Veterinary Advice Online: Kennel Cough in Dogs.
The information contained within this article covers a range of topics written to fully educate pet owners about kennel cough in dogs (a disease otherwise known as canine infectious
tracheobronchitis, canine cough, canine croup, canine parainfluenza and canine
Bordetella infection). The information presented is detailed (but still easy to understand) because we are
aiming to educate owners thoroughly about the disease, including its transmission, treatment
and prevention, and provide owners with enough information that they might be better informed and able to troubleshoot problems with their own pets. The topics are covered in the following order:
1) What is kennel cough? - a basic overview of the disease.
2) Which animals are at risk of contracting kennel cough pathogens?
2a) Kennel cough in dogs (includes information on kennel cough vaccine failure in dogs).
2b) Kennel cough in humans and other animals (includes info on cat-flu and human infections).
3) How do animals catch kennel cough? - this section contains information about where and how animals can catch kennel cough; the high risk environments and whether kennel cough vaccines can cause disease.
3a) Virus transmission from dog to dog.
3b) What environmental conditions predispose to kennel cough transmission?.
3c) Real-life situations that promote dog to dog transmission of kennel cough.
3d) Can a neighbourhood dog or a visiting dog give my dog kennel cough?
3e) My dog hasn't been near another dog in months - how could he get kennel cough?
3f) Can vaccines cause kennel cough?
4) Symptoms of kennel cough - what does kennel cough do to your dog? This section contains the following subsections:
4a) How kennel cough viruses cause disease (how they replicate and destroy cells etc.).
4b) How do kennel cough primary and secondary bacteria cause disease?
4c) Symptoms of kennel cough: how does kennel cough affect the respiratory tract and mucous membranes?
4d) Chronic, recurrent kennel cough infections - kennel cough that keeps coming back.
4e) Can animals be infected with kennel cough and show little or no signs of disease?
5) How is kennel cough diagnosed? This section discusses the diagnostic modalities
used by veterinarians in order to test animals for the various causes of coughs and respiratory illness.
It contains information on findings that might be expected in animals with kennel
cough and the pitfalls that might be encountered with the testing procedures. This section contains
excellent photographs.
5a) Blood panels and urine testing.
5b) Chest radiographs (x-rays).
5c) Bronchoalveolar lavage (BAL): cytology, culture and sensitivity.
5d) Endoscopy or tracheoscopy.
5e) Kennel cough virus isolation.
6) What other diseases look like kennel cough? The differential diagnoses for kennel cough.
7) How is kennel cough treated?
7a) Antibiotics.
7b) Cough suppressants.
7c) Anti-inflammatories.
7d) Nebulisers and shower therapy.
7e) Isolation.
7f) Rest.
7g) Environmental management.
7h) Beware of neck pressure and collars.
7i) What happens if you don't treat? Is not treating for kennel cough an option?
8) What is the prognosis for kennel cough?
9) How to prevent kennel cough in pets. - this section contains excellent general advice on the prevention of canine cough for pet owners. It includes detailed information about vaccination schedules and vaccine types (intranasal vaccines, injectable vaccines) and many great tips
for reducing your pet's exposure to kennel cough viruses and/or bacteria.
10) How to prevent kennel cough in high risk situations. - this section contains useful tips and hints
for preventing and controlling canine cough infection and spread in situations with high viral/bacterial contamination
and high dog numbers (e.g. breeding facilities, dog clubs, boarding kennels).
11) How do you disinfect the environment following kennel cough contamination?
12) Summary and take home messages - a summary of the important points.
WARNING - IN THE INTERESTS OF PROVIDING YOU WITH COMPLETE AND DETAILED INFORMATION, THIS SITE DOES CONTAIN MEDICAL AND SURGICAL IMAGES THAT MAY DISTURB SOME READERS.

1. What is Kennel Cough?
Kennel cough, otherwise known as canine cough, canine croup, canine infectious tracheobronchitis, canine parainfluenza infection, canine Bordetella bronchiseptica infection
and even, I have heard,'canine whooping cough' is a common respiratory disease affecting dogs, and related canine species, all around the world. Canine cough is
a multifactorial disease caused by a variety of infectious disease organisms that attack the upper respiratory tract (throat, nose, trachea and bronchi) and exacerbated by numerous non-organism factors such as poor-ventilation, overcrowding, low-immunity, high stress, high dust levels and dry air conditions (low humidity). Common organisms implicated in kennel cough infections include the primary infectious disease organisms: parainfluenza 2 virus, canine adenovirus type 2, Bordetella bronchiseptica (a bacteria) and various mycoplasma species as well as a range of secondary bacterial organisms including: Pasteurella, Staphylococcus, Streptococcus, Bordetella, Mycoplasma, Escherichia coli (E. coli), Klebsiella and Pseudomonas. Occasionally, canine
herpesviruses, reoviruses, canine adenovirus type 1 and even canine distemper virus have
been associated with kennel cough symptoms in dogs.
Kennel cough is generally spread in conditions whereby large numbers of dogs
are kept in close proximity to each other (pounds, shelters, pet shops, boarding kennels, breeding facilities, dog clubs, dog shows and multiple-dog households). Usually appearing
in unvaccinated (and even vaccinated) dogs 3-10 days after exposure to infected dogs, the disease is characterised by infection and inflammation of the upper airways. Affected dogs
develop a fever; enlarged throat and neck lymph nodes (generally not appreciated by
their owners) and a cough. This cough is harsh and hacking (often described as 'honking' or 'hoarse') and severe, explosive bouts of coughing will often be followed with a gagging, retching action (expectoration), whereby the dog looks like it is attempting to bring something up. The pet may indeed bring up something (a patch of white foam or phlegm) but, more commonly, the animal will swallow the expectorant
and you won't see anything brought up. Bouts of coughing can often be so severe and persistent
that owners will fear their dog is choking and/or unable to catch its breath!
The severity and frequency of the coughing is often exacerbated by dry air conditions, heavy panting, exercise (exercised dogs pant dry, irritating air across their inflamed airway linings) and pressure on the throat (e.g. the owner pulling on a lead and collar). A watery nose and or eye discharge may also be seen. Generally, most animals affected with canine cough will still appear to be bright and active and healthy-looking to their owners, despite the nasty cough, however, some animals may become more sleepy and lethargic than normal and go off their food a bit, as a result of the fever and illness. Generally the disease is self limiting (it usually goes away on its own in 7 to 10 days) but, occasionally, some dogs will progress to severe secondary complications, including pneumonia
or chronic, long-term airway infection and irritation (a harsh cough that, quite simply, won't go away).

2. Which animal species are at risk of contracting kennel cough?
2a) Kennel cough in dogs:
Kennel cough is a disease that can infect dogs of all ages. Mild to moderate clinical
signs are typically seen in older dogs (over 6 months) that have good, up-to-date immunization.
The most severe clinical signs (including pneumonia) are typically seen in young puppies (under 4 months of age),
immunocompromised animals and unvaccinated animals.
It is possible for dogs and puppies that have been vaccinated before to contract the disease following exposure to causative infectious disease organisms in multiple-dog environments (boarding kennels, pounds etc).
There are many reasons for the 'vaccination failure' that can occur with kennel cough vaccines:
1) Not all organisms that cause kennel cough are vaccinated for.
Most kennel cough vaccines only cover our canine friends against parainfluenza 2, Bordetella bronchiseptica and occasionally canine adenovirus type 2. Vaccines do not cover against
any of the other infectious agents that are known to cause or contribute to kennel cough.
2) Infectious agents (e.g. parainfluenza virus) can mutate and change.
Vaccines protecting against one wild-type strain of a virus (or a bacterium) may not protect the animal as well against a different strain of the same organism.
3) The nature and site of the kennel cough infection versus the immune response that occurs with vaccination.
Respiratory viruses (and bacteria) affect the lining of the respiratory tract. Antibodies
and kennel-cough-targeting immune cells, produced following injectable vaccinations, tend to circulate in the blood and lymphatic systems, not within the air passages of the lungs themselves (where the bugs
invade). Thus, it can take some time for the immune response to be able to mobilise into the airways of the dog, following kennel cough infection: this delay gives the organisms a head start in creating damage and airway irritation and, as a result, clinical signs of kennel cough tend to be seen.
Note that the immune defensive response towards kennel cough invaders tends to occur faster with intranasal vaccines, leading to less vaccine failure with this route of vaccine administration (see section 9a on vaccines for kennel cough).
4) Kennel cough is often misdiagnosed.
There are a lot of diseases that mimic
kennel cough (see section 6). It is common for vets to diagnose a coughing condition
as kennel cough (even in a vaccinated animal), when the illness might, in fact, be something else entirely.
5) Immune suppression in stressful situations.
Vaccines have no benefit if the vaccine-induced immune system response is suppressed - i.e. you can have a perfectly immunized dog, with great levels of anti-kennel-cough antibodies and immune cells in its body, that is unable
to mount a response against a kennel cough infection because its immune system is depressed. This immune suppression is not always a result of a severe immune-suppressive disease
or immune suppressive drugs, either. Low-grade immune suppression (enough to let kennel cough symptoms show) can occur simply under conditions of high stress - the kind of
stresses that can be experienced by most dogs placed in new environments
(e.g. kennels, pounds, areas away from their familiar home) and/or unsuitable
environments (e.g. draughty, dusty conditions, poorly-ventilated conditions),
surrounded by unfamiliar, threatening dogs. The number of stress factors ... it is really no wonder that vaccinated pets come home from pounds or boarding kennels with kennel cough!
There are many other causes of vaccine failure and these are discussed on our
great vaccination failures page.
So why do we vaccinate against kennel cough then, if the vaccines don't work?
Hold on a second! Who said that kennel cough vaccines don't work?
Regardless of their imperfections, kennel cough vaccines still do a great job of protecting dogs from the many respiratory tract organisms that are capable of causing kennel cough. In reality, the vast majority of kennel cough infections go completely unrecognised by pet owners because of the complete lack of symptoms
seen or because of the mildness of the symptoms that do develop. This is proof that,
for the most part, the kennel cough vaccines are having their desired effect. Although kennel cough vaccines may not always 100% prevent animals from showing some signs
of infection (watery eyes and nose, a harsh cough), they are still essential because
they prevent animals from getting severe kennel cough symptoms (i.e. the kind of infection that can result in inappetence, dehydration and severe secondary complications,
including death). Vaccination can mean the difference between a dog with a mild to
moderate cough, that is still bright and eating well at home, and a dog that is very sick
with fever, breathing problems (including pneumonia) and in dire need of costly veterinary hospitalization and treatment (intravenous fluids, oxygen support etc.).
2b) Kennel cough organisms in humans and non-canine animal species:
Kennel cough viral organisms and other species:
The viral organisms implicated in canine infectious tracheobronchitis (including the ones we
vaccinate against) are quite specific to the canine family of animals. These respiratory dog viruses do not tend to infect animal species outside of the canine family.
For example, humans will not catch kennel cough viruses from their
canine pets and nor will they pass on their own viral 'flus' to their dog.
There are many viral organisms which are closely-related to the various kennel
cough viruses, however, that do cause respiratory disease symptoms in other species of animals (including
livestock, rodents and felines). For example, there are certain parainfluenza viruses that
cause respiratory disease symptoms in cattle and birds and there are a range of herpesviruses
that cause respiratory disease signs in pigs, cats, cattle, horses and birds. Instead of 'kennel cough', these infectious viral diseases are given other nicknames that are more specific to the host and situation involved (e.g. 'shipping fever' of cattle, 'cat flu' in cats). In many cases, the respiratory symptoms seen in these virus-infected animals closely mimic the signs seen
in dogs with kennel cough (harsh cough, eye and nose discharges, tracheal sensitivity and fever), however, these closely-related-virus infections may be more or less severe than the canine disease and they may also be associated with disease in organs other than the respiratory tract. The main thing to remember is that, although these other respiratory
virus diseases, seen in non-dog species, are closely related (both in terms of virus types and
symptoms) to kennel cough: they have not come to these animals from a dog.
Kennel cough bacterial organisms and other species:
The host-specificity of the viral organisms is not shared by the bacterial causes of kennel cough. It is possible for Bordetella bronchiseptica to spread between a number of different species including: dogs, cats (see cat flu discussion below), humans (see human discussion below), horses, swine, guinea pigs (cavies), rats, rabbits and even koalas, and for the bacteria to cause severe respiratory disease and even pneumonia in these creatures. The other secondary bacteria types commonly implicated in kennel cough infections (these are bacteria that secondarily invade and infect respiratory tissues which have already been damaged by the primary viral and bacterial causes of canine cough) including
Streptococcus species, Staphylococcus species, Pasteurella, Rhodococcus, Pseudomonas and several coliform species can also infect humans and other animals. Under the right conditions, these secondary bacterial species are also capable of producing severe respiratory and systemic
(body-wide) disease signs in humans and other animals.
Bordetella bronchiseptica and humans:
Bordetella bronchiseptica is a bacteria that has been known to infect humans,
in particular: small children, people with pre-existing respiratory and cardiac diseases
and immunocompromised humans (e.g. HIV patients, recipients of organ donations
and people with various causes of bone marrow suppression including leukemia, chemotherapy,
immune-mediated diseases and immune-suppressive drugs such as corticosteroids). The bacterium has the potential to cause severe respiratory disease (pneumonia, bronchitis, sinusitis) and even multiple organ infection in these people.
The bacteria typically spreads to humans via the air (in the form of bacteria-containing aerosolized
cough and sneeze secretions), during periods of close association with infected dogs, cats, rabbits and pigs. Transmission to humans is particularly high if the animals are living in overcrowded, dusty/dirty conditions with poor air ventilation and circulation. It is also possible for humans (generally immune-suppressed humans, infants and young children) to become infected by the bacteria used in the intranasal Bordetella vaccine, should it become aerosolized during a consult. For safety, high-risk people should not be present in the consultation room when the veterinarian gives the intranasal vaccine. (see section 9a
on human risks of intranasal Bordetella vaccination for more info).
The other thing to mention, dear reader, is that there are many other nasty fungal, bacterial and parasitic respiratory infections that can be transmitted from dogs to man,
which do not come under the topic of kennel cough. These non-kennel-cough infections will not be discussed further on this page (we are planning a zoonosis page down the track,
so please be patient). Whether or not you need to worry about human disease transmission from your pets comes with your vet establishing the correct diagnosis in the first place.
Kennel cough versus cat flu.
As mentioned above, the typical virus organisms that cause kennel cough in dogs do not usually infect cats (they are specific to dogs). Cats do, however, get their own combination of respiratory tract viruses (many of which are closely related to some of the kennel cough viruses) and these cause a syndrome called cat flu. Cats with 'cat flu' tend to present with fever, watery ocular (eye) and nasal discharges and sneezing. Sometimes, the catflu viruses can even affect the throat and trachea (upper airways),
causing symptoms very similar to that seen in dogs with kennel cough: harsh, violent 'spasms' of
coughing, gagging and retching, changes in voice and inappetence. This coughing condition is not a case of 'kennel cough' appearing in cats, but merely another variation of catflu presentation and clinical signs. The affected cat is likely to have caught the condition from another cat, not a dog.
The time that we do see a big cross-over between these two disease syndromes (cat flu
and kennel cough), in terms of the infectious organisms involved, is with Bordetella bronchiseptica. This bacteria is contagious between cats and dogs (and other species), but may, in some cases, be part of the normal bacterial population of the cat or dog throat (many non-symptomatic
animals have been found to have Bordetella in their airways). The bacteria is
known to be a major contributing factor in both cat flu and kennel cough and is thought
to be a primary disease agent in both diseases, not just a secondary invader.
Author's note: Vaccines are available for Bordetella in both dogs and cats.
Other secondary bacterial organisms commonly implicated in kennel cough infections (Staphylococcus, Streptococcus, Pasteurella, Pseudomonas and E coli) are also found in the airways of cats with catflu. It is likely that both species of animal (cats and dogs) already have these organisms present in their
mouths and airways (i.e. they are a normal part of the resident bacterial population),
rather than that they have spread from one animal to the next.

3. Kennel cough transmission - where do dogs get kennel cough from?
3a) How is kennel cough transmitted from dog to dog?
The respiratory viruses and bacterial and mycoplasmal organisms that contribute to kennel cough are present in the respiratory secretions (sputum, phlegm, snot etc.) of the nose, throat, large airways and lungs of the affected animal. When an affected animal coughs or sneezes, these respiratory secretions are blasted at high speed and pressure from the airways, into the air, as microscopic droplets of fluid (termed aerosols).
These aerosolised droplets contain thousands of infectious disease particles. A single
cough or sneeze can disperse these infection-containing droplets throughout a very large space, whereby they can infect a large number of other dogs.
Dogs become sick (become infected with kennel cough) if they inhale the aerosolised respiratory secretions of a dog infected with kennel cough. The infectious aerosolised droplets of fluid are so small that, when the next dog inhales them, they are capable of penetrating deeply into the nasal passages, throat, trachea and even the smallest air passages of the lungs.
Once inhaled, the infectious organisms invade and replicate within the cells lining these airway passages, damaging these cells in the process and causing local infection and inflammation of the airways. This results in symptoms
of coughing and sneezing and in the production of watery nose, throat and airway discharges. The coughing, sneezing
and watery discharges all shed replicated infectious disease particles into the environment and, consequently, the disease spreads and infects new hosts.
(Section 4 has detailed information on how viruses and bacteria replicate, damage cells and cause disease symptoms.)
Animals that are unvaccinated or inappropriately vaccine protected can also become infected if they ingest respiratory secretions contaminated with infective virus and bacterial particles. Such inadvertent consumption of infectious disease particles can occur if your pet eats or drinks out of (apparently clean) feeding dishes and water bowls that have been contaminated by a sick dog's respiratory secretions (e.g. nasal discharges). As an owner, you might
not even realise that there is contamination present. It is for this reason (the risk
of catching infectious diseases) that owners should be very careful about letting dogs eat and drink from the same unwashed feeding dishes, water troughs and standing water sources (pools, puddles etc.) as other animals.
It is also possible for dogs to ingest infectious viral and bacterial particles when they
lick the shoes, hands or clothes of a human that has been in hands-on contact with
an infected animal. Dogs that sniff and lick hands and clothes can leave infectious
secretions (e.g. snotty discharges) behind on those hands and clothes. They might even sneeze
or cough on those hands and clothes, coating them with infectious aerosols. The hands and clothes may appear visibly clean to the person, but still contain hundreds of organisms that are infectious to other animals (e.g. some aerosols are microscopic and invisible to the
naked eye). Dogs that bite and lick the fur of infected animals may also contract the
infection. Infected animals spread virus particles onto their own fur through licking their bodies (infectious respiratory secretions are transferred onto the coat in this way).
3b) What environmental and husbandry conditions predispose to kennel cough transmission?
Given that kennel cough is most commonly transmitted via the air (through infectious, aerosolized
respiratory fluids being ejected into the air via coughing and sneezing), it follows that
most dog to dog infections will occur when large numbers of dogs are placed in enclosed conditions in close proximity to each other. The larger the number of dogs, the more
likely it is that at least one or more dogs will be shedding the infectious particles that can infect others.
The more enclosed the conditions are (e.g. indoor facilities, facilities with poor air ventilation
and circulation), the more aerosolized particles are going to remain in the air around the animals waiting to be breathed in (instead of being quickly taken away from the animals
via the wind or ventilation ducting, where they can do no harm). The closer the dogs are to each other, location-wise, the more likely it is that infection from a sick dog will spread to others: the virus-laden aerosolised particles will have less distance to travel in order to find a new host.
Author's note: it is possible for dogs with kennel cough to infect animals that are located
in other rooms or locations. This can occur if animal handlers do not exercise appropriate levels of hygiene when handling other dogs (e.g. if handlers do not wash their hands
or change their clothes between handling infected and uninfected dogs, they can spread viruses
and bacteria from animal to animal). It can also occur if an air-conditioning or ventilation-ducting system is present that takes air from one region/room of a facility and distributes it to other rooms and areas containing dogs (infectious aerosols, carried aboard air currents, can be moved from room to room in this way). It can also occur in open-air settings if air-currents are in such a direction as to be able to blow infectious aerosols from one group of dogs to another group of dogs further downwind.
From an animal husbandry viewpoint, conditions with high dust levels; moderate to high humidity levels
(moist air); poor ventilation and air circulation; high levels of airborne irritants (e.g. high ammonia
levels, high disinfectant vapor levels) and conditions where animals are frequently exposed to
extremes of cold, heat, humidity (excessively wet or dry air), draughts, poor nutrition or changes in nutrition, overcrowding, excessive exercise fatigue and transportation all predispose to kennel cough manifestation and spread.
High dust levels:
High dust levels contribute to kennel cough for two reasons. Firstly, infectious aerosolized droplets attach to dust particles in the air, where they can remain infectious
for longer periods of time (dust protects fragile viruses from heat and drying out) and be easily inhaled by animals. Secondly, dusty conditions irritate and abrade the airways of animals, leading to airway lining damage - this results in inflammation and irritation of the airways, thereby worsening the signs of kennel cough. The damaged areas also provide a nice place for secondary bacteria to invade and grow and produce bigger infections.
High air humidity:
High air humidity levels do not irritate the airways as badly as dry air conditions do, but they do increase the risks of airborne infectious disease transmission because respiratory bacteria and viruses
tend to survive longer (hang around longer) in wet, humid environments and the infectious
aerosols are less likely to evaporate very quickly in wet conditions (thus they remain in the air longer and have
more opportunity to be breathed in).
Poor ventilation and circulation:
Poor ventilation and air circulation conditions are an issue because they contribute to higher dust levels in the air and they allow infectious, aerosolized particles to remain in the air, close by the susceptible animals, for longer (rather than being blown away from these animals by the wind or decent ventilation ducting).
Airborne irritants:
Airborne irritants (e.g. high ammonia levels, high levels of irritating disinfectant vapours)
all contribute to a worsening of kennel cough signs because they irritate and abrade the airways of animals, leading to airway lining damage - this results in inflammation and irritation of the airways, thereby worsening the signs of kennel cough. The damaged areas also provide a nice place for secondary bacteria to invade and grow and produce bigger infections. Additionally, some airborne chemical irritants
even reduce the motility of the respiratory cilia (small 'hairs' in the respiratory tract that are designed to remove infectious contaminants from the lungs), thereby
making it much easier for bacterial and viral infections to become established.
Stressful conditions:
Conditions of extreme or frequently fluctuating heat and humidity, as well as dusty conditions; overcrowded conditions; unsanitary conditions; draughty conditions; transportation; exercise fatigue; weaning; pregnancy; lactation; the presence of other diseases (e.g. parasites and other illnesses) and conditions of inadequate or ever-changing nutrition all contribute
to kennel cough manifestation and spread. This is because all of these conditions result in high levels of animal stress: stressed animals (even vaccinated animals) have poorer immune systems and, as a result of this, are more likely to show signs of infection
and more likely to shed infectious particles into their immediate environment.
3c) Real-life situations that promote dog to dog transmission of kennel cough:
1) Boarding kennels:
Kennels often house large numbers of dogs in close proximity; these animals are often stressed (which lowers
their immunity to disease) and the facilities are often designed to be of a more enclosed/indoors
structure, rather than an outdoors/open-planned structure (consequently, there may be
little breeze to blow the infectious aerosols and dust away). 2) Pounds and shelters:
This is probably the worst situation for kennel cough transmission. Animals are often
kept in overcrowded conditions, in close proximity to each other; conditions are often
dusty (dust traps infectious particles and can be breathed in); animals are often very stressed and of poor nutritional status (this lowers their immunity to disease) and their vaccination history is generally very poor (thus there are more animals shedding
the infection and more animals that are susceptible to it).
3) Dog clubs and dog shows:
On the plus-side, animals that attend dog shows and dogs club events are generally well-vaccinated; their owners generally don't take them to these events if they are sick and these events are often held in spacious settings (often outdoors). All of these factors act to reduce the risk of canine cough transmission. It is, however, still possible for dogs to contract canine cough in these settings because of the large numbers of dogs that attend
these events (dogs in close proximity can spread viruses easily); the stressed state of the animals (stressors include transportation, unknown dogs, unknown locations, exercise-induced fatigue etc.); the possibility of non-clinical disease shedders being present (some vaccinated animals infected with kennel cough can secrete virus particles but show almost no symptoms) and the possibility of dogs drinking from contaminated
communal water sources.
4) Breeding facilities:
Again, vaccination tends to be adequate among most breeding populations. Kennel cough, if it manages to get into a breeding colony, is likely to spread rapidly throughout the breeding facility, however, because of the number of animals located in close proximity to each other; the number of underage, highly-susceptible
animals around (newborn puppies etc.) and the high levels of stress that can occur
in bitches who are pregnant and lactating and in pups that are being weaned.
3d) Can a neighbourhood dog or a visiting dog give my dog kennel cough?
As vets, we are often asked by owners if their dog could have gotten a disease from a visiting dog or a dog that happened to 'sniff their dog through the fence.' In the
case of kennel cough, such disease transmission can certainly occur in this way, but is only really likely to occur if the visiting animal was overtly unwell (e.g. coughing in your dog's face); spent some period of time around your animal
(the longer the time spent with the infectious animal, the more chance of infectious disease transmission)
or drank from your dog's bowl (leaving infectious residues behind). It is unlikely
that your dog would catch kennel cough from the other dog if that dog appeared clinically
well (was not coughing and sneezing on your dog), if the contact was only brief (e.g. a brief sniff through a fence is unlikely to do it) and if your dog was in good physical and nutritional condition (under conditions of normal to low stress)
and adequately vaccinated.
3e) My dog hasn't been near another dog in months - how could he get kennel cough?
As mentioned before, there are other sources of kennel cough transmission, aside from
direct dog-to-dog contact. It is possible for a human (owner) to be contaminated by a dog with kennel cough and to spread the disease on to another animal via unwashed hands and clothes. Another possibility is that your dog was not
exposed to a dog with kennel cough recently, but ages ago, and developed a 'latent' virus infection at that time, which has, only now, decided to reactivate. Adenoviruses and herpesviruses
are two viruses that are known to 'go dormant' in the body for long periods of time. Following infection with these viruses, some of the organisms will go dormant and hide out in the animal's cells for months to years, producing no signs of infection. In situations of high stress (e.g. very anxious dogs, dogs that are unwell for another reason etc.), these viruses can reactivate, producing signs of kennel cough when no recent exposure to another dog has been noted by the owner. Similarly, the kennel cough bacteria: Bordetella
bronchiseptica, can survive in the airways of animals for long periods of time
without causing any symptoms. Similar to the latent virus situation, Bordetella can
reactivate in periods of high stress or immune suppression and go on to produce clinical
symptoms of kennel cough, regardless of recent exposure to a dog.
3f) Can vaccines cause kennel cough?
It is possible for some of the disease syndromes commonly attributed to wild-type, infectious
kennel cough organisms to occur when animals are given live kennel cough vaccines. Kennel cough vaccines, particularly the live intranasal parainfluenza 2, Bordetella and adenovirus
vaccines, can be associated with mild to moderate upper respiratory disease symptoms
(watery eye and nose discharges, sneezing, fever and coughing). The signs usually
develop within 2-5 days of receiving the vaccine. These symptoms are usually self limiting
(they usually abate in 4-7 days) and, in normal animals, they are generally neither severe nor life threatening. Most dogs do not require any specific treatment
for vaccine-induced kennel cough. Owners tend to get concerned about the signs because they are concerned about vaccine failure and believe that the vaccine has not worked.

