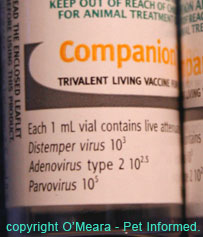
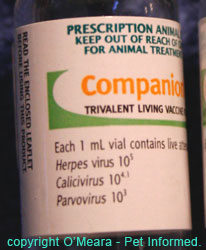
Images of various vaccine bottles, showing the terms used (inactivated, killed etc.) to indicate killed vaccines.
You are probably by now wondering, "If killed vaccines (inactivated or subunit) have all of the antigens needed in order to induce an immune protective response and they do not replicate in the animal and cause disease, why don't we just use killed vaccines all the time?"
The reason for this was touched on in the live vaccine discussion. When we inject a killed (or subunit) vaccine into the body, it does not replicate. It just stays in one spot for the immune system to 'kill'. Without replication of the virus, the immune
system does not get exposed to the massive amounts of antigen generated by live viruses when they replicate. This results in poorer humoral immunity (fewer memory B cells
and smaller amounts of antibody that don't last in the body as long) and poorer cell mediated immunity
(not as many memory T cells waiting by to target the next wild-type virus that comes along).
The only way that the humoral and cell-mediated immunity can be improved is by:
1) putting massive quantities of killed virus or bacteria matter into each inactivated vaccine. This increases the amount of antigen available for the immune system to recognise, but
increases the risk of allergic reactions and also local, inflammatory injection site reactions.
2) adding additives to the vaccine (termed adjuvants) which are designed to increase
the effectiveness of the immune response to that vaccine. These adjuvants are not
all benign and, being highly immune-stimulatory, they can increase the risk of allergic reactions, anaphylaxis, injection site reactions and even feline vaccination
associated fibrosarcomas.
What are the contraindications of killed virus vaccines?
Because killed virus vaccines do not invade and replicate within the cells of animals,
they are unlikely to cause disease in immunosuppressed animals or pregnant
animals or newborn animals (neonates) that failed to get their colostrum. In fact, many of the killed vaccines have, as part of their recommendations sheet,
a statement saying that they are safe for use in animals which are pregnant
or which have immunodeficiencies.
The one major issue I have with the use of killed vaccines in immunocompromised animals
is that, even though these vaccines might be safe to give to immunodeficient animals, if an animal has a poor immune system will it actually be able to respond to the vaccine in order to gain protective immunity? It is possible that vaccines given to immunosuppressed
patients and FIV cats (ones which already have proven immunodeficiency and low T cell counts) may be doing very little.
Other situations in which a killed vaccine might be ineffective (due to a poor immune response)
include animals with a fever and animals with subnormal temperatures. Obviously, if these animals were also sick (already diseased), the vaccine might even be unsafe
(contraindicated) to use (see next part - contraindications of killed vaccines in sick animals).
Killed vaccine contraindications:
- Unwell animals. When an animal is vaccinated, lots of white blood cells are consumed in fighting
the vaccine 'infection'. These white cells (especially the non-antigen-specific 'soldier' cells)
are thus not available for use elsewhere in the body, should another infection arise somewhere. If an animal is unwell or brewing an infection somewhere, then all of its immune cells will already be invested in battling the infection or trauma already afflicting the animal. If you then go and vaccinate this animal, cells will need be to diverted away from the site of disease to the vaccine site. This
loss of 'troops' from the site of disease could well result in the disease becoming worse
since there are less cells available to fight it.
(Note - this immune-suppressive effect
of vaccination is nowhere near as much of an issue with killed vaccines as it is for live vaccines.)
- Sick animals with a fever
- Sick animals with a subnormal / low temperature.
Animals that have had previous allergic reactions to killed or subunit vaccines should not be
given the same ones again.
Note: some killed vaccine labels indicate that they are unsafe to use in pregnant bitches
(e.g. some of coronavirus vaccines, some of the leptospira vaccines). This contraindication
is probably not due to the infectious organism (after all, it is dead), but some other component
of the vaccine (e.g. an adjuvant chemical) that is unsafe for fetuses.