4. What does kennel cough do to the dog? - an overview of kennel cough symptoms.
As mentioned in the opening sentences, kennel cough is a disease caused by certain viruses and bacteria that is characterized by fever and upper respiratory tract symptoms, such as coughing, sneezing
and watery eye and nose discharges, in dogs afflicted with it. The following
discussion is mostly for those of you who are interested in how the viruses and bacteria infect these organs and create the canine cough symptoms observed. Understanding how the infectious disease organisms work is useful because it aids your understanding of why the various symptoms occur; what complications can develop; how the disease is spread and what treatments are available.
4a) How the kennel cough viruses cause damage:
This discussion focuses on the major primary disease causing viruses that contribute
to kennel cough, namely: canine parainfluenza virus 2 and canine adenovirus 2.
There are other viruses that contribute to kennel cough (canine distemper virus (CDV), reovirus, canine adenovirus 1, canine herpesvirus), but these are of lesser significance and,
for ease of simplicity, can be thought of as having the same mechanisms of replication and
cell injury as canine parainfluenza 2 and canine adenovirus 2.
A parainfluenza virus (which is a subtype of paramyxovirus) is a tiny organism (much smaller than a bacteria) made up of a protein shell or capsule (termed a capsid) entwined around and protecting a strand of virus RNA (not DNA). The whole complex (the RNA sequence plus its protective capsid) plus additional free-floating proteins and enzymes is contained within a membrane coating (termed an envelope) that is made up of proteins, carbohydrates and lipids (fats). This envelope is very fragile, making the
parainfluenza virus organism highly susceptible to being killed/deactivated by heat, light, desiccation
and detergents or disinfectants.
An adenovirus, on the other hand, is a tiny organism (much smaller than a bacteria) made up
of a protein shell or capsule (called a capsid) entwined around and protecting a strand of DNA.
The organism is not enclosed in a protective membrane envelope, like the paramyxoviruses
(parainfluenza 2) are, and this lack of a weak, flimsy envelope imbues this organism
with great resistance to heat, light, desiccation and many disinfectants.
What is DNA and RNA?
You have probably heard of DNA (Deoxyribonucleic Acid). All human cells have DNA. DNA is a sequence of four different kinds molecules
(A,T,C,G) which can be arranged in millions of different combinations of varying lengths
to code for all of the genes of your body. The information contained in each gene
sequence can be used by the cell as a template or set of instructions by which that cell is able to manufacture certain important proteins and molecules vital to cellular function,
replication and survival. Every cell in the body has the same DNA (every cell therefore contains every gene in the body), but not every gene contained in the
full DNA sequence is switched on (activated) in every cell. Only certain cells use certain genes to guide them in making the proteins necessary for their structure and function.
For example: insulin is a protein coded for by a gene sequence contained in the DNA. The insulin
gene is only switched on in pancreatic cells and the cells of the pancreas use the information
contained in the sequence to enable them to make insulin for the body.
The DNA and RNA (RiboNucleic Acid) sequences contained within the adenoviruses (DNA) and parainfluenza
viruses (RNA) play a similar role in the functioning of the virus organisms to the role that DNA plays in our own cells. Similar to human DNA, viral DNA and RNA is basically just a strand of protein molecules arranged in various combinations (genes) that code for certain proteins and molecules vital to
virus function, replication and survival. The viral DNA or RNA contains sequences (genes) that
code for: enzymes needed in the replication of more strands of viral DNA or RNA; internal viral proteins (such as the virus capsid) and various other virus components, such as the surface proteins (the same ones we called antigens in our How Vaccines Work page) which allow the viruses to access animal cells.
Unlike bacteria and other, more advanced organisms, viruses do not contain all of the components needed to replicate by themselves. They require a host cell (e.g. a dog cell)
which contains all of the right components required for viral replication. For the sake
of this discussion, animal cells can be thought of as being comprised of three main
regions of viral importance:
1) The cell membrane - the coating (wall) of the cell which acts as a barrier to stop the nucleus and cytoplasm from leaking out and which plays a role in virus attachment and facilitation of virus infection (viruses must attach to the cell membrane first
in order to access a cell).
2) The nucleus - a region within the cell that is contained within its own thin membrane. It
contains the DNA that codes for all of the functions of the animal cell (see above DNA discussion).
3) The cytoplasm - the 'innards' of the cell that lie outside of the nucleus, but within the main cell membrane. The cytoplasm contains all of the 'equipment' needed to manufacture
proteins and molecules vital to cell function: it is the factory of the cell.


The images show a normal dog white blood cell: the important anatomy is of the cell is indicated (cell membrane, nucleus and cytoplasm).
When the parainfluenza virus or adenovirus enters the body of a dog, it attaches to the cell membrane of a particular body-cell-type that it has been specially 'designed' to invade. The virus has specific surface proteins, called attachment proteins, that allow it
to recognize, bind to and access certain cell types. For example, in canine cough, the cells that the virus prefers to invade are the cells of the upper respiratory tract and mucous membranes (conjunctiva of the eye and lining of the mouth and nose). When a kennel cough virus attaches to the right kind of cell, one of two things may happen:
1) the virus outer membrane fuses with the cell membrane (in the case of paramyxovirus), resulting in the virus capsid and RNA being released into the cytoplasm of the cell OR
2) the cell membrane reaches outwards, surrounding the adenovirus or parainfluenza 2 virus inside a 'bubble' of cell membrane (the process is termed endocytosis). This bubble gets released into the cell's cytoplasm where the virus fuses with it, resulting in the release of the viral RNA or DNA into the cytoplasm.
Either way, the genetic material of the virus (RNA or DNA) ends up within the cytoplasm of the host cell.
This viral RNA or DNA (depending on the virus type) travels to the nucleus of the cell. As mentioned above, the nucleus is the region of the cell that contains the cell's DNA - all of the gene sequences that code for the production of all of the proteins, sugars and fats that make the cell function normally (e.g. the proteins used in cellular chemical reactions, the proteins and fats used to make the cell membrane, the enzymes needed to get rid of unnecessary 'junk' that accumulates in the cell as a byproduct of its chemical reactions etc). The viral DNA or RNA enters the nucleus of the cell and makes use of the enzymes that the cell nucleus contains (and that the virus itself lacks), which enable the DNA of the cell to replicate prior to cell division. Using these borrowed enzymes, the virus replicates hundreds of copies of identical viral DNA or RNA sequences. It also uses the 'cell's machinery' (various cellular enzymes and cellular organelles contained in the cell cytoplasm) to get the cell to create hundreds of new capsids; viral proteins and virus surface attachment
proteins: all the components needed to make new viruses. The new DNA or RNA copies get packaged into the newly-created capsids, along with the other viral elements and surface proteins that the cell body has produced and, viola, hundreds of new viruses are made. In the case of canine adenovirus, the cell dies as a result of this infection and bursts, releasing all of the newly-formed viruses into the respiratory tract, where they can then go and infect other cells. In the case of the parainfluenza 2 virus, the RNA/capsid complexes (basically parainfluenza viruses without their enveloping
membranes) attach to the inside of the dog cell membrane and 'bud' out, taking a
surrounding coating of dog cell membrane with them. This cell membrane becomes the new
viral envelope of the parainfluenza virus and contains all of the viral surface proteins required to attach to and invade other dog cells (these surface proteins were
secreted onto the dog cell membrane surface during their creation, in preparation for
the moment of budding). The cell dies as a result of the destruction of its cell membrane by the many evacuating viruses.
This repeated process of virus invasion and cell destruction is what causes disease in the animal. In the case of kennel cough, because the virus needs to make use of the cells of the upper respiratory tract
(nasal passages, throat, pharynx, trachea, bronchi), this is where the cell damage occurs: consequently, most of the clinical signs seen relate to these organs. The more severe symptoms of disease are seen when the immune system fails to respond in enough time to kill the virus off in its early stages of infection, and large numbers of cells start dying as a result of viral replication.
4b) How the kennel cough primary and secondary bacteria cause damage:
Bacteria are microscopic organisms, large enough to see with a normal microscope
(unlike viruses which need a special electron microscope to see them). They are capable of replicating on their own, without making use of a cell, and they exert their
damaging effects on cells, not by way of intracellular reproduction (like viruses do),
but by the production of toxic byproducts that they release into their general environment. Large numbers of bacteria are capable of releasing large amounts of toxic byproducts:
these can cause great damage to the cells lining the respiratory tract.
Bordetella bronchiseptica is a respiratory bacterium with several interesting properties that make
it an exceptional invader and disease-causing organism within the respiratory tract.
Pathogenic (disease-causing) properties of Bordetella bronchiseptica:
1) Pili: Bordetella is equipped with finger-like appendages (termed pili), that help it to cling onto the surfaces of target cells. In this way, Bordetella is able to withstand the air currents present within the respiratory tract (even coughs and sneezes)
and not be blown away from its target cells.
2) Ciliary spasm toxin: Bordetella releases a toxin that stops the small 'hairs'
(termed cilia) lining the respiratory tract from moving. These hairs act to move
infectious particles and debris (mucus etc.) upwards along the trachea to the
throat, ready to be coughed out. By preventing them from working, Bordetella reduces
the ability of the lungs to clear out primary and secondary infectious disease organisms.
3) The ability to live inside cells: Bordetella is one of the bacterial species that can live happily inside cells (including white blood cells), easily evading the intracellular defenses that normally act to destroy invading, intracellular bacteria. Because of this property, Bordetella is able to evade the body's immune system (it is hiding inside a cell, away from the immune system's defenses) and able to avoid being killed by antibiotics that are unable to penetrate inside cells (see treatment section 7a - antibiotic properties needed for Bordetella destruction are
discussed here). As a result, if the incorrect type of antibiotic is administered or the
antibiotics are not given for long enough or at sufficient doses, the only effect will be to kill
the Bordetella organisms that are located outside of the cells. The intracellular Bordetella organisms will hide out inside the cells until the antibiotics have stopped and then they will come out again and start to replicate madly, creating disease signs once again. This is one of the ways in which animals might be seen to 'keep getting kennel cough': persistent Bordetella infection is one cause of chronic, recurrent airway tract infections that just keep coming back. It is also the mechanism by which some dogs maintain a persistent, low-grade Bordetella infection without any clinical signs (a carrier state): shedding infectious particles into the environment that can be caught by susceptible animals.
4) Chemicals that destroy cells: Bordetella releases chemicals that damage and
destroy the cells lining the respiratory tract. This creates inflammation of the airways
(and symptoms of infection - coughing, sneezing etc) and ulcerated places for secondary bacterial
pathogens to invade and replicate within. Note: Bordetella does not need to invade the cell to injure it.
5) Chemicals that reduce bone and cartilage regeneration: The bone and cartilage contained within
the nasal passages and trachea of an animal are breaking down and regenerating all the time as
part of their normal cell and tissue turnover processes. Old tissues are replaced by new ones.
Normally the bone and cartilage breakdown rate = the bone and cartilage regeneration rate. Bordetella bronchiseptica is capable of suppressing this bone and cartilage
regeneration rate such that the overall result is an eroding and softening of the bone and
cartilage of the trachea and nasal passages. Over time, this eroding and softening can lead to loss
of cartilage and bone in the upper respiratory tract and warping of structures such as the trachea and bronchi (if they lose their rigid structure, they can start to collapse
as the animal breathes in and out, resulting in airway obstructive signs). In piglets, Bordetella
causes a condition called turbinate atrophy where the cartilage and bone in the nose is completely eaten away.
6) The ability to live in oxygen: Some bacteria are incapable of surviving in conditions of
high oxygenation. Obviously, these bacteria would make very poor respiratory tract pathogens. Bordetella, on the other hand, likes to grow in conditions of high oxygenation and thus it is perfectly
suited to inhabit the respiratory tract.
7) Endotoxins: see pathogenic properties of secondary bacteria below (point 9).
In addition to Bordetella bronchiseptica, there are many other bacterial types that are able
to create damage within the upper respiratory tract: e.g. Pasteurella, Streptococcus,
Staphylococcus, Klebsiella, Pseudomonas, E. coli and Rhodococcus. These bacteria may be 'contracted' from other animals, but, more commonly, they are already a normal part of the bacterial flora that
inhabits the animal's respiratory tract at all times. You can often culture these bacterial
types from the airways of normal animals. Normally, these bacteria do not cause any signs of disease
because the normal debris-removal mechanisms (cilia motion etc) and respiratory
tract immune system defenses keep them in check. The time that they do become a problem is
when the upper respiratory tract is damaged by a primary disease causing organism
such as a respiratory virus or Bordetella infection. These bacterial organisms take advantage
of the damage inflicted by these primary kennel cough organisms (erosion of the airway linings, spasming and immobility of the cilia, suppression of the local immune system etc.)
and replicate to large numbers, whereby they are able to inflict further damage to
the upper respiratory tract. Because they generally do not cause disease in normal
tissues and mostly take advantage of already-injured tissues, these bacterial types are termed secondary
disease causing organisms. It is mostly to reduce this secondary bacterial infection that
antibiotics are given to animals with kennel cough (see treatment section 7a).
Pathogenic (disease-causing) properties of secondary bacteria:
1) Ciliary spasm toxin: Other bacteria are able to release toxins that stop the small 'hairs' (termed cilia) lining the respiratory tract from moving. This reduces
the ability of the lungs to clear out primary and secondary infectious disease organisms.
2) Pili and slime: Bordetella is equipped with fingerlike appendages (termed pili), that help it to cling onto the surfaces of target cells. There are other bacteria (e.g. Pseudomonas and E. coli) that also share this method of cellular attachment. In the case of many Staphylococcus species, the attachment
mechanism is not via small fingers, but, instead, via a sticky, slimy coating that glues the bacteria
to the target cells. In this way, these organisms are able to withstand the air currents present within the respiratory tract (even coughs and sneezes)
and not be blown away from their target cells.
3) Chemicals that destroy cells: Many bacteria including E. coli, Pseudomonas, Pasteurella, Staph aureus
(golden Staph) and various Streptococcus species release chemical enzymes that damage and destroy the cells lining the respiratory tract. For example: proteinases released by
bacteria break down host cell proteins (most of a cell is protein); lipoproteinases break down lipoproteins (lipoproteins are fat-protein complexes that make up most of a cell's outer membrane) and esterases and lipases break down various fats. These chemicals create vast regions of cell destruction, open ulcers and tissue inflammation and more places (e.g. ulcers and regions where the defensive cilia have been stripped away) for secondary bacterial pathogens to invade. Pseudomonas aeruginosa in particular, is noteworthy:
this bacteria produces many cell-destroying toxins and causes severe necrosis (rotting)
and ulceration of the respiratory tract tissues.
4) Chemicals that call-in inflammatory cells: Many bacteria (particularly the pus-making bacteria such as Streptococcus, Staphylococcus) release chemicals that
act as powerful messages, calling white blood cells into an area of infection (this
is all pus is - bacteria and white blood cells mixed together). Although these white blood cells
are doing the right thing (coming in to kill bacterial invaders), their effects on the
lungs and respiratory tract can be very damaging. White blood cells kill bacteria
in many ways, one of which is by 'exploding' near the bacteria and releasing nasty chemicals
into the environment that break down the bugs. Unfortunately, these chemicals also
erode the cells and tissues of the respiratory tract, creating further damage and inflammation. In addition to this, too many white cells (too much 'pus') in the airways can block
the airways, resulting in an animal that is having trouble breathing past all the junk. This is
particularly the case if the ciliary clearance mechanisms of the lungs are not working (not helping
to clear the excess pus from the airways).
5) The ability to live inside cells: Bordetella is not the only bacteria capable
of surviving and hiding-out inside animal cells. Several species of Streptococcus and Rhodococcus also have this property. Similar to Bordetella, these organisms are able to evade
the body's immune system defenses and the many antibiotic types that are unable to penetrate inside of
cells. As with Bordetella, these intracellular bacteria are able to hide out within the body's cells until the antibiotics have stopped and then reemerge to create disease signs all over again. This is one of the ways in which animals are seen to 'keep getting kennel cough':
intracellular bacteria are able to create chronic, recurrent airway tract infections that just keep coming back.
6) Antiphagocytic capsules: Some bacteria, such as Pasteurella multocida, Pseudomonas, certain Staphylococcus species and numerous Gram negative bacterial types (named for their dye-staining properties), are coated with a slimy sugar capsule that protects them from being eaten by white blood cells (the process whereby white cells ingest and destroy bacteria is termed phagocytosis). Bacteria with this property are able to avoid immune system destruction for longer periods and, therefore,
have extra time in which to create more damage and replicate more copies.
7) Chemicals that kill immune cells: Some bacteria, including Pseudomonas, Streptococcus and Staphylococcus, are able to release toxins (e.g. hemolysins, leukocidans and NADases) that kill off white blood cells. Bacteria with this property are able to avoid immune system destruction for longer periods and, therefore,
have extra time in which to create more damage and replicate more copies.
8) Coagulases: Some bacteria, including Staphylococcus species, produce chemicals called
coagulases that facilitate the clotting of plasma proteins (which leak into inflamed
respiratory tissues from the blood stream) into a firm, white protein matte or mesh called fibrin. Fibrin is useful for bacterial survival because the bacteria can hide out in it, thereby avoiding the white blood cells of the immune system that are out to eat them. Fibrin protects the bacteria from the white blood cells because the white cells are too large
to get through the mesh of fibrin protein: it is as though the bacteria have protected themselves
inside a 'fence' of protein that the white cells can't access.
9) Endotoxins: Endotoxins are chemical toxins contained within the membranes of certain
bacteria (termed Gram negative bacteria because of their special staining properties)
including E.coli, Pseudomonas, Salmonella, Pasteurella and Bordetella, which are released into the local environment when those bacteria die. Endotoxins released into the bloodstream of an animal can result in many severe life-threatening side effects, including: septic shock, hypotension (low blood pressure), fever, reduced white blood cell numbers, critically low blood sugar levels, systemic inflammatory effects, deleterious effects
on the blood clotting system (animals are at risk of throwing blood clots (e.g. strokes or
pulmonary thromboembolism) or of having severe bleeding disorders) and even multiple organ
failure. It is for this reason that animals with severe Gram negative infections (e.g. Gram negative pneumonias) are so very sick. Staphylococcus aureus or 'golden staph' (a Gram positive bacteria) is able to produce a toxin that is not an endotoxin, but which has similar properties to one, among them, the ability to initiate symptoms of toxic shock.
10) The ability to invade tissues and organs: Some bacteria produce chemicals (e.g. hyaluronidases, proteinases,
lipoproteinases, lipases) that allow them to invade tissues deeply, even entering the bloodstream and setting up infections in other organs. This can result in microabscesses forming in other organs such as the eye, joints, kidneys, liver and brain.
11) Antibiotic resistance: Many bacteria have developed ways of avoiding contact with or succumbing to the lethal effects of many common antibiotics. The use of inappropriate antibiotics
can result in the bacteria gaining a head-start and causing severe respiratory infection. For example: some bacteria, notably the Streptococcus and Staphylococcus species, are able to produce chemical enzymes (termed B-lactamase or penicillinase) that destroy penicillin-based antibiotics. These antibiotics may have no effect against the organism. Pseudomonas is well-known for being resistant to large numbers of drugs and for being able to adapt and develop resistance following long term antibiotic therapy with the one drug. It can be a real battle to kill!
4c) Kennel cough symptoms - effects on the respiratory tract and mucous membranes.
The respiratory tract (nasal passages, throat, pharynx, trachea, bronchi and alveoli) of the dog is lined by a thin layer of cells termed an epithelium (i.e. the respiratory epithelium) or a mucosa. These cells have many important roles including:
1) secretion of mucus: Certain cells of the respiratory tract epithelium secrete a protective mucus
designed to capture any dust and infectious organisms (bacteria, viruses) that enter the nose and
trachea. This mucus capture prevents these irritating or infection-bearing particles from reaching the small air passages deep inside the lungs (the vital thin-walled regions where oxygen enters the bloodstream) where they could do most damage. These mucus-producing
cells are the reason why your nose 'runs' when you have a cold or an allergy.
2) forming a cell barrier: The epithelial cells form a physical barrier preventing bacteria and
viruses within the respiratory tract from entering the deeper lung tissues, bloodstream and other organs.
3) ciliary expulsion of contaminants: Many epithelial cells of the trachea and nose are topped with motile 'hairs' (termed cilia) that are designed to move mucus, cell debris and infectious contaminants out of the lungs and trachea and up to the mouth for coughing out or swallowing.
4) transfer of oxygen into the blood: The deepest regions of the lungs (termed alveoli) are
comprised of airsacs with walls so thin that oxygen is able to diffuse through them and into
the bloodstream. Similarly, carbon dioxide (a waste product of cell metabolism) is able to
leave the body through the same route: diffusing from the blood into the airways for exhalation.
The initial stages and symptoms of kennel cough infection: the primary infection.
When the cells of the respiratory epithelium become infected with a kennel cough virus
and/or a primary bacterium (e.g. Bordetella bronchiseptica), they become damaged and
start to degenerate. Ulceration of the lining of respiratory tract results, leading to severe irritation and inflammation of the affected regions (trachea, throat and lining of the nose). This irritation and inflammation causes the animal to cough and sneeze. Large volumes of watery, protein-filled inflammatory fluid and mucous (mucous is produced in large amounts by certain respiratory epithelial cells when they are irritated or damaged, as a last
ditch effort to remove the invading organisms) floods the respiratory tract. The animal
coughs up watery fluid (clear, white froth) and may find it difficult to breathe if the fluid and mucus is high in volume or if the infection and inflammation
involves the thin layers of cells within the deepest regions of the lung, where the oxygen gets
transferred into the blood. Severe irritation of the nasal passages results in
an initially watery, mucussy nasal discharge and sneezing. Affected animals may display signs of fever
(a hot mouth and nose, red gums, panting, drinking excessively, seeking out of cool areas to lie down) and
lethargy / sleepiness during these early stages of infection.
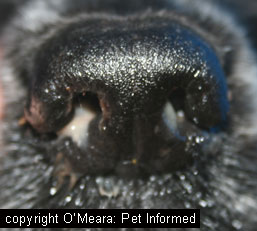
The effect on the mucous membranes of the nose, eyes and mouth:
The respiratory epithelium that lines the lungs is continuous with the mucous membranes
lining the eyes, nostrils and mouth (the cells on the surface of gums and the conjunctiva of
the eyes are mucous membranes too and are lined with similar epithelial cells). Kennel cough viral damage can extend to these regions, resulting in swelling, ulceration and inflammation of the gums, conjunctivae and nasal passages. The animal may develop irritation, redness and swelling of the eyes
(eye pain, squinting and a watery ocular (eye) discharges), nose (a watery nasal discharge and sneezing)
and mouth. Secondary bacterial infection of the nose and eyes can occur (see the next stage), resulting in a secondary, pussy bacterial conjunctivitis and rhinitis (inflammation of the nose).
The next stages and symptoms of infection: secondary infection.
 The damage and ulceration of the lining of the nose, trachea and bronchi results in paralysis and/or loss of the motile hairs (cilia) that normally clear bacteria from the airways. The loss of the
surface epithelial cells (which normally act as a physical barrier against infection) allows
the bacteria to attach to and gain a foothold in the exposed tissues underneath and the large volumes of inflammatory proteins and secretions within the damaged airways provides nutrition for the bacteria, allowing their populations to grow quickly. As
a result, secondary bacterial infection of the throat, trachea and nasal passages
can occur. This bacterial overgrowth results in massive numbers of white blood cells
flooding into the affected airways. The animal will often develop thickening of
the secretions within the trachea and nasal passages: these discharges may even develop a greenish or
yellowish discolouration (e.g. yellowish 'snot'). The presence of the white blood cells and bacteria within the airways can often worsen the clinical signs (e.g. the cough worsens as the bacteria and white blood cell toxins further erode the lining of the airways). Animals may find it difficult to breathe because of the thick pus plugging their airways (they will gag and hack and appear to choke
at times). These animals may be miserable and febrile (feverish) and will usually have a bad cough and sometimes a pussy nasal discharge. Sometimes these animals will be off their food and can appear very unwell. As a general rule, these animals will not usually have any increase in their respiratory rate (it should be 15-30 breaths per minute) because the disease is not yet affecting their lung function ... yet (see next section).
The damage and ulceration of the lining of the nose, trachea and bronchi results in paralysis and/or loss of the motile hairs (cilia) that normally clear bacteria from the airways. The loss of the
surface epithelial cells (which normally act as a physical barrier against infection) allows
the bacteria to attach to and gain a foothold in the exposed tissues underneath and the large volumes of inflammatory proteins and secretions within the damaged airways provides nutrition for the bacteria, allowing their populations to grow quickly. As
a result, secondary bacterial infection of the throat, trachea and nasal passages
can occur. This bacterial overgrowth results in massive numbers of white blood cells
flooding into the affected airways. The animal will often develop thickening of
the secretions within the trachea and nasal passages: these discharges may even develop a greenish or
yellowish discolouration (e.g. yellowish 'snot'). The presence of the white blood cells and bacteria within the airways can often worsen the clinical signs (e.g. the cough worsens as the bacteria and white blood cell toxins further erode the lining of the airways). Animals may find it difficult to breathe because of the thick pus plugging their airways (they will gag and hack and appear to choke
at times). These animals may be miserable and febrile (feverish) and will usually have a bad cough and sometimes a pussy nasal discharge. Sometimes these animals will be off their food and can appear very unwell. As a general rule, these animals will not usually have any increase in their respiratory rate (it should be 15-30 breaths per minute) because the disease is not yet affecting their lung function ... yet (see next section).
If the condition progresses ...
In severe cases of kennel cough, primary and secondary bacteria can reach the deep regions of the lungs, resulting in severe pneumonia (fluid and bacteria located within
and plugging-up the oxygen-transfer sections of the lungs) and an inability of the animal to get adequate oxygen into its bloodstream. Animals with severe pneumonia can even die from a lack of oxygenation, though this is rare with the kennel cough condition. These animals
will be very unwell, with increased respiratory rates, a soft, wet-sounding cough
and often fever and inappetence. Some will appear to have lost a lot of weight rapidly. Some of these animals will appear to breathe very rapidly and
heavily and will be reluctant to lie down and/or lie on their sides (some will simply stand
in one spot: not able to lay down nor walk around). Some animals may even have
a blue-tinged gum and tongue color (cyanosis). These are all signs of an animal with severe lung disease and respiratory compromise: these animals need urgent veterinary attention! Eventually, secondary bacteria and/or bacterial toxins may enter the bloodstream, resulting in severe illness, septic shock and the potential for multiple organ infection/damage and even organ failure. Death can be the result.
4d) Chronic recurrent kennel cough infections.
In the vast majority of cases, the antibiotics and other therapeutics prescribed by
the veterinarian will have their desired effect: the kennel cough infection will go away and the dog will be fine. In a small minority of patients, however, the kennel cough infection will seem to keep coming back again. The animals will seem to respond to the antibiotics prescribed (although, sometimes they may not even respond to these), the cough will seem to settle down and then, within weeks to months of the antibiotics coming off, the symptoms will return again (especially the characteristic harsh, dry cough).
So what is happening here?
Well, there are many reasons why the symptoms of kennel cough may keep on returning
within the one animal. These are as follows:
1) The disease is not kennel cough:
Face it. If you are treating a condition correctly and the animal is not responding
to the treatment given, it is time to re-evaluate the diagnosis. There are many conditions
that can mimic the symptoms of kennel cough, including other tracheal diseases (e.g. collapsing trachea, tracheal masses), tracheal and bronchiolar foreign bodies, cancer and allergic airway diseases (see section 6 - diseases that look like kennel cough). Some of these conditions can even be complicated
by secondary bacterial infections, such that they, like kennel cough, will seem to respond favorably (but transiently) to antibiotic therapies. Further work-up (see section 5), including
chest radiographs (x-rays), tracheoscopy, bronchoalveolar washes and cultures is required.
2) Some of the bacterial invaders are hiding-out intracellularly:
Some bacterial types (Bordetella, Streptococcus and Rhodococcus) are able to hide from
antibiotics inside of cells. They remain there safely, in hiding, until the antibiotics have stopped whereupon they then re-emerge as a renewed infection. If recurrent infection is thought to be the issue,
it is important for your vet to get a culture of the airways (culturing one of the known intracellular
bacterial types may be highly supportive of this diagnosis). It is also important
that your vet re-evaluates the antibiotic therapy that your pet is on: does the antibiotic
administered treat intracellular bugs, is the medication being administered long enough and at a sufficient dose?.
3) You are dealing with a resistant bug:
Some bacterial types (e.g. Pseudomonas) are very difficult to kill and highly resistant
to a wide variety of antibiotic types: they will keep coming back if the therapy is
insufficient. If resistant infection could be an issue, it is important for your
vet to perform a culture and sensitivity test on the animal's airways (see section 5c). The vet takes a sample of fluid from the trachea or bronchi of the animal and sends the sample to a lab, not only to determine the species of bacteria responsible for the recurrent infection, but also to determine the antibiotics that the bacteria is sensitive and resistant to. This test helps the vet to plan future antibiotic treatments. The antibiotic therapy that the pet is on should also be re-evaluated: is the antibiotic suitable, is the medicine being administered long enough and at a sufficient dosage?).
4) You are dealing with a latent virus that keeps re-activating:
It is possible for certain viruses (adenoviruses and herpesviruses etc.) to lie
dormant in the tissues of an animal for months to years, reappearing intermittently
to create signs of disease in that animal. Generally, the reappearance of latent viruses
is not a big factor in recurrent kennel cough infections (it is a huge issue with
recurrent herpesvirus cat-flu infections in felines). If it occurs, it generally occurs in animals that are undergoing a lot of stress (e.g. poor husbandry, conditions
of extreme heat and cold, poor or imbalanced nutrition, other illnesses, lactation, weaning or pregnancy, transportation, overcrowding, altered environment, owner absence etc.) or in animals
that have immunosuppressive diseases or are on immune suppressive medications. Prevention
of recurring latent virus infections involves determining the source of stress or immune suppression
and removing it (if possible).
5) The animal has some form of immune suppression and keeps getting infections:
Antibiotics can only really go a small way towards eradicating infection from an airway
or any other part of the body. When we give an animal antibiotics, we are hoping that
the antibiotics will kill as many of the bugs as possible, holding the infection at bay
so that the immune system (white blood cells, antibodies etc.) has time to respond and
finish the job (clearing all of the infection). If the animal's immune system fails to respond
(e.g. the animal is on immune suppressive drugs, chemotherapy or has an immunosuppressive
disease or congenital immune disorder) there is a high risk that antibiotics alone will be insufficient to clear all of
the infection. Consequently, as soon as the antibiotics are stopped, the infection will return
in a big way. Alternatively, because immune suppressed animals are at risk of catching infections in general, even if your antibiotics do do the job and wipe out all of the infectious
organisms this time, there is every chance that the animal will very soon get a whole new infection from the next virus or bacterial invader that comes along.
6) Environmental factors are still playing a role:
Kennel cough is a multifactorial disease with infectious, environmental and host elements
all playing a role in the severity and presentation of clinical symptoms. Some of the signs of kennel
cough (e.g. the harsh cough, nasal discharges) can be caused by some of the environmental
factors that contribute to the disease's severity: e.g. high dust levels, dry air conditions, airborne
irritants (ammonia levels, disinfectant fumes etc). If signs of respiratory disease
are seen to persist in an animal that has been treated appropriately for kennel cough, consider
the possibility that environmental factors could be keeping the signs of airway irritation going.
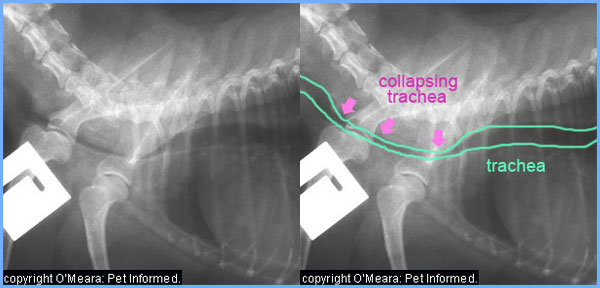
7) The canine cough disease has created secondary changes which are now the problem:
Severe kennel cough has the potential to cause long-lasting injury, scarring and weakness to
the upper respiratory tract: these secondary changes can result in chronic airway
irritation and clinical signs similar to kennel cough (coughing, risk of secondary infections), long after the original viral and bacterial kennel cough infections have gone. For example, bacterial infections such as Bordetellosis have the
ability to penetrate deeply into the cartilage of the airways, damaging and weakening
their structures. This can result in a weak, flimsy trachea and/or bronchi which are prone to
collapsing as the animal breathes in and out (see images below). Animals with this secondary airway disease
(collapsing trachea, dynamic airway disease) will have persistent airway problems and a long term chronic cough. Diagnosis of secondary mechanical airway issues can be made
on the basis of chest radiographs and endoscopy (a camera inserted down the trachea under
anaesthetic) - see section 5.
4e) Can animals show little or no signs of kennel cough and yet carry and transmit the infection?
The primary viruses and bacteria:
Whether or not the clinical signs of kennel cough appear in an individual animal
depends on several factors including: the immunity of the animal towards the disease (e.g. prior vaccination, prior exposure, a naturally strong immune system); the virulence of the virus or bacteria strain in question (how well the organism creates disease signs)
and the dose (number of organisms) of the virus or bacteria inhaled or ingested. These
and other factors all interact to determine if an animal will display disease signs or
not and, if so, how severe those disease signs will be. For example, low numbers (a low dose) of a very virulent, highly-aggressive organism be enough to create disease signs. Example 2: Low numbers of an infectious disease organism might be enough to create disease signs in an unvaccinated animal (animal with no pre-existing immunity), but not in a vaccinated animal.
Although I have mentioned before that vaccination is not 100% effective at preventing the clinical signs
of kennel cough from appearing (e.g. due to virus strain differences, dose of virus
inhaled etc. - see section 2a), it does, nonetheless, go a huge way towards reducing the severity of
clinical symptoms seen. Animals that have been previously vaccinated against kennel cough and which have good immunity towards the disease will often only get very mild disease symptoms or show no clinical signs at all when
exposed to a primary kennel cough virus or bacteria. All you might get is a low fever, a few days (around about a week) of occasional coughing and sneezing and perhaps some watery eye and nasal
discharges. The signs could be so subtle (a couple of coughs a day) that owners do not even know their pet has the disease.
Similarly, animals infected with a very low dose of kennel cough organisms or infected with very weak strains of kennel cough organisms may also permit these infectious agents to replicate briefly within their respiratory tracts (ready to pass on to other pets), but only show minimal signs of
infection themselves.
Author's note: dogs with low grade infections that are showing minimal or no clinical
signs of disease for reasons of pre-existing immunity, non-virulent virus/bacteria strains
and insufficient dosages of infectious agents probably make up the vast majority of animals that are infected
with kennel cough. Most animals of normal vaccine status that encounter kennel cough organisms
in their environment will show no signs or only develop mild signs of disease. They make up a much larger proportion of animals than those that go on to get the full-blown signs of kennel cough. The trouble is that we only recognize
those animals with the moderate to severe signs - we don't recognize the mildly affected
animals as readily and so their true prevalence goes unidentified.
It must be mentioned that dogs with these low grade, subtle signs of kennel cough can spread
enough viral and bacterial particles in their occasional coughs and sneezes and nasal discharges to infect other animals. Vaccination may go a big way towards stopping the animal
from showing severe clinical signs of disease, but it can not 100% stop the viruses and bacteria
from growing and replicating in and shedding from that dog's airways during the period of clinical infection and for variable periods of time after the clinical signs
have resolved. If another animal comes across these secreted viral and/or bacterial particles,
which has not been vaccinated against the disease or does not have an optimal immune system response,
this animal might well go on to develop severe signs of kennel cough, even though the dog that gave it the
disease was showing barely any signs at all.
This is the main way in which kennel cough still manages to be passed from dog to dog in high-vaccination-rate facilities such as dog clubs, breeding facilities and boarding kennels. In every vaccinated population, there will be a proportion of dogs that have acquired the canine cough infection and who are replicating and shedding the viruses/bacteria from their airways, but who are showing almost no signs at all. Because these animals (I'll term them 'mildly clinical') show minimal symptoms of infection (maybe
a subtle watery nasal discharge, an occasional cough etc.) the operators of the dog facilities do not recognise the infection and do not think to isolate these animals from the other dogs. Therefore, when new dogs enter the facility, whose vaccination status
is not optimum or whose levels of stress make their immune responses suboptimal, they
are likely to encounter the primary viruses and bacteria being shed by the mildly clinical
animals and consequently, they catch the disease.
Mildly clinical animals do not shed virus particles in their breath (i.e. an animal won't be affected
just by having another animal breathe on them). They tend to pass on their virus and
bacterial particles to other animals through shared food and water bowls (subtle, watery nasal
discharges contaminate the bowls), through face-to-face contact even through fences (face licking etc. where discharges could be consumed) and through coughing and sneezing
(aerosols carrying infectious particles get blasted into the air ready to be inhaled by
other animals). Unlike obviously infected dogs which cough and sneeze all the time and are readily identifiable, a mildly clinical dog might just cough or sneeze a couple of times a day (in a big facility, this might go completely unnoticed by the human carers). Even this infrequent
coughing and sneezing, however, is enough to disperse plenty of infectious disease particles throughout a facility (particularly a poorly ventilated, enclosed and/or overcrowded facility).
In addition to the mildly clinical animals (ones with active infection and only subtle signs), it is also possible for animals to become carriers of kennel cough. Carriers are animals that have recovered from kennel cough infection and who have no clinical signs at all, but who are carrying and replicating infectious organisms within their respiratory tracts. These
animals are impossible to identify just by looking at them, yet they pose a major
infectious disease risk to other susceptible animals because they are shedding infectious particles all the time. Carriers are a real issue in a large dog facility because
they are so hard to identify and remove from the main population - persistent carriers
make eradication of any infection almost impossible.
Thankfully, persistent, long term carrier states are not as prevalent with kennel
cough organisms as they are with certain other diseases. The kennel cough viruses
(parainfluenza and adenovirus) tend to only shed for up to 10 days after the animal
has recovered from kennel cough symptoms (i.e. the carrier state only lasts for about 10 days
after the clinical signs of infection have abated). Thus, continuing to isolate an infected animal for 10 days after the signs have resolved will overcome this carrier issue, if the kennel
cough disease seen is virus-related.
The main problem of kennel cough carrier states comes with the animals that have the Bordetella bronchiseptica form of kennel cough.
Bordetella is shed from the respiratory tract into the environment for an average of 3 months after the clinical signs have resolved (i.e. a carrier state of around 3 months can be expected) and some animals may carry and shed the infection for much longer. Some animals may even carry the bacteria indefinitely (after all,
many clinically normal animals have Bordetella in their respiratory tracts). Because it is not possible to tell which animals are going to carry and shed the
bacteria for over 3 months and which animals are going to shed it indefinitely, recommendations can not be given as to how long these
animals should be quarantined from the rest of the population for (3 months? - it's
a long time!) With Bordetella infection, one has to resign themselves to the fact
that long term carriers are possible and likely and that there will always be a
low grade shedding of Bordetella organisms into any kennel or cattery environment. The bacteria is unlikely to be 100% eradicated from any facility it gets into, despite prolonged isolation policies, good vaccination and disinfection protocols or any antibiotic remedies and, thus, vaccination is the best protection you can give in order to reduce the severity of disease
signs in susceptible animals.
The secondary viruses and bacteria:
In the case of secondary bacteria, such as Streptococcus, Rhodococcus, coliforms, Staphylococcus, Pasteurella and Pseudomonas, it is very common for animals to carry and shed these organisms and show absolutely no signs of infection at all. Carrier states are normal. In most healthy animals, these organisms are a natural part of the bacterial flora
that exists in the throat, nose and trachea all the time. The organisms have adapted to live
in these regions of the body and are kept in check and prevented from causing disease
by the animal's immune system and other physical barriers (e.g. the cilia of the trachea;
the respiratory epithelial cell barrier; the mucus secreted by the epithelium). The only time that these organisms become a problem, is when the respiratory tract's defenses get broken down as a result of damage by a primary disease-causing organism (e.g. such as kennel cough)
or some other pathological process (e.g. cancer, foreign body).
Secondary bacterial organisms do not usually cause any problem if they get passed on from one dog to another because both animals usually have the organisms present in their airways already.
The main times that transmission of secondary bacterial types (in saliva, respiratory secretions etc.)
can be a problem is if they are being passed on to non-typical hosts (who have not adapted to them
as the dog has); if they are being passed to hosts with poor immune systems (e.g. animals on chemotherapy, immune suppressive drugs, animals with immune suppressive diseases - HIV, FIV etc) or if they are being inoculated into areas of the body that are not as immune-competent or being inoculated in a manner which bypasses the normal defensive barriers. For example, the normal respiratory tract is able to cope with Pasteurella because of the immune system defenses and physical barriers that are in place
there. If that same organism gets inoculated deeply under the skin, through a bite or
scratch (bypassing the skin itself: a physical barrier to bacteria), the organism will not be able to be kept under control and an abscess may form.