7. Live vaccines versus killed vaccines: the pros and cons of each.
Live vaccines - benefits:
1) More amplified and longer lasting humoral and cell mediated immune responses - resulting in better, longer lasting immune protection.
2) More rapid induction of immunity.
3) Only a small amount of viral material needs to be injected because it replicates in the body. Less viral
material means a reduced risk of allergic and injection site reactions.
4) New vaccines produced can achieve long-lasting antibody (12 months - 3 years) after only a single dose.
5) No adjuvants required, reducing the risks of allergic and injection site reactions.
6) Live vaccines can be produced that can be given by routes other than injection (e.g. intranasal vaccines) - see next section.
This means that vaccines can potentially be tailored to induce immunity in the areas of the body where immune protection will be most effective (e.g. immunity in respiratory system to protect
against respiratory viruses ... makes sense.)
7) From a company viewpoint, they cost less to produce (this cheaper price might then, hopefully, be passed onto veterinarians and then pet owners).
Live vaccines - potential problems:
1) Because the virus is alive, it has to be stored carefully or the virus can die and become ineffective.
2) Potential to cause disease in immunocompromised or pregnant animals.
3) Certain live vaccines can cause severe complications: e.g. live rabies vaccines can cause
fatal neurological disease in some dogs and cats.
4) Vaccines that have not been produced properly and undergone adequate quality control may
contain virulent organisms which could produce severe disease (this is very rare).
5) Some live vaccines, if given by the wrong route, can cause severe illness (e.g.
injectable cat flu vaccine viruses that accidentally get inhaled by a cat will produce marked signs of cat-flu and
intranasal Bordetella vaccine viruses that get injected can cause liver damage and death of the animal).
6) Live vaccines tend to 'take up the time' of a lot of the body's white blood cells, leaving fewer white blood
cells available to fight other infections. This relative immunosuppression may leave the body less defended and thus more vulnerable to other diseases during the period of time that the vaccine is present. This is less of
a problem with killed vaccines.
7) A lack of preservatives in these vaccines means that their shelf life might be shorter.
Killed vaccines - benefits:
1) Unlikely to cause disease in immunocompromised or pregnant or newborn animals (though the response
to vaccination in immunosuppressed individuals might be low).
2) Do not tend to cause the same relative immunosuppression and vulnerability to other diseases that the live vaccines do.
3) They store for longer periods.
Killed vaccines - potential problems:
1) Poorer, shorter-duration cell-mediated and humoral immunity (unless lots of virus particles and/or adjuvants are included).
2) Greater risk of causing allergic reactions and injection site reactions because of the presence of large volumes of virus material and/or adjuvants.
3) Some products are not safe for use in pregnant animals.
4) Most require a minimum of two doses to achieve the desired effect (risk of vaccine reaction with the second dose).
5) They are generally more expensive to produce.
6) Must be given by injection (not available in other routes of administration - intranasal etc.)

8. Different routes of administration of vaccines (e.g. intranasal vaccines).
Some of the live attenuated vaccines can be given by routes other than subcutaneous (under the skin) or
intramuscular (into the muscles) injection. The use of alternative routes of administration is designed to
1) improve the protective immune response of the animal by inducing protective immunity at the very places in the body that certain viruses and bacteria are likely to target (e.g. the respiratory viruses attack the respiratory tract: intranasal
vaccines are great at inducing protective immunity in the respiratory tract)
2) reduce the side effects of the vaccine by either slowing the rate of uptake of the antigens (e.g. intranasal vaccines are taken into the body more slowly than injectable
vaccines, thus reducing the risk of allergic reaction) or by administering the vaccine viruses to
an area of the body that they do not typically grow in (thus reducing the disease-causing
effects of some of the strains of live vaccine viruses)
3) improve the ease of administration (some animals don't mind intranasal or conjunctival vaccines as much as needles)
Intranasal Vaccines.
Intranasal vaccines are the most common alternative route of vaccine administration encountered
in veterinary practice. Intranasal vaccines are avirulent, live virus strains that are given up the nostrils of the animal using a special applicator (pictured). The vaccine virus
coats the cells lining the upper respiratory tract (nasal passages, throat, trachea) and replicates in these cells. The immune cells present in the respiratory tract attack these viruses (and/or bacteria), inducing a protective immune response that tends to remain within or near the respiratory tract
(e.g. protective antibodies actually get secreted onto the surface of the respiratory tract cells during this immune response to the vaccine).