5. Diagnosis of kennel cough.
Kennel cough is a common disease (probably the most commonly seen of the vaccinatable diseases
affecting dogs) that is generally diagnosed on the basis of the clinical signs seen in the animal and on the animal's history (has the animal been in contact with other dogs within the last
7-10 days?, are other dogs in the family showing the same signs?, is the animal
up to date with its vaccinations? ...). If the animal's clinical symptoms and recent history
are supportive of a diagnosis of kennel cough, then the vet will often treat the dog for this
disease without doing any specific diagnostic tests. It is a similar situation to what you, as a human patient, experience when you go to the doctor with a mild case of 'flu' or 'cold': the doctor will check you over, ask some questions about your recent history
and then prescribe some cold and flu medications. The only time that further diagnostic tests
are pursued is when the patient is very unwell (e.g. perhaps breathing rapidly or showing signs
of early pneumonia) or the clinical signs and history are not quite supportive of
a diagnosis of kennel cough. Diagnostic tests might also be pursued later on if the animal has not responded to the treatment given or keeps getting bouts of disease symptoms
(recurrent or chronic disease signs).
Author's note: dogs that have been fully vaccinated against kennel cough are
still capable of catching the infection. Up to date vaccination should not be used as
a reason why a dog might not have kennel cough, particularly if other aspects of the
pet's history are supportive (the dog has been to a pound or kennels recently, other dogs in the household are also coughing etc).
For the purpose of completeness, the rest of this section contains information and pictures pertaining to some of the diagnostic tests that your vet might run when presented with a coughing dog that
may or may not have kennel cough. Each segment includes information about the specific
test results that might be expected in a dog which does have kennel cough disease.
5a) Blood panels and urinalysis:
Running a full blood and urine panel is a useful way of getting information
about the overall bodily health of an animal, regardless of what disease it might have. It is one of the first tests that vets do when confronted with any sick animal. Basic
blood and urine tests run by veterinarians either 'in-house' (using machines available within the vet clinic) or 'at the lab' (sending blood off to a laboratory to be tested) can provide three kinds of information:
1) Biochemistry results,
2) A complete blood count and
3) A urinalysis.
Biochemistry panels are blood tests that measure the levels of calcium; pancreatic, muscle and
liver enzymes; metabolic waste products (urea, creatinine); electrolytes (blood salts);
proteins and fats (cholesterol, triglycerides) in the blood. These panels
can provide vets with general information about the health of the animal's kidneys, liver, pancreas, muscles and other organs and give clues as to the level of dehydration of an animal.
A very sick dog with kennel cough may not have been drinking for a day or so and a blood test
will indicate to the vet whether that dog needs to go on a 'drip' (intravenous fluids)
or not. A very old or very sick kennel cough patient (especially a dog with signs of pneumonia
or septic shock) may be at risk of liver and kidney damage (or organ failure) from the disease
and a biochemistry panel can tell the vet this too.
A full or complete blood count (FBC or CBC) is where the vet or pathologist takes a sample of the blood; performs a blood smear with it (a drop of blood is placed on a slide and 'smeared' out to a thin layer so that individual blood cells are easy to visualise); stains the smear in special stains/dyes and then examines it under a microscope. The size, shape, structure and coloration of the red blood cells
is assessed and noted. Also examined are the white blood cells (immune cells): the number and type of white blood cells is determined and presence of any 'toxic' features in the white blood cell populations
is identified and noted. The number and size of the blood platelets (small blood particles used
in blood clotting) is also examined.
A 'well' dog with kennel cough will often show white blood cell
changes typical of 'stress' (high cortisol levels in the blood): a high neutrophil and
macrophage count and a low lymphocyte and eosinophil count. These 'stress-related' changes
are not specific to kennel cough and occur in almost any sick dog. Dogs that have gone on to develop pneumonia or high levels of respiratory tract infection or blood infection may show a massive increase in their white blood cell populations (especially the neutrophils - see image 1). The
neutrophils may display what pathologists term 'toxic changes' (see images 4, 5): which means
that they have altered their cellular activity (and thus their appearance) in preparation for waging war against the bacteria. In severe infections, some of the white blood cells seen in the smear may be 'juvenile' white blood cells (termed bands - image 3):
immature white blood cells that the bone marrow has been forced to release out into the blood early (prior to complete maturation) in a desperate attempt to get more 'soldiers' into an area of infection. The presence of numerous immature white blood cells is a grave sign that infection is overwhelming the immune system's defenses. A low white blood cell count in the face of severe infection is an even graver sign, for it suggests that all of the white cells are being consumed in the infection: well in excess
of the white cell numbers that the bone marrow is physically capable of releasing into the system.
Other features of the blood cell sample including: the percentage of blood cells in the sample
(termed the PCV - packed cell volume); the levels of hemoglobin in the blood sample (Hb)
and the overall size of the red blood cells in the sample (termed the Mean corpuscular volume - MCV) are also included as part of the complete blood count. Special machines are needed to determine these values: they can not be done off a blood smear.
For example: a dog with kennel cough may present to a vet with a high PCV. This means that there are too many red blood cells (RBCs) in the sample and not enough blood fluid (termed plasma): i.e. it indicates
that the red blood cells are too concentrated. A high PCV can indicate that the dog is dehydrated and that it might need to go onto a drip. Dogs with chronic lung disease (not usually kennel cough, but certainly many other lung diseases) may have a persistently high PCV; not because of dehydration, but as a consequence of chronic hypoxia (long-term low blood oxygen levels). In these chronic cases, the bone marrow is being stimulated to make excessive numbers of red blood cells in a desperate attempt to move more oxygen around the body (the job of a red blood cell is to carry oxygen to the tissues).
A urinalysis is an assessment of the animal's urine, looking at the urine concentration (termed the USG
or urine specific gravity); the levels of glucose (sugar), protein, haeme (blood pigment), ketones and bilirubin in the urine and looking for the presence of cells, crystals, bacteria and fungi in the urine. The urinalysis is usually performed in conjunction with a full blood panel (biochemistry and complete blood count) and it gives the vet added information about the animal's kidney function and hydration status.
Complete blood count images:
Author's note: these are not kennel cough specific images. They are generalised images
of what vets might see running these tests.
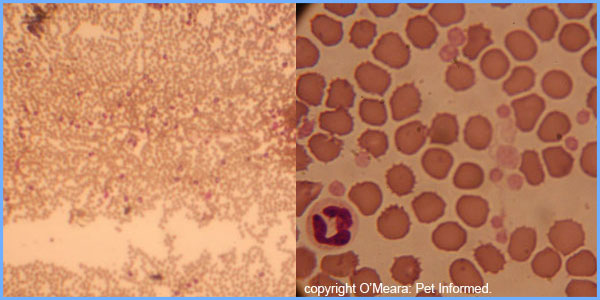
Image 1: This is a low-power microscope view (distant view) of a blood smear with a very high white blood cell count. See all of the darker purple dots throughout this image? These are
all white blood cells.
Image 2: This is a normal blood smear showing numerous red blood cells, a white blood cell (neutrophil) at the left edge of the image and many platelets. The platelets are the smallest, paler pink dots in the image.
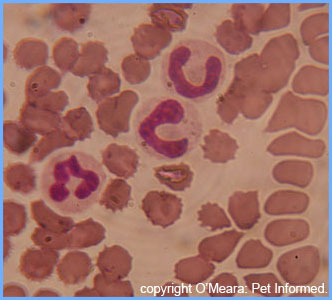
Image 3: The two cells with the horseshoe shaped nuclei are bands: immature neutrophils released into the blood in times of high infection.
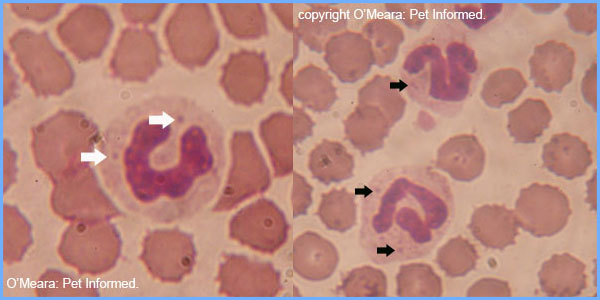
Image 4 and 5: These are both images of 'toxic' neutrophils: neutrophils preparing to attack nasty infectious invaders. Their cytoplasm color is darker, their nucleus is swollen and expanded-looking and they have Doehle bodies in their cytoplasm (the darker-staining dots indicated with arrows).
Urinalysis images:
Author's note: these are not kennel cough specific images. They are generalized images
of what vets might see running these tests.

Image 1: Testing the urine for pH, protein, glucose, ketone, haeme/blood and bilirubin
levels using a urine dipstick.
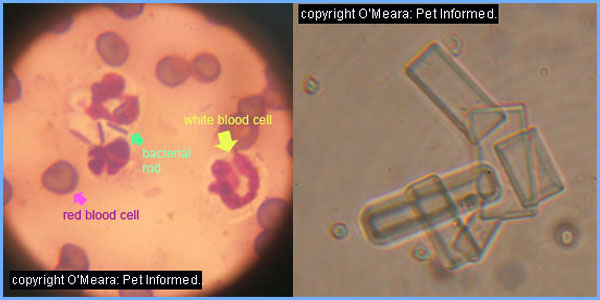
Image 2: This image is a microscopic view of a urine sample taken from a dog with a urinary tract infection. The cells in the image are white blood cells (neutrophils). One of the white cells contains
bacterial rods that it has ingested (phagocytosed) and is about to destroy. If a dog with
severe kennel cough developed pneumonia and bacterial dissemination throughout its body, bacteria traveling to and infecting the kidneys might appear in the urine as a secondary urinary tract infection.
Image 3: Struvite crystals in the urine of a cat. Struvite crystals can sometimes be
seen in dogs as a secondary complication of urinary tract infections and high urine pH.
5b) Chest radiographs (x-rays):
Chest radiographs (otherwise known as thoracic radiographs) are an excellent way of assessing the heart and lungs and major
airways of an animal with respiratory disease symptoms (rapid breathing, coughing, difficulty breathing etc.). Radiographs can give the veterinarian an indication of the size and shape of
the animal's heart (i.e. Is the animal coughing because of heart disease? Is the heart small
because of severe dehydration or shock?). Radiographs can give vets an indication of whether there is fluid within the lungs (e.g. pneumonia, heart failure); swelling around the bronchi and bronchiolar airways of the lungs (e.g. bronchitis, asthma, chronic inflammatory airway disease) or masses (tumours) within the lungs. Certain masses and foreign bodies trapped in the trachea or smaller airways may also be visible on chest films. Vets can assess the size of the blood vessels (arteries and veins) in the lungs, to see if there is evidence of congestive heart failure; heartworm disease; severe shock or dehydration or even pulmonary embolism. Xrays also show the vet the areas
outside of the lungs: the diaphragm, ribcage and chest cavity (e.g. Is the animal having trouble breathing
because there is fluid or cancer/masses between the lungs and the ribcage? Is the
animal having trouble breathing because it has fractured ribs or a fractured sternum? Does
the animal have a diaphragmatic hernia and abdominal organs in its chest cavity?).
The radiographs can also give the veterinarian information about the size, shape and outline
of the main airway - the trachea (e.g. Is the trachea collapsing? Is the trachea too narrow? Is it being
compressed by a tumour or a massive heart? Does the trachea have a tumour or a foreign body?).
In an uncomplicated case of kennel cough, it is unlikely that much
will be seen at all on the radiographs (see image 1). The heart size should appear normal, the lungs should
appear clear (nice and black on the radiographs), the airways and pulmonary blood vessels
should appear normal in size and shape and there should be no signs of chest wall (ribcage etc.) or
chest cavity (the space between the lungs and the ribcage) disease.
Author's note: obviously animals can have more than one disease. If an animal with pre-existing
heart disease or lung disease contracted kennel cough, you would expect the chest radiographs
to show signs/evidence of the pre-existing disease condition.
Animals with severe kennel cough disease and secondary complications (e.g. pneumonia, tracheal collapse) may
show supportive radiographic changes on their chest films. Pneumonia will appear
as dense patches of fluffy white opacity within the lung fields, often with the major airways (which may not yet be fluid-filled like the deepest parts of the lung are) clearly visible against that background of fluffy white. The appearance of clearly-visible, tree-like major airways on a background of white, opaque lung tissue is termed an air bronchogram.
It is characteristic of fluid in the lung tissues. See images 2-5, below.
Author's note: on a radiograph, fluffy white opacities in the lungs only tells you that there is fluid and/or cellular debris in the lungs. It does not prove that the
disease is pneumonia (lung infection and inflammation). Pulmonary bleeding, lung cancer and non-infectious fluid leakage into the lung tissues (a result of heart failure; low blood protein levels; severe systemic, whole-body inflammation and numerous other diseases) can all appear similar to pneumonia on a radiograph.
Author's note: the chest films seen in the images below are not kennel cough specific images. They are generalised images of the kinds of diseases vets might discover when radiographing the chest of any dog that is coughing or having trouble breathing.
Normal chest (thoracic) radiograph:
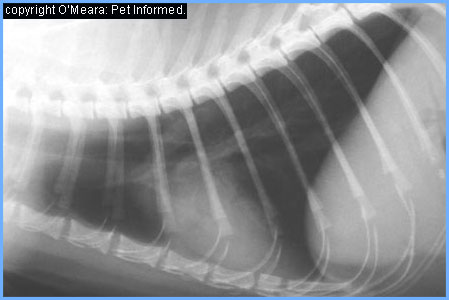
Image 1: The is a normal radiograph of an animal chest (in this case, a cat)
showing the heart (white region in the center) and lung fields
(the black regions) of the chest. Note how nice and dark and clearly defined the lung fields are
and how clearly defined the fine blood vessels in the lungs are. This nice, clear,
normal image is what would be expected in a dog with non-complicated kennel cough.
Lung disease - pneumonia:
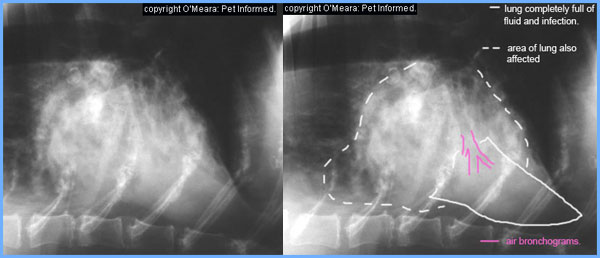
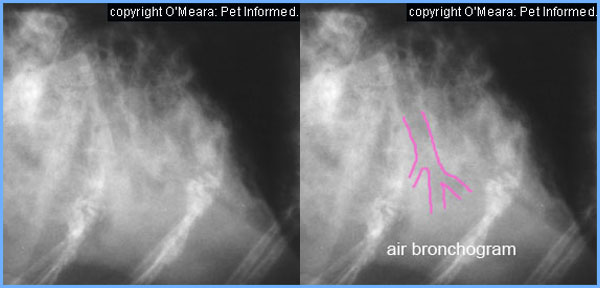
Image 2 and 3: This is an image of a dog's chest with aspiration pneumonia. See how
the lung is white and fluffy/cloudy-looking in the region indicated with the white dashes?
This is lung containing fluid and infection. One region of the lung (indicated with a solid white line)
is completely full of fluid and infection: there is no aerated spot left in it. A
tree-like air bronchogram (indicated in pink) is clearly visible here.
Image 4 and 5: Close up of the air bronchogram.
Lung disease - cancer:
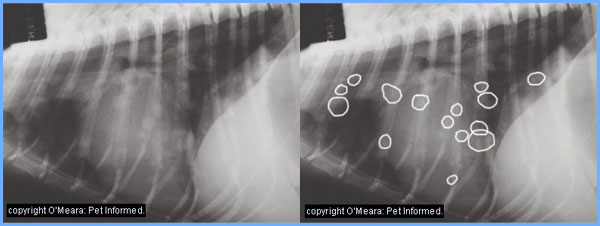
Image 6 and 7: This is the chest of dog with metastatic cancer. All of the white circles
in the lung fields (remember, the lungs should be black, not spotty) are tumors
that have spread from a cancer located somewhere else in the body.
Heart failure radiographic signs:
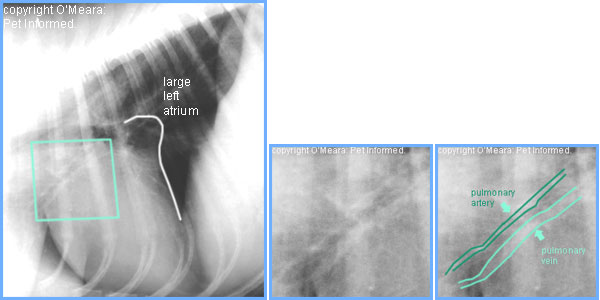
Image 8: This is a radiographic image of a heart with early signs of heart failure. The heart is enlarged, with a very straightened, upright rear margin and an obvious atrial wedge.
The atrial wedge is a radiographic sign that appears on the radiographed heart when
the left atrium (a chamber of the heart) gets very big due to heart failure. The region
indicated inside of the green box is the region contained in images 9 and 10.
Image 9 and 10: This is a close-up on one of the pulmonary arteries and veins (artery and vein supplying the lung)
of the heart failure chest indicated in image 8. See how the pulmonary vein is much larger
(wider) than the artery? This suggests that blood pressure is building up within the pulmonary veins because the heart isn't pumping very well. This dog is close to having fluid leaking into its airways and developing clinical signs of heart failure (coughing, trouble
breathing etc.) See image 11 - a dog in actual clinical heart failure.
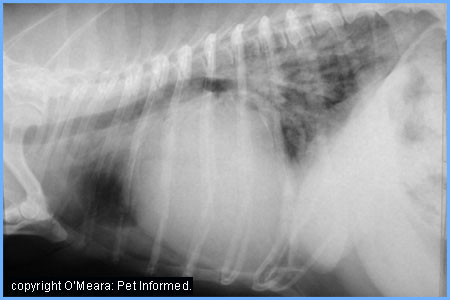
Image 11: This is a chest film of a dog with severe heart failure. The heart size is
enormous (compare it to the heart size in image 8) and the lung fields at the top
of the heart are fluffy and white in appearance. This white, fluffy opacity is fluid that has leaked into the air spaces of the lungs from the enlarged, over-pressured pulmonary
veins. This dog would be coughing and finding it very hard to breathe.
Chest cavity disease radiographic signs:
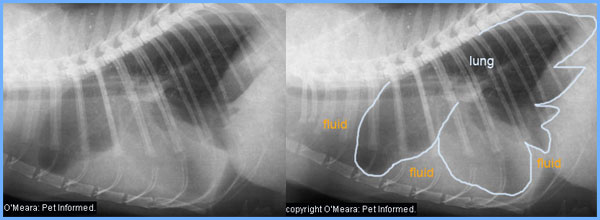
Image 12 and 13: This is an image of fluid trapped in the space between the lungs
and the chest wall. This dog would be having a lot of trouble breathing.
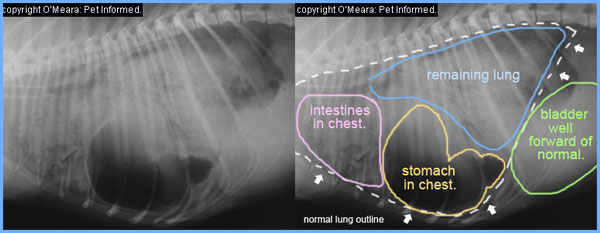
Image 14 and 15: This is a radiographic image of a dog with a diaphragmatic hernia. A prior road
accident resulted in this dog's abdominal contents herniating into its chest. You can imagine how difficult it was to breathe!
5c) Bronchoalveolar lavage: cytology and culture and sensitivity:
This test involves several different parts. Basically, a bronchoalveolar lavage (BAL)
is a procedure whereby an animal is placed under an anaesthetic; a long tube is threaded down its
trachea (main airway) into its smaller airways and small amounts of sterile saline are flushed in and out of the lungs in order to get a sample of the cells and fluid (and any bacteria or other infectious agents) contained in the lung. The fluid obtained from this procedure
is sent to a lab where two main tests are performed:
1) Cytology and
2) Culture and sensitivity.
Cytology is where the pathologist makes a smear of the fluid obtained during the
BAL procedure and examines it under a microscope in order to see what kinds of cells and
other items of interest are present. The types of cells present can provide clues as to the nature of the underlying disease. For example, if lots of degenerate (breaking down)
neutrophils (see image 1) and maybe some bacteria were seen in the sample, it might be suspected
that some kind of infection or pneumonia was part of the animal's problem. It may
not be the whole problem (remember, bacteria in the lungs can replicate as a secondary complication of a number of other diseases including lung cancer, foreign bodies and kennel cough viruses), but at least a contributor to the problem. If lots of eosinophils
were seen in the lung wash (see image 2), then an allergic or parasitic cause might be to blame. BALs can sometimes even yield some weird surprises including larval worms (e.g. lung worm infections
in cats) and cancer cells (some cancers shed cells into lavage fluid).
Culture and sensitivity is where the veterinarian places some of the BAL fluid sample
into a culture medium (a sort of nutritious 'broth' that the bacteria can grow in) and
sends this to the lab. At the lab, the bacteria are allowed to grow and tests are
done in order to determine the kind/s of bacteria responsible for the infection. The
kind of bacteria responsible gives the veterinarian vital clues as to how the bacterium
should behave and how it should best be treated. The sensitivity part of the test is where
the laboratory attempts to grow the bacteria in different kinds of antibiotic-containing
culture mediums in order to determine which antibiotics the bacterium is resistant to
and susceptible to. This also helps the vet to pick the right antibiotics to use.
It is possible for veterinarians to make a more definitive diagnosis of kennel cough, using
the BAL and culture technique, should the culture yield a strong growth of Bordetella
bronchiseptica. Bordetella is, after all, one of the primary kennel cough causing pathogens and, consequently, finding a good population of it would be very supportive of that diagnosis.
For your vet's advice: Bordetella is able to grow in oxygenated conditions and can be cultured
on blood agar or serum agar culture mediums. It is rapidly-growing and colonies should appear in
2-3 days. The one problem with trying to culture Bordetella is that it can often be outcompeted
by faster-growing organisms such as Pasteurella and Streptococcus (which are always present in the airways too) and not show up, resulting in a false negative result. Special culture mediums for
Bordetella (e.g. Bordet-Gengou agar) are available which may reduce the risk of Bordetella
being outcompeted and a false negative result occurring. Additionally, Bordetella culture
samples should be obtained from tracheal aspirates or BAL, not from swabs of the nose, mouth or throat.
The nose and throat are rife with secondary bugs and Bordetella tends to adhere to swabs
made of cotton or other fibers instead of going into the culture medium.
In the case of kennel cough, just culturing some of the secondary bacterial types from
a BAL and culture is not going to be definitive for a diagnosis of kennel cough. It is not uncommon
to culture Pasteurella and various Streptococci and Staphylococci from a wide range of diseases:
they are, after all, always in the respiratory tract. This does not, however, mean that
culture of suspected kennel cough animals is pointless. For one, the sample might culture
Bordetella. Secondly, if one of less-common, nastier secondary bacteria such as E. coli, Klebsiella or Pseudomonas was cultured from the respiratory tract of a dog with kennel cough, at least the vet would know to expect that this dog might become very ill and realise that these bacterial types need aggressive, longer-term treatment with a very specific range of antibiotics.
A final note: BAL, culture and cytology is not generally done when a dog first presents
to a vet with signs of kennel cough. Although you can culture Bordetella and might do this to
prove the diagnosis of kennel cough, most vets do not do this: they just treat for the disease. The main times that BAL and culture and cytology is done is when
the vet is suspicious of a disease other than canine cough; the kennel cough becomes complicated by pneumonia; the cough is not responding to empirical treatment (e.g. a resistant
bug is suspected) or the cough keeps on returning. Owners of large facilities (e.g. breeding kennels)
that are experiencing a major outbreak of upper respiratory infection may elect to do a culture
on several animals in order to clearly identify the organism at fault (know what they
are actually dealing with) and plan for better ways of controlling it (correct antibiotics, correct disinfectants to use etc.).
Cytology images:
Author's note: these are not kennel cough specific images. They are generalised images
of what veterinarians and pathologists might see running these tests.
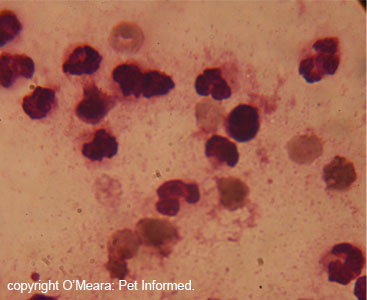
Image 1: degenerating neutrophils from a dog with a severe bacterial infection. See how broken-down
and indistinct the neutrophil nuclei are? They just look like purplish
'splats'. This is what is meant by degenerative.
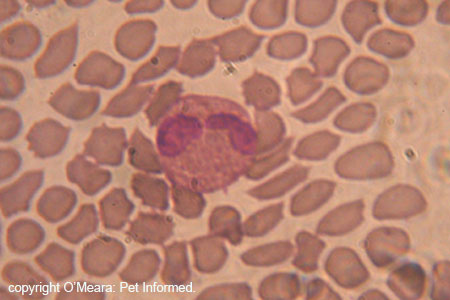
Image 2: This is an eosinophil in a blood smear. They are large white blood
cells with bright pink spots (called eosinophilic granules) in their cytoplasm.
A lot of these showing up in BAL fluid would be highly suggestive of an allergic
or parasitic (or maybe cancerous) respiratory disease.
5d) Endoscopy or tracheoscopy:
Basically, endoscopy or tracheoscopy is a procedure whereby an animal is placed under an anaesthetic and a long thin optical tube, with a video camera at the end, is threaded down its
trachea (main airway) in order for the vet to view the throat, trachea and the entrances to the smaller airways. Endoscopy is often coupled with the BAL procedure
(they are done at the same time) because the animal needs to have a general anesthetic
for both procedures.
Endoscopy is great for diagnosing problems such as tracheal tumors, tracheal foreign bodies
and mechanical airway issues such as collapsing trachea and dynamic airway disease (where the
airways are weak and collapse as the animal breathes in and out). It is not usually
of much help in diagnosing uncomplicated cases of kennel cough.
In a dog with an uncomplicated case of kennel cough, all the vet is likely to find
on endoscopy is a reddened throat and trachea; enlarged pharyngeal lymph nodes and
tonsils and possibly a mucussy to pussy slimy discharge over the surface of the nasal
passages, throat and trachea. This finding could fit with any number of irritant
upper airway diseases, not just kennel cough.
A final note: endoscopy is not generally done when a dog first presents to a vet
with signs of kennel cough. Most vets just treat for the disease. The main time that endoscopy is done is when the vet is suspicious of a disease other than canine cough; the kennel cough becomes complicated by pneumonia or a secondary issue such as collapsing
trachea; the cough is not responding to empirical treatment (e.g. a foreign body may be suspected of harbouring bacteria) or the cough keeps returning.
5e) Viral isolation:
It is possible to definitively diagnose canine parainfluenza virus and canine adenovirus 2, on swabs of
throat, tracheal and nasal tissues, using special virus isolation procedures available from certain laboratories. These viruses are, after all, primary kennel cough causing pathogens and finding evidence of them would be very supportive of that diagnosis.
Author's note: virus isolation is not generally done when a dog first presents
to a vet with signs of kennel cough. Although you can isolate parainfluenza virus and adenovirus 2
from swabs of the throat, nose and trachea, and might do this to
prove the diagnosis of kennel cough, the reality is that most vets do not do this: they just treat for the disease. The main times that virus isolation might come in handy is when
the vet is suspicious of a disease other than canine cough or the cough keeps returning
(the vet might be worried about a latent adenovirus that keeps reappearing). Owners of large facilities (e.g. breeding kennels) that are experiencing a major outbreak of upper respiratory symptoms may elect to do virus isolation
on several animals in order to clearly identify the organism at fault (know what they
are actually dealing with) and plan for better ways of controlling it (correct housing and isolation
procedures, stress-reduction plans, correct disinfectants to use etc.).

6) What other diseases look like kennel cough?
Kennel cough is characterized by irritation and inflammation of the nose, throat, trachea
and large airways, resulting in a harsh, dry, 'honking' cough that is exacerbated by
dry-air conditions, exercise and neck pressure (e.g. collar pressure); occasional sneezing
and sometimes a watery nasal and ocular discharge. Fever may or may not be present.
Sounds simple enough ...
Unfortunately for those of you who like to self-diagnose, there is a wide range of other conditions that dogs can get which may also present as a dry, harsh, hacking cough with or without signs of sneezing or nasal discharge. Basically, any condition
that causes irritation or inflammation of the throat, trachea and/or major bronchi
(the large airways branching off the trachea) will produce these clinical signs. The following
is a list (by all means not exhaustive) of conditions that can present similarly:
Collapsing trachea - a condition where the trachea collapses on inspiration or expiration.
Dynamic airway disease - a condition where the bronchi collapse on inspiration and/or expiration.
Tracheal or bronchial masses (e.g. tumours, cancers).
Tracheal or bronchial foreign bodies (e.g. inhaled grass seeds).
Tracheal or bronchial parasites - e.g. lungworms, Oslerus, Filaroides, migrating roundworm
and hookworm larvae.
Heartworm disease.
Early heart disease - during the early stages of heart failure, the heart can enlarge and
compress the left mainstem bronchus, producing a chronic, honking cough.
Allergic airway disease - chronic inflammation of the main airways due to pollen allergies, dust allergies etc.
Irritation of the airways from inhaled irritants - dusty conditions and the presence of
noxious vapors such as ammonia and disinfectants can irritate the throat and trachea
producing signs of coughing.

7) Treatment of kennel cough?
There is no specific treatment for the viruses that cause upper respiratory tract infections like kennel cough. Specific treatment (antibiotics) is available for
Bordetellosis (Bordetella infection). As a general rule, the treatment of canine infectious tracheobronchitis is pretty much a treatment of symptoms. The aim of therapy is to keep the animal comfortable
whilst it is fighting off the viral and bacterial infections and to manage and prevent any secondary complications (e.g. secondary bacterial infections, pneumonia). The hope is that, eventually, the animal's own immune responses will take over and destroy the viruses and bacteria, thereby bringing the condition to a conclusion. The treatment options for kennel cough,
their mechanisms of action and their pros and cons are discussed below.
7a) Antibiotics.
Antibiotics are pretty much the mainstay of kennel cough treatment. As mentioned in section 4, animals with kennel cough suffer a lot of damage and inflammation to the
lining of their respiratory tracts and are at risk of developing secondary infections
from bacteria present in the airways (this can lead to pneumonia and even infection of the blood and other organs). Antibiotics are given to these patients as a way of preventing this secondary infection
from occurring. They also act to kill off any Bordetella that might be forming a component of
the primary infection. Antibiotics do not kill viruses.
A lot of vets only prescribe antibiotics to their canine cough patients and nothing else: these animals often do perfectly fine. They might be more uncomfortable during their recuperation than those animals that receive additional anti-cough medications and anti-inflammatories, but they
generally recover nonetheless.
Commonly used antibiotics include:
1) Clavulanic acid / amoxycillin combinations (tradenames include Augmentin, Clavulox and Noroclav):
Most of the bacterial infections that complicate simple cases of kennel cough are
quite responsive to the antibiotic, amoxycillin. Amoxycillin is a B-lactam antibiotic, closely
related to penicillin. Because some of the strains of Streptococcus and Staphylococcus
are now resistant to amoxycillin (these bugs make penicillinase, an enzyme which destroys the drug), the antibiotic is generally combined with a secondary antibiotic called clavulanic acid, which helps to overcome this resistance (it inhibits penicillinase). Amoxycillin/clavulanic acid combinations are safe to use in dogs, including young puppies and pregnant and lactating bitches.
Dose rate: 15-20mg/kg orally, twice a day. It is generally administered for 10-14 days.
Clavulox is available as a syrup for easy administration.

2) Trimethoprim sulfonamide combinations (tradenames include Tribrissen, Trivetrin):
 Trimethoprim and sulfonamide are two individual antibiotic drugs that have been found to have
synergistic properties (enhanced bacterial killing properties) when they are used together. When used on their own, these drugs are bacteriostatic (they inhibit the
growth of bacteria, but don't kill them), but when used in combination, these drugs are
bacteriocidal (they kill the bacteria). As a result, most products containing trimethoprim or
sulfonamide include both drugs in the one capsule or tablet. The trimethoprim/sulfonamide combination drugs are highly effective at killing most of the bacterial types that commonly complicate kennel cough infections, including: Pasteurella, Streptococcus, Staphylococcus, E. coli, Klebsiella, Proteus and Bordetella. They have poor action against Pseudomonas. The trimethoprim-sulfa drugs are particularly useful because they are able to access many tissues (including the brain) that clavulanic acid/amoxycillin combinations can not reach.
Trimethoprim and sulfonamide are two individual antibiotic drugs that have been found to have
synergistic properties (enhanced bacterial killing properties) when they are used together. When used on their own, these drugs are bacteriostatic (they inhibit the
growth of bacteria, but don't kill them), but when used in combination, these drugs are
bacteriocidal (they kill the bacteria). As a result, most products containing trimethoprim or
sulfonamide include both drugs in the one capsule or tablet. The trimethoprim/sulfonamide combination drugs are highly effective at killing most of the bacterial types that commonly complicate kennel cough infections, including: Pasteurella, Streptococcus, Staphylococcus, E. coli, Klebsiella, Proteus and Bordetella. They have poor action against Pseudomonas. The trimethoprim-sulfa drugs are particularly useful because they are able to access many tissues (including the brain) that clavulanic acid/amoxycillin combinations can not reach.
Some cautions: trimethoprim/sulfonamide (TRMS) drugs should be avoided or used very cautiously in very young animals, very old animals, animals with kidney issues and in very dehydrated animals because they have the potential to cause renal problems (crystals of TRMS will deposit in the kidneys, leading to renal injury).
TRMS has the potential to cause dry-eye (keratoconjunctivitis sicca - KCS) in susceptible individuals
and caution should be exercised, particularly in KCS-prone breeds like cocker spaniels
and cavalier king Charles spaniels. Trimethoprim/sulfonamide combinations should be avoided
in certain breeds, especially the dobermann and weimeraner, because of the risk of drug
induced autoimmune joint disease and skin disease.
Dose rate: 15mg/kg orally, twice a day. It is generally administered for 10-14 days.
3) Doxycycline and other tetracycline drugs (tradenames include Vibravet):
The tetracycline drugs, particularly doxycycline, are particularly useful in canine and
feline respiratory tract infections. They are effective against a very wide range
of infectious disease organisms and their spectrum includes the commonly implicated
respiratory disease organisms, Bordetella and mycoplasma. As an extra bonus, these antibiotics are also able to get inside of cells in order to kill intracellular bacteria. They are quite safe for most dogs and cats of any age, but have the potential to cause browning of the developing permanent teeth, when given to animals under 4 months of age. For most owners,
this staining will not be of concern, but owners of show animals might want to be mindful
of the potential. Doxycycline can potentially be associated with stomach ulceration and tummy upsets (inappetence, vomiting and diarrhea can result) and so owners need to watch out for
these signs.
Dose rate: 5mg/kg orally, twice a day. It is generally administered for 10-14 days.
Vibravet is available as a paste for easy administration.
Important: Doxycycline tablets should be washed down with water (via a syringe) after giving so
that they go all the way to the stomach and do not sit in the esophagus. This is important
because doxycycline tablets and capsules have been known to cause severe oesophageal ulcers
and strictures if stuck here.
Tetracycline drugs should not be given with food that contains calcium (e.g. milk, bones)
or magnesium or other cations because these reduce its absorption from the gut.

4) Enrofloxacin, orbifloxacin and other fluoroquinolones (tradenames include Baytril and Orbax):
The fluoroquinolones are one of the newer antibiotic families to appear on the veterinary market.
These are great drugs with a good spectrum of action against many of the bacteria
that complicate kennel cough. They even kill mycoplasmas and Pseudomonas. They tend
to be more expensive than many of the aforementioned antibiotics (especially in large dogs)
and, because of their relative 'newness', many vets choose to use them as a last resort (reserved for severe infections only) in order to limit the evolution of bacteria
that are resistant to them. Some bacteria are only susceptible to fluoroquinolones now
and we are trying to reduce the development of antibiotic resistance to these drugs by not overusing them.
Fluoroquinolones are safe for most animals. They should not be used in dogs under 12
months of age (under 18 months old for large breeds) because of toxic effects on growing
bone cartilages. They should be avoided in cats of all ages, where possible, because of links with
sudden retinal atrophy and permanent blindness.
Dose rate: 5mg/kg orally, once a day. It is generally administered for 10-14 days.
Baytril is available as a syrup for easy dosage.

5) Other drugs:
Azithromycin (Zithromax) at 5-10mg/kg once daily for 5-7 days has been found to be effective.
Chloramphenicol has also been used in kennel cough patients - it has severe human health implications (aplastic anaemia) and should be only used as very last resort.
6) Alternative routes of administration:
In severe cases of kennel cough disease: animals with severe pneumonia, animals with
systemic (body-wide) bacterial infections and animals that do not seem to be responding
adequately to oral antibiotics; antibiotics can be given by alternative routes. Antibiotic solutions can be given intravenously to hospitalised animals that have been
placed onto intravenous fluid drips. Hospitalised animals with severe pneumonia may also respond
well to aerosolized (breathed-in) antibiotics, given using a nebuliser. Antibiotics
such as gentamicin and kanamycin (from the aminoglycoside family of antibiotics) can
be aerosolized using a nebuliser and breathed in by the animal, reaching the lungs
where their bacteria-killing effects are most required. These antibiotics are quite safe to give via this route because they are not absorbed into the rest of the body across the lungs.
7b) Antitussives - medications that suppress coughing.
Owners often get very concerned when their pet is coughing and coughing as a result of
kennel cough infection. The animal appears so very distressed when it coughs; it looks
uncomfortable and sometimes the coughing is so bad owners fear that their animal is
choking and can't catch its breath. Additionally, excessive coughing keeps the pet (and the owner) up at night. In order to ameliorate these symptoms, veterinarians often prescribe, in addition to the antibiotics, some form of cough suppressant medication.
Useful cough suppressants in pets:
Hydrocodone at 0.22mg/kg twice to three times daily. [ref 3 and 32]
Dextromethorphan-containing solutions (e.g. Linctol syrup) are also useful and given twice to three times daily.
Codeine-containing antitussives and butorphanol are also useful in pets, but their availability
is limited due to their potential for human misuse (they are drugs of addiction). It is also possible that products containing Dextromethorphan, Hydrocodone and dihydrocodeine
(Rikodeine) may soon become difficult to access due to recent misuse of these opiate-related products.
Airway dilators can also help reduce coughing by reducing the irritating spasming
and constriction of the inflamed airways. They are used a lot in asthma and allergic bronchial
conditions and may help with kennel cough. Useful drugs include:
Terbutaline (bricanyl).
Aminophylline and theophylline.
Where possible, the use of antitussives (cough suppressants) should be minimised
as much as possible. Coughing, annoying as it is, does perform a vital role in respiratory
disease resolution. Coughing acts to forcibly remove mucus, bacteria and cellular debris
from the airways, thereby helping to resolve airway blockage and infection. By preventing
this natural reflex, antitussives can potentially exacerbate and prolong respiratory
infections. These remedies are not recommended in animals with pneumonia (these animals need to
cough and clear their infections out!)

Image 1: Cough suppressant - dihydrocodeine.
Image 2: Cough suppressant - dextromethorphan.
Image 3: Bronchodilator - terbutaline (Bricanyl).
7c) Anti-inflammatory drugs - corticosteroids or non-steroidals.
Anti-inflammatory corticosteroid drugs (e.g. prednisolone, dexamethasone) or anti-inflammatory
non-steroidal drugs (e.g. meloxicam, carprofen, firocoxib) are often administered to kennel cough patients in an attempt to reduce the swelling and inflammation of the
throat and trachea and thereby ameliorate the clinical signs (coughing and fever).
Corticosteroids:
Prednisolone: 0.5mg/kg twice daily for three days, once daily for three days, then every second day for three days.
Dexamethasone: Often given as a one-off injection at consultation.
These drugs must be given with food.
Non-steroidal drugs:
Carprofen: 1-2mg/kg twice daily for 3-4 days.
Meloxicam: given as per label instructions.
Firocoxib: 5mg/kg once daily.
These drugs must be given with food.
A few safety tips: both families of drugs have the potential to cause severe side
effects including renal failure, liver injury and intestinal ulceration if used improperly.
They should be used very cautiously in very old and very young animals and should not be
used at all in severely dehydrated animals or in animals with preexisting renal disease, liver disease or severe intestinal ulceration. Additionally, the corticosteroid drugs are known to cause some degree of immune suppression
(they reduce white blood cell numbers and effectiveness), which means that they have
the potential to make infectious viral and bacterial conditions worse!
Because of the potential immune suppressant effects of the corticosteroid drugs, as a practicing
veterinarian, I tend to avoid the use of them in favour of the non-steroidals. If the
animal's symptoms are not too severe, I don't prescribe anti-inflammatory drugs at all.

7d) Nebulisers and shower therapy.
It has long been known that moistening the airways of an animal or human with pneumonia
or excessive mucus production in the trachea and throat can aid in treating the respiratory disease. Ever remember sitting at the kitchen table with a towel over your head,
breathing in boiled water and lemon fumes from a bowl, to try to resolve a flu? That's
nebulisation.
Nebulisation is a process whereby solutions of sterile water or saline (plus or
minus medicants such as antibiotics or airway dilators) are bubbled and/or heated through a machine
in order to produce an aerosolised vapor that can be breathed-in by a patient. The vapor
particles (aerosols) are so small that they are able to reach deep into the lungs. The aim of therapy is to moisten the airways and deeper sections of the lungs and, by doing so, moisten, soften and loosen the mucus secretions and pus secretions that are making
it so difficult for the animal to breathe and so difficult for the bacteria to be removed
(many bacteria hide out in the mucus away from the effects of antibiotics and immune cells
and can only be removed by being coughed up). This moistening, makes the debris easier
to cough up. Coupaging of the chest (a fancy way of saying firm, controlled beating on the chest) can help to loosen the moistened secretions and induce the animal to cough up the junk. (Don't try coupage at home without a vet to
show you first - you can do damage if you hit too hard or in the wrong spots). An added bonus of nebulisation is that it can be used deliver medications into the lungs
as well as moisture.
Most nebulising is done in a veterinary clinic. Animals with pneumonia, for example, are often kept in hospital and part of their therapy involves nebulising and coupaging
them every 4 hours.
Owners can also learn to nebulize their animal at home. Even 'well' dogs with kennel cough
(they don't have pneumonia, just a horrid cough) will build up mucus and debris
in their throats and tracheas, which you can help them to cough out through home-based
airway-moistening techniques. Home-nebulising can be done using a portable nebuliser machine
(a lot of people own them and they are easily accessible from pharmacies). These
machines are great because sterile saline can be put into them in order to create a sterile vapor.
Alternatively, a form of nebulisation can be done in the bathroom. Place the animal
in the bathroom (just on the tiles, not in the shower or bath itself) and turn the hot water tap on for 10 minutes or until there is a heavy mist in the room. This is aerosolised vapor - otherwise known as steam. Leave the dog in the room for 10-15 minutes (don't let it access the hot water or
it could get scalded) to breathe in the vapors. This will moisten the airways adequately enough to soften the mucus and debris in the throat and trachea and facilitate their clearance. It is not as sterile as the nebulising of sterile water or saline solutions, but it
is a useful technique in mild-moderate cases of kennel cough and other mucus-producing
and snot-producing diseases such as cat-flu and bronchitis.
7e) Isolation.
Kennel cough is a contagious disease that is highly transmittable to other vaccinated
and non-vaccinated dogs. Dogs with the disease should be kept in isolation at home
(away from other dogs in the family) and not exposed to dogs in public areas
(including the park, the street, dog clubs etc.).
How long should I keep my pet in isolation?
Dogs should be kept in isolation whilst they are displaying any signs of kennel cough and, once the clinical symptoms have abated, they should remain in isolation for a further
10-14 days. The reason for this prolonged isolation is because the kennel cough viruses may continue to be shed into the environment for at least a further 9 days, post-infection.
Bordetella has the potential to persist in and shed from the respiratory tract for an average of 3 months after clinical signs have abated (sometimes much longer). If Bordetella has been isolated
from a diagnostic tracheal wash (BAL) and culture, you might have to consider isolating your dog for that long (3 months post infection) - though this is not always practical or realistic. Owners of dog facilities and breeding facilities who are dealing with a kennel cough epidemic
or outbreak may have to seriously consider these 'long-term Bordetella shedders'
and isolate them for much longer, if they are to rid themselves of the infection.
7f) Rest.
Don't underestimate the value of rest. Animals with kennel cough should be allowed
to bed down in a quiet, warm, stress-free place whilst their infection resolves. These animals
feel crummy and feverish: they don't want to walk around the block any more than
you do when you have a cold. These animals have mucus and pus in their throats and
noses and can often find it hard enough to breath while laying down, let alone running around a park! Additionally, exercise places stress on the body, which
lowers the immune system, and exercised dogs pant, an action that forces dry air
across the airways and can exacerbate the tracheal and throat irritation and the clinical signs. Animals should be rested and not exercised for 2 weeks following
diagnosis of the condition.
7g) Environmental management.
As mentioned in section 1 and section 3, kennel cough is a multifactorial disease with
environmental as well as infectious components that can exacerbate the disease's severity
and clinical presentation. You can help your animal recover from kennel cough by removing
some of the environmental factors that could be exacerbating your friend's respiratory
signs. These include:
Reduce dust levels: dust irritates the airways and worsens symptoms. Reducing the dust levels in your pet's environment (through better cleaning, air purifiers and better ventilation
and air circulation systems) or removing your pet from a dusty environment can help.
Reduce irritant levels: disinfectant vapors and high ammonia levels in an area can
worsen respiratory symptoms. Reducing the levels of irritants in your pet's environment (through better sanitation, better rinsing after disinfection, air purifiers or better ventilation and air circulation) or removing your pet from an affected environment can help.
Reduce stress levels: extremes of heat and cold, draughts, overcrowding, poor nutrition and
many other factors produce stress, which lowers the immune system and reduces the animal's ability to fight infection. Managing stress is an important factor in treating animals for kennel
cough and in removing or reducing kennel cough in large facilities (see sections 9 and
10 on kennel cough prevention). Making sure that animals are warm, dry and comfortable
is important. Animals need to be fed a balanced diet, enough to meet all their nutritional
needs (including extra needs such as lactation, weaning, growth or pregnancy, if the
animal has these requirements). Dogs should not be overcrowded or placed in situations
where they are being constantly threatened and intimidated by other dogs (e.g. boarding
kennels with mesh fencing - the animals have no privacy and get very stressed). Ventilation
and air quality should be optimal and animals should be kept in clean areas with
good sanitation (not lying in urine or droppings).
7h) Be aware of tight collars - remove them if you can.
Collars, choker chains and neck leads of any description put pressure on the trachea. In dogs with kennel cough, the trachea is very sensitive. One of the tests that vets do
in order to support a diagnosis of kennel cough is to press lightly on the trachea - if that simple pressure
makes the animal start coughing madly, then this is evidence of tracheal sensitivity
and supportive of a diagnosis of kennel cough. Likewise, collars and leads placed around a sensitive
trachea will also trigger the dog to cough severely, which is not very comfortable for the poor animal.
If your pet is resting inside your home and is at not risk of going missing, then
you can relieve some of the throat discomfort by removing or at least loosening
the animal's collar. Don't do this if there is any risk of the animal escaping
into the suburbs, because it will probably need its collar tags for proof of
identification and registration.
I said, in point 7f, that rest was important. If, for any reason, your kennel cough dog does
need to be walked (e.g. taken to the vet for a recheck), you can make this process
more comfortable for the animal by using a face-halter or a harness (goes around the chest)
instead of a collar and lead, which goes around the neck.
7i) Can you simply do nothing? Can you simply not treat for kennel cough?
A tricky question for a vet (we like to treat things). Because of the risk of animals with kennel cough contracting secondary bacterial infections, which can go on to cause pneumonia and
severe illness, I, personally, am an advocate of at least giving dogs with kennel cough some form
of antibiotic cover, if nothing else. Because antibiotics are prescription-only medicines, in order to get them you must see a veterinarian and have a consultation. If you can
afford it, then this is my number 1, optimum suggestion of what to do with a suspected
kennel cough dog: see a vet (make sure it is kennel cough) and get some antibiotics.
The reality is, however, that most dogs with mild-moderate cases of kennel cough
(particularly previously-vaccinated animals) will recover regardless of what you
or your vet does for them. Their immune systems and airway defenses are often perfectly capable of
taking on the infection, clearing it and then healing the damage without a single
drug or intervention from us. Think of yourself. How often do you 'ride out' a mild to moderate case of cold or flu without ever seeking help from a doctor? Plenty of
times, huh? It is the same thing for mild to moderate cases of kennel cough: most
animals will recover without seeing a vet.
Although I do prefer that you always see a vet if your dog is coughing (to be sure that your pet's condition is actually kennel
cough and not some other nasty disease), should you choose not to see a vet, there
are some things that you can still do at home to help. You can rest your pet (7f),
control any environmental and stress factors (7g), loosen your pet's collar (7h),
shower-nebulize your pet (7d) and isolate your pet from other animals (7e). If you do take the option
of not-treating, you need to watch your pet closely for any signs of deterioration
that might indicate a kennel cough complication is developing or that
the animal does not actually have kennel cough.
Things to be concerned about:
Your pet starts having trouble breathing.
Your pet's resting respiratory rate is over 30 breaths per minute.
Your pet's gum colour is very dark (brick red), very pale or bluish-tinged.
The cough is getting worse.
The animal is coughing up thick yellow or green mucus or blood.
The nasal discharge is yellow or green.
The animal goes off its food.
The dog starts showing signs unrelated to the respiratory tract (vomiting, diarrhea, neurological signs, bloating, skin disease).
There are some patients in which a wait-and-see approach is not recommended. I would
always get a very young animal (under 4 months old) or a very old animal (over 8 years) checked out immediately, if a cough developed. Very young animals can
succumb to secondary pneumonia very quickly, because their immune systems are not as advanced. Old animals also suffer a waning of their immune systems and they are also more likely to
get other diseases (heart failure, cancer) that can mimic kennel cough in appearance, but which can turn out to be much more severe. I would never advise a wait-and-see approach in any animal
with pre-existing lung or heart disease: a bout of kennel cough infection can be enough
to send these patients over the edge. I would, likewise, never advise waiting in animals
that have known chronic diseases or immune-suppressive diseases (e.g. immune mediated diseases, congenital immune system defects, cushing's disease, diabetes mellitus, cancers, renal failure, liver failure etc.)
or that are on immune suppressive medications (e.g. chemotherapy, corticosteroids). A bout of kennel cough infection could well send one of these animals over the edge:
their immune systems can not cope with secondary bacteria. I would, as a final note, also advise against using the wait-and-see approach on any dog, old or young, that has
not been previously vaccinated against kennel cough. You can expect that these animals
will suffer a much more severe infection than the vaccinated animals will, if left untreated.