When a wild-type, pathogenic, respiratory virus or bacteria (e.g. kennel cough, cat-flu) comes along,
it will usually access the body via the respiratory route (these organisms are usually
inhaled by a potential 'host' when another, infected animal coughs: each cough contains
millions of aerosolized infectious particles). If the animal has received an intranasal vaccine previously, the lining of its respiratory tract will be coated with protective
antibodies and the regional, respiratory-system lymph nodes will contain hundreds of memory cells
all primed to recognise the antigens contained on the invading respiratory viruses. As soon as the invading viruses and bacteria reach the respiratory tract, these antibodies and memory cells will react and kill them off, a response that will be so much quicker than
that seen with an injectable vaccine because, with intranasal vaccination, the immune defenses produced are
located in the same region as the invading pathogens. As a result, the invading viruses will not get the opportunity to damage many cells and clinical signs of disease should not occur or, if they do, they should be very mild.
Diseases for which intranasal vaccines are available:
- kennel cough (Bordetella, parainfluenza +/- the respiratory form of canine adenovirus)
- cat flu (feline herpes virus, feline calicivirus, feline Bordetella)
- In the USA, Heska has brought out an intranasal vaccine that contains panleukopenia (a gut organism)
- In the USA, Canada and Europe, Pfizer has brought out an intranasal vaccine against
feline coronavirus - a common virus that is a precursor to the development of the highly
fatal disease, FIP.

Advantages of intra-nasal vaccines:
- they induce much better protection against respiratory tract viral and bacterial
infections (such as kennel cough and cat flu) than injectable vaccines do.
- some types can be given to pregnant bitches and to puppies as young as 4 weeks.
- only a single dose is required to induce immunity each year.
- they are less likely to cause allergic reactions than injectable vaccines because the
uptake of viral antigen into the body is slower.
Disadvantages of intranasal vaccines:
- they can often induce a mild upper respiratory tract infection, characterised by
watery nasal and ocular discharge, sneezing and even coughing. It is usually self limiting and
very mild and should not be confused with vaccination failure.
- many dogs and cats violently dislike intranasal vaccines (esp if they are given cold). They
squirm and will often sneeze violently after administration.
- they are generally only effective against respiratory pathogens (aside from a few feline intestinal organisms).
- intranasal vaccines are needed every year (note that this goes for any vaccine used against
respiratory pathogens, not just intranasal ones).
- intranasal Bordetella vaccines accidentally injected can cause severe liver
damage and even death of the animal.
Alternative Routes:
Aside from the intranasal route of vaccine administration, few other non-injectable routes
exist for which vaccines are commercially available. Currently, vaccine companies are
investigating ways of improving the response of the gastrointestinal immune system towards diseases
like parvovirus and coronavirus through the use of orally-administered vaccines and intraperitoneally-administered
(vaccines given into the abdominal cavity) vaccines. They are also trying to achieve
injection-free vaccination through the use of dermal patches and sprays (vaccines applied to the skin surface)
and transdermal vaccines (aerosolized vaccine particles that are forced at high-pressure through the skin using special instruments, thus avoiding the need for needles). Currently one company, Merial, is producing commercially available feline leukemia vaccines in a needle-free transdermal form.

To go from this How Do Vaccines Work page to the Homepage, click here.

References and Suggested Readings:
1) Prevention of Infectious Diseases. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
2) Greene CE, Immunoprophylaxis. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
3) Resistance of the Body to Infection: II. Immunity and Allergy. In Guyton AC, Hall JE, editors: Textbook of Medical Physiology, Philadelphia, 1996, WB Saunders Company.