8) What is the prognosis for kennel cough?
As a general rule, the prognosis for kennel cough is excellent. It is very rare to see an animal die from the disease, unless it becomes complicated by severe secondary issues such as pneumonia or septic shock or infection with a resistant bacteria (e.g. Pseudomonas)
or a nasty, systemic bacterial type (e.g. E. coli, Klebsiella, Pseudomonas).
The prognosis should always be considered somewhat more guarded in the following
patients (the reasons were discussed in section 7i):
very young animals (under 4 months old),
very old animals (over 8 years),
animals with pre-existing lung or heart disease,
animals with known chronic diseases or immune-suppressive diseases and
animals on immune suppressive medications.

9) How to prevent kennel cough.
This section focuses on the prevention of kennel cough in individual situations. It explains how pet owners (people with only a few animals) can prevent their pets
from contracting the infection. For information on kennel cough prevention and control
in large facilities (e.g. breeding facilities), see section 10.
The prevention of kennel cough in individual animals involves three key steps:
a) kennel cough immunization (vaccination);
b) avoiding contact with contaminated animals and environments and
c) enhancing the health, body condition and immunity of the animal.
9a) Vaccinating against kennel cough.
Canine parainfluenza 2 and Bordetella bronchiseptica are two of the five core vaccine
pathogens used in almost all puppy vaccines (the others being canine distemper, canine parvovirus and canine adenovirus type 1). Some intranasal vaccine products also contain protection against a third kennel cough causing agent: canine adenovirus Type 2.
There are three main types of vaccine products that can be administered to puppies for their first and subsequent kennel cough vaccinations: live intranasal vaccines, live injectable vaccines and killed (inactivated) injectable vaccines. These are discussed in detail
in the following paragraphs.
1: Intranasal kennel cough vaccines:
Intranasal vaccines are vaccines containing live, avirulent (low-disease-risk) kennel cough viruses and bacteria that are given up the nostrils of the dog. Intranasal
vaccines tend to be the kennel cough vaccination route of choice in many vet clinics because they are thought to provide superior protection against respiratory tract viral and bacterial infections when compared to the injectable vaccines.
Why are intranasal vaccines thought to be superior? Details about intranasal vaccine immunity:
Wild-type, disease-causing respiratory viruses and bacteria (e.g. kennel cough) gain access to the body via the respiratory route: the organisms are inhaled by a potential 'host' when another infected animal coughs them out. If the potential host animal has received an intranasal vaccine previously, the lining of its respiratory tract will be coated with protective
antibodies (made in response to the intranasal vaccine) and its regional, respiratory-system lymph nodes will contain hundreds of memory cells all primed to recognise the attachment proteins (antigens) contained on the surface of the invading respiratory organisms. As soon as the invading viruses and/or bacteria reach the respiratory tract, these antibodies and memory cells will activate and kill them off. In the case of intranasal vaccines, this immune system response is much quicker than that which occurs following an injectable vaccine because, with intranasal vaccination, the immune system defenses produced are
located in the same region as the invading pathogens. As a result, the invading agents don't get time to damage many cells and clinical signs of disease are greatly reduced.
On the flip side, because the intranasal vaccines have such a specific, localised effect
within the respiratory tract, they may not be as effective at increasing blood antibody levels
as the injectable vaccines are. Put simply: intranasal vaccines are best at inducing respiratory
tract immunity (as explained above) and are, therefore, better at inducing immune protection in the regions
where the organisms colonise, but the antibody levels in the blood (which protect the rest of the
body from infection) may not be as high with intranasal vaccines as they are after an injectable vaccine
is given. Consequently, kennel cough organisms that do manage to avoid the respiratory tract's immune system and which do manage to gain access to other regions of the body may not encounter as large an immune system attack (blood antibodies etc.) with the intranasal vaccines
as they would following an injectable vaccine. (See author's note at end of section 9a.)
The answer then?
Well, ideally, you want both: you want the respiratory tract's immune
system responses to be very high (to kill the organisms at the site where they invade)
and you want the blood antibody levels to be very high also (to kill any bugs that happen to
get through the respiratory tract's defenses and invade other regions of the body).
Studies on Bordetella (Greene CE) have shown that immune protection against kennel cough is strongest when puppies are immunised using both intranasal and injectable kennel cough vaccines. The immunity induced using this combination vaccination protocol is better than the immunity achieved when either intranasal
or injectable vaccines are used alone. In high-risk situations, puppies should receive
at least two injectable vaccinations against kennel cough in addition to a single intranasal
vaccination. Adult dogs receiving their yearly boosters can also be given both an
injectable and an intranasal kennel cough vaccination at the same time.
Opinion point - if the use of both vaccination routes at the same time was
not an option and I was forced to choose between one route of vaccine administration or the other, as a veterinarian I would most likely go with the intranasal vaccine route. The more focussed, respiratory-tract-localised immune response just seems to make a lot more sense
when protecting against respiratory tract invaders such as kennel cough. Also, the intranasal
vaccines do induce some level of blood antibody responses - the animal's body is
in no way left unprotected should the infectious agents manage to escape from the respiratory
tract into the bloodstream (see author's note at end of section 9a).
Other facts on intranasal vaccines:
Intranasal vaccines are available against Bordetella bronchiseptica, canine parainfluenza 2
and even canine adenovirus 2. Most intranasal vaccines only require a single dose
(given at 6 weeks or older) to be given in order to achieve their protective effects. Immunity may be achieved in as little as 72 hours, depending on the product used. Boosters are required
annually to maintain this protection.
Aside from their superior localised immunity, intranasal vaccines have other benefits. Some intranasal products can be used in dogs as young as 4 weeks of age and some can even be administered to pregnant bitches (see our vaccinating the pregnant dog page). Intranasal vaccine products are much less likely to cause allergic reactions than injectable vaccines are because the uptake of viral/bacterial antigens into the body is slower and, because
they are given intranasally, they are unable to cause vaccine site reactions (injection site lumps).
Because the viruses and bacteria in the intranasal vaccines do replicate within the respiratory tract
(this is how they exert their immune-system inducing effects), the animal will sometimes show mild signs of kennel cough (watery eyes, nose and mild cough) 2-5 days after vaccination,
and will shed vaccine viruses and bacteria into the environment. Although some owners find these
vaccine-induced symptoms annoying, they can be of benefit in multiple dog households and multiple
dog situations because the vaccine-infection aerosols produced can pass on to other dogs, potentially vaccinating them as well. The main issue with these side effects, particularly in large, multiple-dog facilities, is that these vaccine-induced symptoms
can closely mimic the real disease symptoms, thereby making it difficult for shelter personnel to distinguish
the infected animals from the post-vaccinated animals and know which ones to isolate.
Some intranasal kennel cough vaccine products:
Nobivac KC (Intervet) - Bordetella and parainfluenza 2. Able to be used in pregnant bitches
and pups over 4 weeks of age. Achieves its protective effect in 3 days, following a single dose. Yearly
boosters required.
Protech Bronchi-Shield III (Fort Dodge) - Bordetella, parainfluenza 2 and canine adenovirus 2. Able to be used pups over 8 weeks and achieves its protective effect following a single dose. Yearly
boosters required. Not for use in pregnant bitches.
Protech Bronchi-Shield I (Fort Dodge) - Bordetella only. Able to be used in pups over 3 weeks and achieves its protective effect following a single dose. Yearly
boosters required. Not for use in pregnant bitches.
A note of caution: the shedding risks of intranasal vaccines.
Dogs vaccinated with intranasal vaccines can potentially shed Bordetella organisms for up to 6 weeks following intranasal vaccination. Although this effect can be of benefit in
'vaccinating' other animals, dogs that are potentially shedding vaccine-associated
Bordetella should be kept away from pregnant bitches, young litters and immunocompromised
animals. These animals could become sick if exposed to the vaccine organism. If separation
from these highly-susceptible animals is not possible, the use of an injectable vaccine may be safer.
Additionally, vaccine-associated Bordetella can potentially cause disease in humans. Most of the time, human infection with Bordetella goes unnoticed, however, in a small population of people
(particularly immune-suppressed people, AIDS patients etc.) vaccine-induced Bordetella
can create severe illness. If exposure to immune suppressed people is suspected or likely, it might be safer to go with the injectable kennel cough vaccines discussed in the next section.
2: Live and killed (inactivated) injectable vaccines:
Because some dogs react so violently against having intranasal vaccines (most dogs
really don't like liquid being squirted up their noses) and because some owners (especially
breeders and show-types) find the side effects of intranasal vaccination (mild kennel cough signs) unacceptable, an alternative to intranasal vaccine administration is for the veterinarian
to use a live or killed injectable vaccine. Injectable vaccines are preferred when
high levels of blood antibodies are required (e.g. in large outbreaks) and they can even be
given in addition to intranasal vaccines to achieve a most ideal combination of both localised respiratory tract protection and whole-body antibody protection.
There are many brands of injectable kennel cough vaccines available. Most of the injectable parainfluenza 2
virus vaccines are live virus vaccines that come in combination with other vaccine viruses:
parvovirus, distemper virus and infectious hepatitis/adenovirus 1. These 4-in-1 combination vaccines
are termed C4 vaccines. Most of the Bordetella injectable vaccines are killed (inactivated) vaccines which usually have no other viruses or bacteria added. There is no canine adenovirus type 2 injectable
vaccine, however, some cross protection may occur with canine adenovirus type 1, which
is the vaccine virus given when we vaccinate against canine infectious hepatitis.
Unlike intranasal vaccines, injectable live and killed kennel cough vaccination schedules typically require two or even three doses be given to puppies in order to achieve protection, with yearly boosters administered thereafter.
Parainfluenza 2 injections:
Injectable vaccination against canine parainfluenza typically begins with a first needle that is administered at 6-8 weeks of age (the needle given is generally termed a C4 because it
protects against 4 different viruses, including parainfluenza 2).
Following the 6-8 week shot, your puppy will require follow-up vaccinations. The protocol
for these follow up boosters differs depending on the type and brand of C4 vaccine used by your vet and on the manufacturers' recommendations for use. In particular, whether or not
the vaccine is a conventional type of vaccine or a newer, potentiated vaccine will have a huge effect on the vaccine protocol applied. Your vet will have all of the relevant information on the vaccines s/he uses and will notify you of when the next vaccinations are due.
The original, conventional vaccines:
The original conventional vaccine brands put out by vaccine companies (and still commonly used today) typically advise that puppy vaccinations be given at 6-8 weeks, 12-14 weeks and 16-18 weeks (basically, three injections
approximately one month apart). The reason for the (comparatively) long course of puppy shots was the issue of maternal immunity and the fear that, if puppies were not vaccinated at 16-18 weeks, their maternal antibodies might
have 'killed off' the previous two vaccinations and thereby prevented the puppy from gaining its
own protective immunity. See vaccinating the pregnant bitch for details on maternal immunity.
The newer potentiated vaccines:
More recently, potentiated vaccines have been brought out that stimulate a greater immune response, overcome maternal immunity and allow for the vaccine course to be completed earlier (by 12 weeks), thereby allowing earlier puppy socialization. Vaccines of this type include Fort Dodge's Protech Duramune C4
vaccine range. The vaccine guidelines for these vaccines typically advise that a 6 week vaccine, 9 week vaccine and a 12 week vaccine be given or (if the first vaccination was a 9 week shot), a 9 week and a 12 week vaccine only.
The newer potentiated vaccine types also feature 'one-shot protection' in that full immunity
(12 months minimum) against parvo, distemper and adenovirus 1 can be attained with a single C4 vaccination, if that vaccine is given at or after 12 weeks.
Unlike parvo, distemper and adenovirus 1, the one-shot immunization protocol does not seem to confer adequate protection to animals against parainfluenza virus (even when given after 12 weeks of age) and so two doses, 1 month apart, are still recommended to protect against this virus.
Following the course of puppy vaccines, your dog will need to receive a kennel cough booster annually to remain fully protected. 3-yearly vaccines are not available for kennel cough organisms.
Some injectable parainfluenza vaccine types:
Canvac 4 (CSL limited) - live parvovirus, distemper, canine adenovirus 1 and canine parainfluenza 2.
Puppy vaccine schedules: three vaccines given at 6-8 weeks, 12-14 weeks and 16-18 weeks of age. Note that cover
against parainfluenza 2 will be provided after only 2 doses, but 3 doses are needed to cover
against the other three vaccine virus components. If the first vaccine is given at or after 12 weeks, then
a second vaccine at 16 weeks (or a month after the first) will provide full protection. Immunity to parainfluenza is achieved 10-14 days after the second dose. Yearly boosters required. Not for use in pregnant bitches.
Fort Dodge C4 (Fort Dodge) - live parvovirus, distemper, canine adenovirus 1 and canine parainfluenza 2.
Puppy vaccination schedules: three vaccines given at 6-8 weeks, 10-12 weeks and 14-16 weeks of age. Note that cover
against parainfluenza 2 will be provided after only 2 doses, but 3 doses are needed to cover
against the other vaccine virus components. If the first vaccine is given at or after 10 weeks, then
a second vaccine in 4 weeks time will provide full protection against parainfluenza. Yearly boosters required. Not for use in pregnant bitches.
Protech Duramune C4 (Fort Dodge) - live parvovirus, distemper, canine adenovirus 1 and canine parainfluenza 2.
Puppy vaccination schedules: three vaccines given at 6 weeks, 9 weeks and 12 weeks of age. Note that cover
against parainfluenza 2 will be provided after only 2 doses, but 3 doses are needed to cover
against the other vaccine virus components. If the first vaccine is given at or after 12 weeks, then
a second vaccine in 4 weeks time will provide full protection against parainfluenza. Yearly boosters required. Not for use in pregnant bitches.
Canigen DHA2PPi (Virbac) - live parvovirus, distemper, canine adenovirus 1 and canine parainfluenza 2.
Puppy vaccination schedules: three vaccines given at 8 weeks, 12 weeks and 16 weeks of age. Note that cover
against parainfluenza 2 will be provided after only 2 doses, but 3 doses are needed to cover
for the other vaccine virus components. If the first vaccine is given at or after 12 weeks, then
a second vaccine in 4 weeks time will provide full protection against parainfluenza. Yearly boosters required. Not for use in pregnant bitches.
Canigen KC (Virbac) - killed Bordetella and parainfluenza 2. Given as 2 doses, 1 month
apart, when the animal is over 6 weeks old. Yearly boosters required. Not for use in pregnant bitches.
Bordetella bronchiseptica killed injections:
Bordetella injectable vaccines tend to be killed vaccines available individually
or, in some products, in conjunction with parainfluenza virus. Unlike the
intranasal vaccines, they tend to require that two doses, given 1 month apart, be given
initially, followed by yearly boosters. Bordetella vaccines are often given
at the same time as the C4 vaccines are, with the initial vaccine being given
at 6 weeks or 12 weeks and the second shot being given a month later, in parallel
with the next dose of C4.
Injectable Bordetella vaccines are not innocuous. Because they are
killed bacteria-based vaccines (termed bacterins), they are often associated with an increased
risk of injection site reactions (swellings and lumps at the site of vaccination)
and an increased risk of severe allergic reactions (anaphylactic reactions) when compared to
live vaccines and intranasal vaccines. The risk of anaphylactic reaction is particularly
high when repeat vaccines are given: the first needle sensitises the immune system
against the vaccine and the subsequent needles result in the severe reaction. Some vets premedicate dogs with antihistamines 15-30 minutes prior to giving a second or third dose
of a Bordetella bacterin.
Some injectable Bordetella vaccine types:
Canigen KC (Virbac) - killed Bordetella and parainfluenza 2. Given as 2 doses, 1 month
apart, when the animal is over 6 weeks old. Yearly boosters required. Not for use in pregnant bitches.
Canvac BB (CSL limited) - killed Bordetella vaccine. Given as 2 doses, 1 month
apart, when the animal is over 6 weeks old. Generally given at 12 weeks and 16 weeks,
in conjunction with canvac C4. Yearly boosters are required. Can be used in pregnant bitches.
Immunity develops 10-14 days after the second dose.
Protech Duramune BB (Fort Dodge) - killed Bordetella vaccine. Given as 2 doses, 1 month
apart, when the animal is over 6 weeks old. Yearly boosters are required.
Immunity develops 10-14 days after the second dose.
A final note on yearly booster vaccines:
Some veterinary texts (e.g. Greene CE) state that, in the adult dog, intranasal vaccines may not go a long way towards boosting the animal's systemic antibody levels:
that they do not induce the high levels of blood antibodies that the injectable boosters do. This would suggest that kennel cough protection in adult dogs is superior when injectable
boosters are given and, from an antibody-level perspective, it probably is. My issue with this argument, however, is that, although the injectable vaccines
do induce higher levels of blood antibodies (great whole-body protection), the intranasal
vaccines do induce better localised immunity (antibodies in the air passages) where the
bugs actually land. Sure, these intranasal antibody responses might not provide the measurable systemic antibody level increases that the injectable vaccines do, but they are nonetheless present and, in particular, present where they are needed. The comparison seems to be one of measurement - intranasal vaccines provide a lot of protection, but just
because their effects are not as easily measured as the injectable vaccine responses are (you can measure blood antibody responses easier than respiratory immune responses), they are mispresented as being less protective in adult animals.
For best whole body and respiratory tract protection against kennel cough, my opinion is that both areas
(body and respiratory tract) need to be protected using the most effective means
possible for each region (intranasal vaccines for best respiratory protection and injectable vaccines for best blood antibody levels and whole-body protection). This protection can be optimised by giving adult dogs booster vaccines of both the intranasal and injectable forms of kennel cough
organisms at the same time. See author's note below for more clarity.
Author's note - I have simplified the effects of the intranasal and injectable vaccine routes
(e.g. by saying that intranasal vaccines create local respiratory tract immunity and injectable vaccines create systemic antibody immunity) for ease of understanding. In reality, there is some overlap
between the two routes of vaccination: intranasal vaccines do induce some levels of systemic, blood
antibodies and injectable vaccines do produce some immune system responses that end up localised within the respiratory tract. It is due to this overlap of effects that
a single route of kennel cough vaccination only (injectable or intranasal) is administered by most vets
at the time of puppy vaccination and yearly boosters and is the reason why, for the most part, single vaccine-routes (both injectable and intranasal vaccines) are highly effective at preventing or lessening the effects of kennel cough infection. So please, dear reader, don't go and scream at your vet because he only gave your dog an injectable vaccine or
an intranasal vaccine and not both. Most vets do this and most of the time the single
route (either route) is highly effective. The reason that I simplified the workings of the different
vaccine routes was to give you, the reader, a deeper understanding of what the different vaccine routes actually achieve (what they are best at) and to explain why there is greater
benefit when both routes are used at the same time, particularly in situations of high kennel cough risk.
For more information on the pros and cons of intranasal vaccines and live versus killed
vaccines, see our 'How Vaccines Work' page.
9b) Avoid contact with infected dogs and contaminated environments:
As mentioned in section 2a, kennel cough vaccinations, regardless of the vaccine type or vaccine schedule administered, are not 100% effective at preventing dogs from contracting the disease if the animal is exposed to the causative organisms. Consequently, a huge part
of kennel cough prevention involves keeping your pet out of situations where kennel
cough transmission is highly likely.
Because most cases of kennel cough occur when dogs are exposed to environments
that contain lots of dogs all co-existing in close proximity to each other, it stands to reason that kennel cough can often be prevented by not placing your dog in these situations. Boarding your
dog with friends or getting a house-sitter to look after your house and dog while you
go on holidays can be a low-disease-risk alternative to boarding your dog in a boarding kennel. Making sure that your fences and yard are dog-proof can reduce
the risk of your friend getting out and ending up in a pound or shelter where
kennel cough is rife.
Sometimes, of course, you do have to place your pet in environments where there are
many other dogs and thus the potential for respiratory (and other) disease spread. There are precautions that you can take, however, to reduce this risk. Some handy tips include:
1) Vaccinate your pet within 6 months of attending a show, dog event or boarding kennel:
Vaccine-induced immunity is strongest within the first 6 months of a vaccine and, therefore, vaccinating your dog a month or two before it meets other pets will reduce its risk
of contracting a vaccinatable infectious disease. In fact, in high risk situations, kennel cough vaccine producers even advise giving kennel cough booster vaccines, not yearly, but every 6 months!
2) Check out the boarding kennels for yourself before putting your in pet there:
Ensure that your pet's accommodation is suitable. Look for signs of poor husbandry and unsanitary conditions
that might promote disease spread. Does the place smell OK? Is the place well-cleaned
(look for excessive dustiness and dirt). Is the place well-ventilated or is it musty and enclosed with stale-smelling air? Are dogs placed in yards together (which could enhance disease spread)? Do they
share food and water bowls? Is the place overcrowded with animals? Are dogs placed
in situations where they may become stressed (e.g. dogs facing off against each other
through wire fences, extremes of heat and cold, inability to get dry, draughts etc.)
Look at the other pets in the place (if you are permitted to) - do you notice any coughing
or sneezing animals? If you see any major problems, don't board your pet there.
3) Only attend boarding kennels, groomers and dog clubs with strict vaccine requirements:
If they are being strict on you with your pet's vaccinations, you can be sure
that they are being strict on everyone else. This strictness keeps disease out of a place. Lax rules result in diseases.
4) Take your own food and water bowls to the boarding kennel or any dog shows or dog club events: This way your dog will not have to use another, possibly contaminated, bowl.
5) At shows and dog club events - keep your dog on the edge of the action, as far away from
other dogs as possible (preferably in a well-ventilated region):
This will reduce your pet's stress (it won't be close to other foreign animals) and will increase the
distances viruses need to blow to get to you.
6) Preferably attend dog club events that are outdoors, not in enclosed places:
This way the breeze will blow any cough and sneeze viruses away.
Be aware of the potential for you or other people or animals to bring disease home to your pet. If you have visited a place where there has been kennel cough infection (or any outbreak of infectious disease, for that matter), don't bring the disease back to your house on your hands or clothes, where your dog can catch it! Change your clothes, disinfect your shoes and shower thoroughly (this includes washing your hair)
before greeting your pet. Ideally, disinfection should take place somewhere other than
your own home. The same precautions should be taken when other people visit your home:
ask them if they have had any potential contact with infectious animals.
Although most cases of kennel cough infection are contracted in multiple-dog environments, kennel cough can potentially be contracted from individual dogs that visit your home.
Protect your pet by not letting people bring dogs around to your house. If they do, at least
request that their pet is fully vaccinated before it meets your dog. As mentioned in
section 3, it is possible (rare but possible) for dogs to pass kennel cough to your pet
if they cough or sneeze on your pet through a fence or gate. Make sure that your fences are somewhat enclosed: not just see-through wire that dogs can easily access each other through.
If you have had a case of kennel cough in your own home and/or yard, then you will need
to disinfect any contaminated areas and feed bowls in order to make them safe for any new puppies
that you bring home in the future (see section 11 below on kennel cough decontamination). Thankfully, most kennel cough organisms are fragile and very susceptible to many
kinds of physical and chemical disinfection techniques. It should be possible to remove it from your home with thorough cleaning.
9c) Enhancing the health, body condition and immunity of the animal.
A big part of infectious disease prevention, particularly kennel cough prevention, requires the activity of a healthy, fully-functioning immune system. Although vaccination is key to promoting the 'right type' of immune response, the overall health and wellbeing of the animal is critical if there is to be a strong immune system
response towards a disease. Disease prevention involves a holistic approach, with nutrition, exercise and mental health care all important parts of the process. Animals that are in good body condition and which have been given a balanced diet and are well-exercised and emotionally sound (e.g. not overly stressed or bored etc.) will generally be more resistant to disease and able to mount a better immune response.
Puppies that are malnourished and/or which harbour other bacterial and parasitic infections
in their lungs and intestines may be more prone to severe respiratory infections. Thus, good
nutrition and control of intestinal and lung parasites (worming etc.) are important in preventing and reducing kennel cough severity.
Some hints and tips:
- Puppies and dogs should be routinely wormed.
- Puppies and dogs should be fed a completely balanced (AAFCO approved) diet.
- Puppies should be played with and exercised within the home until fully vaccinated
(this human contact fulfills their exercise and mental health needs, but keeps them safe
from disease until fully vaccine protected).
- Dogs should be walked twice daily (once vaccinated) for a bare minimum of 15-30 minutes at a time
to aid both their mental health (reduces boredom) and exercise needs.
- Dogs should have toys and adequate room to move (e.g. yard size) to reduce boredom and stress
whilst you are at work.
- Dogs should not be overfed or allowed to become obese.
- Dogs should not be kept in dusty, irritant or poorly-ventilated air conditions.
- Dogs should be kept in low-stress dry, clean, sanitary environments with no extremes
of heat and cold, no draughts, good shelter and no build-up of urine or feces.
- Any known stressors should be identified and removed, if possible.
- Purchasing in-bred animals should be avoided - excessive in breeding may result in appearance of genetic immune disorders.

10. Controlling canine infectious tracheobronchitis in high-risk and/or already contaminated environments.
Kennel cough outbreaks are quite common in large multiple-dog facilities such as breeding facilities, shelters, pounds and even boarding kennels. They can occur despite good vaccination protocols
because of the multifactorial nature of the disease (environmental factors and
stress factors also play a huge role) and the different strains and types of infectious
agent that can be responsible. Consequently, large dog facilities need to have protocols
in place that will help them to prevent kennel cough and help them to deal with an outbreak of kennel cough
should it occur. Control and prevention of disease in these situations involves:
a) protecting the susceptible animals and preventing them from becoming infected,
b) reducing environmental virus and bacterial contamination and destroying the infectious particles and
c) reducing the non-infectious environmental and stress factors that can contribute to the disease.
10a: Protecting the susceptible animals.
In a situation of high kennel cough risk or pre-existing contamination of the environment
with infectious particles, any unvaccinated or under-vaccinated animals; any very young or very old animals; any unwell animals; any stressed animals (e.g. pregnant, weaning, growing or lactating animals) and any animals of high-risk, immunocompromised breed-lines are all going to potentially be susceptible to infection. The risk of these animals and any other dogs in the facility contracting kennel cough can be reduced
in the following ways (this is by all means not an exhaustive list):
1) Ensure that all animals within the facility and all
those entering the facility are up to date with their vaccines.
I probably don't need to say much more. Vaccines are not 100% effective, but they do
greatly reduce the numbers of clinically affected and severely affected animals. Animals
should, ideally, be vaccinated within 6 months of coming to the facility.
2) In high-risk situations, vaccinate all at-risk animals using intranasal vaccines.
Intranasal vaccines confer superior immunity when compared to the injectable kennel cough vaccines.
3) In high-risk situations, vaccinate all at-risk animals from 4 weeks of age.
There are some intranasal vaccines that can confer kennel cough protection in puppies
as young as 3-4 weeks of age. Starting vaccination early will protect the pups from
severe infection in high risk situations.
4) In high-risk situations, vaccinate all at-risk animals every 6 months.
Immune protection against kennel cough is strongest within the first 6 months of vaccination. After this, it tends to wane, increasing the susceptibility of the animals to the disease, until the time of the next vaccination. 6-monthly kennel cough vaccines can
keep immune protection higher for longer.
5) In high-risk situations, initial vaccines should include both intranasal and injectable vaccine types.
Immune protection against kennel cough is strongest when puppies are immunised using
both intranasal and injectable kennel cough vaccines (according to Greene CE, these studies
were done on Bordetella.) The immunity induced using a combination vaccine protocol is better than the immunity achieved when either intranasal
or injectable vaccines are used alone. In high-risk situations, puppies should receive
at least two injectable vaccinations against kennel cough and a single intranasal
vaccination. Adult dogs receiving their yearly boosters can also be given an intranasal
kennel cough vaccine and an injectable kennel cough vaccine at the same time.
6) Keep all females of breeding age up to date with their vaccines.
Ensure that pregnant bitches are up to date with their vaccines so that they
have some levels of maternal immunity (kennel cough antibodies) to pass onto their newborn puppies
through their colostrum. Vaccinating pregnant bitches to boost colostrum antibodies is an option for kennel cough because there are some Bordetella and parainfluenza 2 vaccines that have been registered for use in these animals.
7) Isolate pregnant bitches and litters from the rest of the dog population.
Pregnant and lactating bitches are under massive levels of physiological stress and are, therefore, highly susceptible
to respiratory infections regardless of their vaccination status. Likewise, newborn puppies
are also at risk of infection because their immune systems are not yet fully developed. Isolate bitches and their litters in easy-to-disinfect (e.g. tiled or concrete areas, not grass or soil) pens,
which have preferably never been contaminated with kennel cough, from the time of whelping to the time of weaning.
These pens should be located as far away as possible from the main dog population because
kennel cough can spread over long distances in aerosols produced from a single cough or sneeze.
Their air-conditioning, heating and/or air ventilation systems should not be continuous with
that of the main dog population because aerosolised organisms can travel through ducting. If whelping bitches and pups can be removed to a new non-contaminated premises altogether, while
decontamination of the kennel-cough-infected facilities is occurring, this would be even better. All bedding and feed and water bowls provided should be new (or well-disinfected) and should be strongly disinfected or discarded after use by the bitch.
8) Ensure that puppies get their colostrum on time (<24 hours after birth).
Puppies must be monitored to ensure that they do get their colostrum (maternal immunity).
Bitches that are recovering from caesarean section (unable to fed the pups yet) or that are
initially reluctant to feed the pups for other reasons can be milked of their colostrum
and this can be fed to the pups through bottle or stomach tubing.
If the bitch has no colostrum or leaks her colostrum early, plasma can be taken from the bitch and given to the puppies either orally in the milk (within the first 12-24 hours) or via
plasma transfusion (if over 24 hours).
9) Don't expose puppies to contaminated environments.
Puppies should, ideally, go from the safe whelping zones straight to their new owners.
The aim is to sell and get the pups out of the environment ASAP. They should not come into close contact with the general canine population, where kennel cough shedders
might be present (remember aerosolised virus transmission), nor should they come into contact with
another animal's food or water bowls (which could be infected) or any areas of the premises that are impossible to disinfect. Early weaning (4-5 weeks instead of 6+ weeks) is a consideration here - try to get the pups out of the environment as early as possible.
10) Wear gloves.
Whelping bitches and unvaccinated or not-fully vaccinated puppies and dogs in high risk situations
should be handled with gloves (plastic disposable drapes are also available for the extra cautious to shield dogs from possibly-contaminated clothing). New gloves should be used for every litter to avoid passing infectious organisms from one bitch (and litter) to the next. If possible, gloves should be used when handling all other dogs on the premises too (though it might not be practical in a big population).
At a bare minimum, hands should be washed thoroughly after handling each dog, prior to
handling the next.
11) Avoid in-breeding - i.e. don't breed susceptible animals.
In-breeding (e.g. breeding facilities) should be avoided to reduce the risk of genetic immune system disorders appearing and enhanced susceptibility to viral and bacterial infections.
12) Control other easily-prevented diseases that might compromise an animal's respiratory function or immune system and make it susceptible to infection.
Respiratory diseases (e.g. irritant bronchitis) and high parasite burdens (both in the lungs and intestines) compromise the defensive mechanisms of the respiratory system, reducing the ability of
the respiratory tract to clear kennel cough viruses and bacteria. Additionally, low-grade, chronic diseases (including parasitism) can cause chronic, low-grade
stress, which may suppress the immune system's response to kennel cough. Consequently, control of these other pathogens and diseases, through appropriate medications and parasite programs (routine worming etc.) is vital. Good hygiene is crucial here too: ensuring that all runs, feed bowls and water dishes are cleaned promptly of fecal and respiratory tract secretions and ensuring that excrement and secretions are not permitted to spread to other runs or kennels through gutters and run-off. Most
intestinal and respiratory parasites and infections are spread through fecal-oral routes, contaminated dishes and coughing/sneezing: less feces, clean bowls and
decent isolation means less disease transmission.
13) Avoid overcrowding of animals.
Overcrowding promotes rapid infectious disease spread from animal to animal; it
promotes stress which suppresses the immune response of susceptible animals and overcrowding makes it
difficult for facility operators to identify the sick and to find a place, sufficiently out of the way, to isolate the sick, once they have been identified. With diseases like kennel cough, overcrowding is of particular concern because a single cough
or sneeze can spread virus particles over wide distances, potentially affecting many
animals.
14) Depopulate.
Kennel cough is one of the few diseases where complete depopulation and resting of a facility (removing all animals for a period of time) may be very effective in rendering it non-infectious. It may be one of the few really effective ways to control a really
severe outbreak of kennel cough in a premises. Most kennel cough organisms are very susceptible
to most disinfectants (thorough disinfection of all of the premises will usually be enough
to kill the agents), and also susceptible to heat and drying (desiccation). Depopulating a premises, thoroughly disinfecting it and letting it rest, unpopulated, for around 2 weeks will usually be enough to remove kennel cough completely, especially in warmer, drier climates. In cold climates, kennel cough may be more resistant to the effects of heat and desiccation, so your disinfectant job will need to much more thorough.
15) Reduce stress.
The number of susceptible animals is reduced when stress is low. This is discussed
in section 10C - reducing the non-infectious, environmental and stress factors that can contribute to disease.
10b: Reducing environmental contamination with kennel cough:
In any place where kennel cough has appeared, it is important to ensure that contamination is minimized
where possible (e.g. reduce the number of infectious particles that enter a 'contaminated' area); that the virus
or bacteria is destroyed as thoroughly as possible (decontamination of the environment) and to ensure
that the infectious disease organisms do not spread from the contaminated regions to 'clean' regions of the premises and beyond. In the case of kennel cough, preventing contamination is actually
the harder of the tasks (because infectious tracheobronchitis can travel place to place via the air and even
through ducting systems), whereas decontamination is actually quite easy because
most of the viruses and bacteria are relatively easy to kill with modern disinfectants (see section 11).
1) Reduce the incidence of shedders (mildly clinical replicators and distributors of infection).
Unlike many other infectious diseases whereby infected animals can shed infectious organisms
into the environment for months to years without showing any clinical signs of infection, animals with viral forms of kennel cough do not seem to develop a prolonged non-clinical carrier state.
With the kennel cough viruses, animals will shed infectious disease particles during the period of infection,
when they have obvious clinical signs, and also for variable short-term periods afterwards (depending on the causative infectious disease agent), when the symptoms may be subtle or no longer evident.
Bordetella bronchiseptica, on the other hand, can induce a carrier state: some animals can be long term
carriers and shedders of Bordetella without showing signs of disease.
In the case of Bordetella bronchiseptica, the animal can shed infectious bacteria
in the saliva and respiratory secretions for an average of 3 months post infection, sometimes longer. In the
case of adenovirus and parainfluenza 2, the virus will tend to shed for up to 10 days after infection. Thus, in order to prevent environmental contamination with
these organisms, it is important that this period of post-clinical shedding be taken into account
and animals not reintroduced to other animals prematurely. Quarantining of infected animals
should extend out to 10-14 days beyond the resolution of clinical signs. If Bordetella
has been definitively diagnosed (e.g. on culture), then quarantining of infected
animals may have to extend to 3 months beyond the resolution of clinical signs, if you are to be thorough in preventing Bordetella contamination of the environment
and susceptible pets by non-clinical Bordetella carriers. Culturing the respiratory
tract, just prior to reintroduction of the animal, may be helpful in ensuring that
Bordetella has been cleared from the tract and that the animal is not a long-term carrier. Long-term carriers (ones that keep culturing positive) may need to be completely removed from the canine population.
See author's note next for drawbacks
on Bordetella quarantine and culture.
Authors note: many animals can carry Bordetella in their airways past the 3 month mark (some will carry the bacteria indefinitely). Quarantining animals for 3 months may, therefore, not be a truly practical solution to the problem because it is impossible to tell which animals will be clear and not clear after that time.
Even culturing (to tell which animals still carry the disease) has its drawbacks
because there is high potential for false negative results to occur on a culture
and because each culture requires that the animal goes under a general anaesthetic (which gets costly).
As mentioned in section 4e, many owners of large dog facilities just have to accept
a low grade level of Bordetella shedding in their facilities and take steps to protect
the susceptible animals from disease: vaccination being the most vital step.
Additionally, owners of large facilities must take into account the mildly-clinical animals (also discussed in section 4e). These are vaccinated or otherwise kennel-cough-resistant
animals that are infected with the disease, but only develop very mild signs, making them
difficult to recognise and isolate from susceptible animals and environments. They are different from carriers, in that carriers are clinically
normal animals (no symptoms) shedding virus or bacterial particles into the environment. These animals
(minimally clinical) do have symptoms (i.e. they do show signs of disease), it is just that these symptoms are mild and take a more skilled eye to recognise. Failure to
recognise and isolate these low-grade infected animals from other animals can result in
significant environmental contamination with infectious agents.
Staff must be trained to recognise the subtle signs of low-grade kennel cough infection
and take steps to isolate/quarantine affected animals. The staff should be on the lookout
for subtle signs: a dog slightly off food, dogs that are occasionally coughing and occasionally sneezing, dogs with a subtle watery nasal discharge etc. Daily temperature
checks may be helpful (so long as the animals are not excited or stressed by the interaction - which can artificially increase their temperatures) to identify dogs
with signs of fever, which can be a clue as to infection.
Vaccination can be used to improve animal immunity towards disease and reduce the
incidence of long-term carriers and minimally-clinical shedders. In the case of kennel cough, vaccination is not 100% in preventing transient and longer term shedding states from developing. It is thought that a lot of vaccinated animals may develop subclinical or low-grade infections with kennel cough and shed virus and/bacterial particles for a variable period of
time without owners being aware of the infection. Still, every little bit helps. It is partly for this reason (not just preventing animals from becoming clinically unwell) that ALL animals in any breeding or multi-dog facility must be fully vaccinated and kept up to date with vaccinations.
2) Isolate infected or sick animals.
Sick animals should be removed from the general population and put into a quarantine region (typically, severely affected pets will go to the vet and the vet will isolate them in a special 'iso' - isolation - ward.) This quarantine region should not be near any thoroughfares (places where animals and people frequently walk) and well out of the way. Because of the spread of kennel cough through the air
in coughs and sneezes, quarantine should ideally be off the main premises altogether
and not share any air conditioning or ducting passages with animal-populated areas.
Animals in quarantine should be handled as little as possible (though not infrequent enough
that they aren't getting proper care). When handled, the carer should wear disposable
gloves; a disposable gown and even a hair net and goggles (many respiratory-spread
pathogens can sit in your hair and within your nasal tract and mucous membranes
for a period of time). All materials used by the carer should be disposed of in bins present in the iso ward so that nothing that is potentially infectious gets brought out into the 'clean' areas. Shoes are generally washed thoroughly in disinfectant foot baths (see section 11) as the carer leaves the isolation area - this should be
enough to kill kennel cough particles.
3) Quarantine areas where sick animals have been.
Areas where sick animals have been should be quarantined from other animals until thoroughly disinfected (see section 11) and rested. Most kennel cough agents are easily killed by disinfectants and so disinfecting the affected regions and 'spelling them' (depopulating them of animals) for a few weeks is often enough to remove all traces of kennel cough pathogens.
4) Discard contaminated bedding.
Any towels or bedding that the sick animal has been on should be discarded as garbage once soiled. In the case of kennel cough, you could disinfect and salvage them
if you really need them (e.g. if the bedding is really expensive or valuable), but the best option is always to throw out potentially infectious items which
could harbour virus and bacteria particles.
5) Be mindful of run-off and air-passages.
Be careful that run-off from quarantined areas does not travel to 'clean' areas.
Be mindful of gutters, gaps under the walls of pens and gaps in the walls of pens (e.g. wire fencing), that might allow respiratory and nasal secretions from infected animals to contaminate clean areas or waterways. Be aware of the potential for kennel cough organisms
to spread via the air through air conditioning or heating ducts
and across open spaces and through wire fencing.
6) All infected rooms, pens and fomites (feeding dishes, grooming gear, benches etc.) should be disinfected thoroughly before exposing other animals
to them. Information on kennel cough disinfection is contained in section 11.
7) Avoid overcrowding of animals.
Overcrowding promotes rapid infectious disease spread from animal to animal; it
promotes stress which suppresses the immune response and overcrowding makes it
difficult for facility operators to find a place, sufficiently out of the way, to isolate the sick.
8) Consider your choice of surfaces: you want surfaces
that don't hold or protect bugs and which are easy to clean and disinfect.
It is almost impossible to keep infectious diseases and parasites out of dirt flooring and
grassy areas: such surfaces are difficult to decontaminate and they tend to pool water, which promotes the growth or survival of infectious organisms. In the case of kennel cough
control, surface choice is not as important as it is with, say, parvovirus. Even if you
can not get at the dirt or grassed area with disinfectants, kennel cough particles will usually die off
within hours to weeks if exposed to heat (especially heat over 20C), sunlight (UV light) or drying
conditions (desiccation).
I make mention of surface choice here mostly because of other, more resistant, diseases
such as parvo (which don't simply die off in the sun) and because of the relative ease
of kennel cough contamination. Sure, canine cough agents may die in the sun, but this takes time. It is far quicker and easier to rid yourself of kennel cough if you can thoroughly disinfect
your premises top to tail. For ease of disinfection (including parvo etc.) you are better to go with cement or tile flooring, which can be easily cleaned of feces, urine, vomit and respiratory secretions and readily disinfected.
Routine sanitation and cleaning is a must in all dog facilities. All surfaces (even ones without kennel cough) should be routinely disinfected and kept clean. Feces and urine must be removed daily. Routine spraying of runs with water to remove
particulate matter and dust is important (these harbour infectious organisms and bacteria) and
intermittent (weekly to 2-weekly) steam-cleaning of surfaces is useful (parvo is killed
by steam-cleaning).
Don't forget to clean cage or door bars and vertical walls where a dog might have
sneezed!
Choice of fencing/walls is important too. Smooth-textured (e.g. steel), solid, filled in walls
are easier to clean than wires or rough brickwork (which have a hugely increased surface
area for bacteria and viruses and dust to cling to). Solid, filled in walls also promote less
aerosol transmission of disease from dog to dog than open wiring does.
9) New animals should be quarantined.
As a routine part of infectious disease prevention, all new dogs to a breeding facility
or pound, shelter or boarding kennel should be quarantined away from the main dog population for at least a month. They should be fully wormed and vaccinated and monitored for disease appearance. Only when the time is up and the animal considered free from disease, should he or she be allowed into the greater population.
Note that this quarantine zone should not be an area that has had diseased animals
in it before. If it has had diseased animals previously, then it should have at least been thoroughly disinfected and spelled prior to the arrival of the new animal for quarantine. If not, the new non-diseased dog could contract disease from the quarantine area.
Quarantined animals should be treated like isolation animals, with gloves, gowns
and foot bathing (or shoe covers etc) used to prevent disease going from the
quarantine zone into the rest of the population or from the rest of the population into the quarantine zone.
In theory, households looking to introduce new animals into their already existent pet family could also employ a similar quarantine procedure. If this is not
possible or practical, new additions to the family should ideally be bought from reputable breeders or families (places with excellent standards
of pet care and hygiene) and vaccinated and wormed prior to arrival.
10) Staff should know the signs of unwellness and kennel cough infection in puppies.
Early detection of illness is key to establishing rapid isolation of the animal
and reducing the spread of diseases like canine cough. Staff should look out for lethargic, inappetent (or reduced appetite puppies) or 'loner' (puppies on their own) puppies. Puppies with any coughing, sneezing, nasal discharges or ocular discharges (watery eyes) should be immediately isolated. Recognition of puppies in poor condition or unwell condition is very important in places like pet shops that receive lots of unvaccinated puppies through their doors. These places should not take on any weak or sickly puppies to sell, as they risk contaminating their facilities and all the other healthy pups that
they get in.
11) Good record keeping.
Breeders that receive dogs from elsewhere and pet shops that receive lots of for-sale
puppies from various sources must keep good records of where these animals have come from. Good record keeping allows these facilities to recognise breeders and sellers that
are frequent offenders and who frequently sell underweight, malnourished, wormy or kennel cough-affected animals. Once identified, not buying from such places can go a big way towards preventing kennel cough and other contagions from
getting into your facilities.
12) Control rodents and insects.
Rodents and insects can potentially carry kennel cough organisms on their feet from animal to animal and place to place. Strict control of these vectors must be put into place in order to reduce the spread of kennel cough in a facility. Obviously, removal of factors which attract rodents (such as grass, grain, open dog-food packs and warm, hidden areas to breed) and flies (feces, open foodstuffs) is vital, but adequate control may need to include the use of rodent poisons and insecticides and 'fly traps'.
13) Reduce dust.
Dust holds viruses and bacteria on it, protecting them from the effects of exposure and
desiccation that would, otherwise, deactivate them. Viruses and bacteria remaining infective
within dust can be inhaled by susceptible animals, resulting in infection. Lots of
dust can holds lots of infection.
10c: Reduce the non-infectious, environmental and stress factors that can contribute to disease.
1) Reduce stress.
Stress lowers the immune system of animals, making them more susceptible to disease.
Each point below addresses a different factor in stress-management:
Ensure that all animals have adequate nutrition. Happy, well-nourished
animals of good bodyweight generally have a better immune system and are better equipped to cope with disease.
Remember to treat each animal as an individual: regularly record the weight and body condition
of each puppy or dog to ensure that the nutrition provided is adequate for him or her and
to ensure that the animal is actually getting fed. It is easy in crowded situations
for individual animals to be underfed (as an individual, they might simply need more food than is on offer) or for carers not to realise that a puppy is being bullied out of a meal. Remember
that nutritional monitoring is particularly important in animals that have high
metabolic requirements: pregnant dogs, lactating dogs, growing pups and performance
animals (e.g. working dogs, sporting dogs and obedience dogs).
Temperature and moisture control. Making sure that kennels and runs are warm and dry and free of draughts and chills
will also go a ways to keeping animals comfortable and stress-free. Temperature control
in runs is important: excessively cold and hot conditions are stressful and can facilitate disease. Constantly fluctuating temperatures are also stressful, even if the swings are not extreme: maintaining a steady-state, comfortable temperature
is ideal. According to Greene CE, temperatures
should be between 21-24 degrees-C. Remember that temperature control is particularly important in animals that have other stresses (you don't want to add temperature issues to their worries): pregnant dogs, lactating dogs, growing pups and performance animals (e.g. working dogs, sporting dogs and obedience dogs).
Sanitation. Making sure that kennels and runs are cleaned and sanitary goes a way towards reducing stress. Kennels and runs must be cleaned twice to three-times daily (or more, if possible). Animals
do not like sitting in feces and urine any more than you do. Excrement promotes the growth of other diseases and infections that the animal's immune system must then fight: these extra infections divert a portion of the animal's immune system away from fighting diseases such as kennel cough and parvo, which the animal might then contract (i.e. the animal's
immune system may have been able to defeat the kennel cough or parvo organisms, had
it not been engaged in fighting off the diseases caused by the lack of sanitation). Remember that good sanitation is particularly important in animals that have other stresses (you don't want to add sanitation issues to their worries): pregnant dogs, lactating dogs, growing pups and performance animals (e.g. working dogs, sporting dogs and obedience dogs).
Exercise and mental stimulation. Animals get stressed when they are bored and
unstimulated and have no opportunity to occupy themselves. Dogs are intelligent creatures
which need stimulation, both mentally and physically. Dogs in large dog facilities
should be walked a minimum of twice daily (ideally for 30 minutes or more at a time)
and be given room to run around in and toys or other nice dogs to play with (provided they
all get on OK). Bitches with newborn pups generally don't like to interact with other dogs
or to be taken away from their pups and so they should be offered toys and a moderate amount
of space and allowed to choose their activities for themselves.
Late-pregnant and lactating bitches. In the wild, these animals usually go off on their own (into a dark den) to give birth and to rear their litter in private (at least for the first 6 weeks). In a breeding facility, these animals should be allowed their privacy: a warm, well-bedded
dimly-lit place to give birth and rear their pups. These animals should not be placed
in close proximity (sight, smell or hearing) to other dogs and should not be forced
to socialize or leave the pups too often. This causes stress.
Avoid overcrowding. See point 5.
Be aware of dog-to-dog interactions. Some animals do not like being near other animals for many reasons: simple dislike, prior experiences, the other dog making
threatening gestures through the fence (rigid stance, growling, staring etc). Placing an animal
for long periods of time in close proximity to a dog that it fears or does not get along
with will inevitably lead to stress. Dogs may not realise (as we do) that the big dog
next door can not get at them through the fence. Thus, leaving those animals side
by side (especially in wire-fenced cages where they can clearly eye each other) will
result in one animal being in constant fear that the other will soon attack them.
Ideally, only place animals in close proximity that get along or are at least indifferent to each other.
2) Reduce dust levels:
Dust irritates the nasal and respiratory passages of the animal, resulting in irritation
and injury that can allow secondary infectious disease organisms to become established. Dust also carries infectious disease organisms: these get inhaled when the dust is inhaled. Dust may also cause symptoms similar to kennel cough (coughing, sneezing and nasal
and ocular discharges) that are impossible to differentiate from kennel cough. This can
result in unnecessary isolating and quarantining of animals because they 'look infected'.
3) Make sure that irritant disinfectant aerosols and other respiratory irritants are well aired-out prior to reintroducing an animal to a kennel or run:
Irritant vapors and aerosols chemically abrade the nasal and respiratory passages of the animal, resulting in irritation
and injury that can allow secondary infectious disease organisms to become established.
They may also cause symptoms similar to kennel cough (coughing, sneezing and nasal
and ocular discharges) that are impossible to differentiate from kennel cough. This can
result in unnecessary isolating and quarantining of animals because they 'look infected'.
4) Provide good ventilation and air circulation:
Kennel cough organisms that are enclosed in respiratory aerosols will swirl around
a room after a cough or sneeze, waiting to be breathed in by a susceptible animal.
If the room has no breeze or ventilation, then the infectious aerosols will remain in the vicinity of the canine population for longer, increasing the risk of infection
passing along. If, however, the room or space is well ventilated (has good breezes
and/or ducted ventilation systems in place), then the aerosols will be blown away from
the dog population quicker, resulting in less infectious disease transfer. Ideally, adequate ventilation of a facility should provide 12-20 air exchanges each hour.
5) Avoid overcrowding of animals.
Yes, I know I have mentioned it 3 times now. This shows how important I think it
is in the prevention of kennel cough and other diseases. Overcrowding promotes rapid infectious disease spread from animal to animal; it
promotes stress which suppresses the immune response of susceptible animals and overcrowding makes it
difficult for facility operators to find a place, sufficiently out of the way, to isolate the sick.
With diseases like kennel cough, overcrowding is of particular concern because a single cough
or sneeze can spread virus particles over wide distances, potentially affecting many
animals.