Pet Informed is not in any way affiliated with any of the companies whose products
appear in images or information contained within this article. The images, taken by Pet Informed, are only used in order to illustrate certain points being made in the article.
Copyright 2008, www.pet-informed-veterinary-advice-online.com.
All rights reserved, protected under Australian copyright. No images or graphics on this Pet Informed website may be used without written permission of their owner, Dr. O'Meara.
Nobivac and Companion C3 are registered trademarks of Intervet.
Protech, Duramune, Fort Dodge, Bronchi-Shield and Fel-O-Vax are registered trademarks of Wyeth and Affiliates.
Any dose rates mentioned on these pages should be confirmed by a vet. Dosing rates for common
drugs are being changed and updated all the time (e.g. as new research comes in and as drug
formulations change) and information here may not remain current for long. What's more, although we try very hard to maintain the accuracy of our information, typos and oversights do occur. Please check with your vet before dosing any pet any medication or drug.
 When an animal (or human) is vaccinated, a veterinarian injects a small amount of a virus or bacteria (or other infectious agent) under the skin of the animal. This organism that gets injected
is generally a non-harmful strain of the virus or bacteria that we are protecting our pets from
(live vaccine) or a killed form of the actual wild-type, disease-causing virus or bacteria. The injection may contain live organisms (termed a live vaccine); inactivated organisms, incapable
of replicating in the body (termed a killed vaccine) or just little bits of the organisms: specific proteins or sugars (termed antigens) that the immune system will recognise as foreign to the body
(vaccines made of bits of an organism are termed a subunit vaccines and are a form of killed vaccine). As will be discussed in the killed vaccine section, killed vaccines and subunit vaccines
are generally less immune-stimulatory (less capable of inducing immune reaction) than live vaccines
and so additives (termed adjuvants) which enhance the immune system's response to the vaccine
are generally added to the killed vaccines to improve their effect.
When an animal (or human) is vaccinated, a veterinarian injects a small amount of a virus or bacteria (or other infectious agent) under the skin of the animal. This organism that gets injected
is generally a non-harmful strain of the virus or bacteria that we are protecting our pets from
(live vaccine) or a killed form of the actual wild-type, disease-causing virus or bacteria. The injection may contain live organisms (termed a live vaccine); inactivated organisms, incapable
of replicating in the body (termed a killed vaccine) or just little bits of the organisms: specific proteins or sugars (termed antigens) that the immune system will recognise as foreign to the body
(vaccines made of bits of an organism are termed a subunit vaccines and are a form of killed vaccine). As will be discussed in the killed vaccine section, killed vaccines and subunit vaccines
are generally less immune-stimulatory (less capable of inducing immune reaction) than live vaccines
and so additives (termed adjuvants) which enhance the immune system's response to the vaccine
are generally added to the killed vaccines to improve their effect. 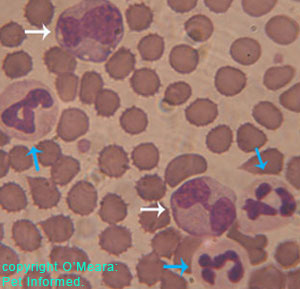
 2) Those cells that are antigen-specific in their responses. Certain lines of cells are designed to only mount a response against certain specific, recognised antigens that are present on
the surface of organisms, foreign bodies and other invaders and that are different (foreign) to antigens
present on the body's own cells. Termed T lymphocytes and B lymphocytes (see definition section and image opposite), large populations of each of these antigen-specific cell types are present in the body at birth.
During the young animal's time in utero, every one of these cells is carefully screened by the embryonic immune system, to ensure that they recognise the antigens present on the body's cell surfaces as 'self' (and thus not attack them) and to ensure that they can detect the differences between these 'self' antigens and the 'non-self' antigens present on foreign invaders (these antigens are sufficiently different from the 'self'
antigens contained on the body's cells that the lymphocytes will bind to them and
induce an immune system attack against them). It is these cells - the lymphocytes - that are of most importance when talking about vaccination.
2) Those cells that are antigen-specific in their responses. Certain lines of cells are designed to only mount a response against certain specific, recognised antigens that are present on
the surface of organisms, foreign bodies and other invaders and that are different (foreign) to antigens
present on the body's own cells. Termed T lymphocytes and B lymphocytes (see definition section and image opposite), large populations of each of these antigen-specific cell types are present in the body at birth.
During the young animal's time in utero, every one of these cells is carefully screened by the embryonic immune system, to ensure that they recognise the antigens present on the body's cell surfaces as 'self' (and thus not attack them) and to ensure that they can detect the differences between these 'self' antigens and the 'non-self' antigens present on foreign invaders (these antigens are sufficiently different from the 'self'
antigens contained on the body's cells that the lymphocytes will bind to them and
induce an immune system attack against them). It is these cells - the lymphocytes - that are of most importance when talking about vaccination.