11. How to disinfect the environment following kennel cough contamination.
Regardless of whether an affected kennel cough case appears in your own home or in a larger multiple-dog environment
such as a breeding facility or veterinary clinic, it is important that correct hygiene measures are
taken to clean and disinfect the contaminated areas. Fortunately, most kennel cough agents
are really easy to kill and there are many ways (both chemical and physical) to remove
the organism from surfaces and fomites (feed bowls, water dishes) in order to prevent the disease from spreading.
Chemical agents (disinfectants) used to kill kennel cough organisms.
Initial cleaning with water.
Before a disinfectant can be used on an area, it is important to thoroughly scrub the
area with water beforehand. This is to remove gross pus, fecal, urine, vomit and soil matter from the surfaces. It is important to do this because organic matter such as feces can inhibit the effects of some disinfectants (for example QUATs)
and even deactivate them! Removing fecal and soil/dust matter will also reduce the surface area over which the kennel cough particles can hide out, thereby enhancing the ability of the disinfectant to make contact with them.
This initial cleaning process should not contain disinfectants or other soaps because some
disinfectants will react badly with or deactivate other kinds of disinfectants (the reaction can even create poisonous gasses which you might breathe in).
Quaternary ammonium compounds (QUATs).
These substances (also termed cationic disinfectants or cationic surfactants) are probably the most common disinfectant substances used by most households today. They are
readily available in most supermarkets and work well in the killing of most kennel cough organisms.
To tell if a cleaning agent contains QUATs, it is important to consult the active ingredients
label on the side of the product. There are many kinds of QUATs available for household or commercial use
and common ingredients used include dodecyl dimethyl ammonium chloride, N-alkyl dimethyl benzyl ammonium chloride and
benzalkonium chloride. Of these, benzalkonium chloride is the more common. Used
at a concentration of around 0.3%, it readily kills kennel cough organisms. Apart from
the actual name of the ingredient, what you might alternatively encounter is the term:
contains cationic surfactants. Cationic surfactants are another name for quaternary ammonium compounds:
the term is often used instead of stating an actual QUAT ingredient.
Although no disinfectant can be termed safe (they all have nasty poison warning labels on
their packets), the quaternary ammonium compounds are probably the most innocuous
of the chemicals that will be mentioned on this page. They can be used to mop over
floors, clean gutters, wipe vertical surfaces and are frequently placed in foot baths
in isolation units. A lot of the detergents used to wash clothes (e.g. fabric softeners and washing powders/liquids)
are quaternary ammonium compounds: they should be fine to remove kennel cough organisms from clothing and bedding.
The most important thing to remember, when using benzalkonium chloride or any of the QUATs, is that these disinfectants are deactivated by organic matter and other soaps and detergents. Therefore, thorough cleaning (water and scrubbing) of the kennel cough contaminated area (removing
all residues and pus etc.) before use is important.
Like many disinfectants, QUATs have the ability to cause chemical burns to skin, mouths, eyes and delicate mucous membranes and open wounds. They need to be thoroughly rinsed
from any surface and/or fomite after application so that animals are not
able to ingest them or get burned by them. QUATs (like any disinfectant chemical) should ideally only be used in well-ventilated areas or, if used in poorly ventilated areas, be used with appropriate safety apparatus (face and eye masks, possibly even breathing apparatus).
 Bleach.
Bleach.
A simple, readily available solution, bleach made up in water to a 1:30 solution (1 part bleach: 30 parts water) will kill parvo and most kennel cough viruses. The solution must be applied thoroughly to ALL contaminated surfaces
and left on for at minimum of 10 minutes to be effective.
Be aware, of course, that some surfaces and materials will not tolerate bleach (it is corrosive at high concentrations). Also be aware that bleach is not safe to breathe in (there are lots of warnings on the labels). The bleach solution should ideally only be used in well-ventilated areas or,
if used in poorly ventilated areas, with appropriate safety apparatus (face and eye masks, possibly even breathing apparatus). Once applied and given time to act, the bleach must be rinsed thoroughly, leaving no residues, and the area allowed to ventilate well before animals can be reintroduced to the area. If it is not rinsed away well, bleach can cause severe ulcers to the skin and mouths of animals that walk on or lick it.
Aldehydes.
 Aldehyde chemicals such as formaldehyde (formalin) and glutaraldehyde and other closely related substances
are high-level disinfectants which are able to kill kennel cough organisms, even at very low concentrations. Available
as liquid disinfectants or as gasses, these chemicals are often used in the sterilization
of sensitive optical equipment and equipment that is sensitive to heat and other chemicals.
Of the two forms, the liquid forms, particularly formaldehyde, are readily available and are able to be used on premises to kill kennel cough.
Aldehyde chemicals such as formaldehyde (formalin) and glutaraldehyde and other closely related substances
are high-level disinfectants which are able to kill kennel cough organisms, even at very low concentrations. Available
as liquid disinfectants or as gasses, these chemicals are often used in the sterilization
of sensitive optical equipment and equipment that is sensitive to heat and other chemicals.
Of the two forms, the liquid forms, particularly formaldehyde, are readily available and are able to be used on premises to kill kennel cough.
I would suggest getting professional advice if considering using formaldehyde or
one of its relatives to disinfect for kennel cough. Compared, say, to the quaternary ammonium
compounds and even bleach, these substances are really nasty. Effective, but nasty. Formalin releases
noxious vapors that irritate the airways and nasal passages and it is a highly
carcinogenic (cancer causing) substance. Aldehydes should ideally only be used in well-ventilated areas or, if used in poorly ventilated areas, with appropriate safety apparatus (face and eye masks, possibly even breathing apparatus). Once applied and given time to act, aldehydes must be rinsed thoroughly, leaving no residues, and the area allowed to ventilate well before animals can be reintroduced. Given the choice, I would stick with the QUATs.
Ethylene Oxide.
This is a powerful gaseous chemical which is able to kill most infectious disease
organisms. It is generally only available in hospitals to sterilize equipment, however,
it could potentially be applied to contaminated canine fomites (dog feed bowls, grooming gear)
in order to kill kennel cough virions. I would consider it to be too cost prohibitive and equipment intensive to be a real practical consideration for the average dog breeder or householder.
Besides, there are perfectly effective, more readily available, cheaper options
available for killing off kennel cough.
Other chemicals and antiseptics that may be effective against kennel cough.
Chlorhexidine is one of the antiseptic disinfectants
commonly used in veterinary hospitals to flush wounds and to prepare skin for surgery.
At normal concentrations (0.5%) chlorhexidine has the potential to kill enveloped viruses
and most bacterial types, provided that enough contact time is allowed for the substance to do the job. It probably won't kill non-enveloped viruses like adenoviruses. As far as its effectiveness as a room-cleaner goes, chlorhexidine is not deactivated by organic materials (feces, vomit etc) or soaps. It does have the potential to
stain surfaces. In reality, chlorhexidine was not really intended for room-disinfectant purposes. It is a great skin and wound antiseptic agent (the mainstay of surgeries everywhere),
but not practical for decontamination of a large premises: there are better cleaning
agents (e.g. QUATs) available for this purpose.
Non-chemical agents used to kill kennel cough.
Steam-cleaning.
Enveloped viruses such as parainfluenza 2 are not resistant to intense heat and pressure. Steam cleaning will kill this virus and even non-enveloped viruses such as parvo virus
and adenovirus and may be an option for carpets, clothing and bedding where other chemical compounds might not be appropriate. Autoclaving (whereby hospitals and vet clinics use intense pressure and heat to sterilize surgical equipment) is a good way of removing infectious organisms from steel fomites, instruments and cloth materials.
Depopulation and resting the environment.
Sunlight, heat and dry, desiccating conditions all kill kennel cough organisms. Therefore, simply removing all animals from a premises, disinfecting the premises well and leaving the premises unpopulated for 2 weeks can be a good way of removing kennel cough from a contaminated environment. In cold climates (close to
freezing), kennel cough may last for quite a few weeks and so you are either going to have to wait and rest the area longer or rely more on intensive chemical disinfection.
Remove the infected surfaces.
This is an expensive way to remove infectious disease organisms, however it does work. Routinely replacing gravel, topsoil or lawn surfaces that have become contaminated and replacing them with new, fresh, non-contaminated surfaces is an excellent way to
remove infectious disease organisms. If the difficult-to-clean infectious surfaces
(soil, lawn etc) can be replaced with a new, easy-clean surface such as concrete or tiles or
metal (in the case of runs and cages), so much the better. In the case of kennel cough, particularly
in warm climates, replacing of surfaces is probably overkill. The organisms
are easy to kill with basic disinfectants and will also deactivate in sunlight, heat and drying conditions.
Author's note: The above disinfectant points pertain to the disinfection of the primary kennel cough viruses and bacteria, not to the individual secondary bacterial
types (Staphylococcus, E coli, Pasteurella etc.) Many of the secondary bacterial
types have their own resistances, both to disinfectant chemicals and to light and heat. For example: Some Staphylococcus species are very resistant to phenols, can survive in 60-degrees temperature for half an hour and can survive in the environment for
many weeks. Some, like E. coli and Klebsiella are easily killed by routine disinfection and heat and drying. If an individual secondary organism is causing a problem in
your facilities, it is best to look up the specifics of this organism for how to control it.

12. Kennel cough summary of important points:
1) Kennel cough is a common, highly contagious disease characterised by a harsh, honking or hacking cough,
watery to pussy eye and nasal discharges and variable appearance
of fever, inappetence and sneezing. Animals are usually bright and alert and well-looking, but have a severe cough.
2) Kennel cough is caused by a number of infectious organisms, both viral and bacterial.
3) Kennel cough is exacerbated by a range of non-infectious disease factors, including
stress, immune suppression, poor air quality, high dust levels and other airway irritants.
4) Kennel cough transmission typically occurs when individual dogs are introduced into environments
with large numbers of other dogs (e.g. kennels, pounds, shelters etc.). Signs usually develop within 3-10 days of being exposed.
5) Kennel cough can become complicated by secondary bacteria, leading to severe
cases of pneumonia and sepsis especially in young or unvaccinated animals.
6) Vaccination is not 100% effective at stopping animals from contracting kennel cough
and showing some symptoms, nor is it 100% effective at preventing animals from replicating
and shedding the organisms into the local environment (ready to infect other animals).
7) Vaccination does reduce the severity of signs and the risk of severe secondary disease
complications.
8) Treatment for kennel cough involves giving the affected animal antibiotics and other supportive remedies and medications (rest, anti-inflammatories, anti-tussives, nebulisers) and isolating the animal during the infection and for a period of time afterwards.
9) It is rare for kennel cough infected animals to die from the disease. Young puppies, very old animals, animals with pre-existing lung or heart disease and immune suppressed animals
are most at risk of secondary complications that could result in severe disease and even death.
10) Animals recently recovered from kennel cough can shed infectious virus particles into
their environment for up to 10 days after infection. Animals recently recovered from Bordetella bronchiseptica kennel cough can shed infectious particles into
their environment for an average of 3 months after infection. Bordetella can convert
to a long term carrier state within animals (dogs shedding the organism, but showing no
symptoms of infection).
11) Bordetella can survive inside of white blood cells, making it difficult to kill.
Long term, recurrent kennel cough infections can result.
12) Both intranasal and injectable kennel cough vaccines are available to protect against the
disease. Both vaccine routes are effective when used on their own (intranasal vaccine routes
are perhaps more effective at protecting against kennel cough organisms than injectable routes are, but both are effective), however, best protection is achieved when both injectable and
intranasal vaccines are administered to animals together.
13) Intranasal vaccines can produce mild signs of kennel cough 2-5 days after vaccination.
14) A wide range of disinfectants and environmental conditions are able to kill kennel cough organisms.

To go from Kennel Cough page to Home Page, click here.

References and Suggested Readings:
1) Prevention of Infectious Diseases. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
2) Greene CE, Schultz RD,Immunoprophylaxis. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
3) Ford RB, Canine Infectious Tracheobronchitis. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
4) Greene CE, Environmental Factors in Infectious Disease. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
5) Lawler DF, Prevention and Management of Infection in Kennels. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
6) Greene CE, Levy JK Immunocompromised People and Shared Human and Animal Infections: Zoonoses, Sapronoses and Arthroponoses. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
7) Hoskins JD, Canine Viral Diseases. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
8) General Characteristics and Classification of Viruses. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
9) Sources and Transmission of Infectious Agents. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
10) Host-Parasite Relationships. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
11) Antimicrobial Drugs. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
12) Sterilisation and Disinfection. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
13) Streptococcus. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
14) Staphylococcus. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
15) Corynebacteria and Rhodococcus. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
16) Enterobacteriaceae. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
17) Pasteurella and Francisella. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
18) Bordetella and Moraxella. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
19) Viral Infections of Cattle. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
20) Viral Infections of Sheep and Goats. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
21) Viral Infections of Horses. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
22) Viral Infections of Dogs. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
23) Viral Infections of Cats. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
24) Immunotherapy. Wroth O, editor: MIMS IVS Annual, St Leonards, 2001, Havas MediMedia.
25) Immunotherapy. Wroth O, editor: MIMS IVS Annual, St Leonards, 2004, Havas MediMedia.
26) Information on Nobivac DHP and Nobivac KC taken from information provided by Intervet Australia Pty Limited, 2007.
27) http://en.wikipedia.org/wiki/Paramyxoviridae - Paramyxovirus.
28) Hunt R, RNA Virus Replication Strategies. Hunt R, editor: Microbiology and Immunology Online - http://pathmicro.med.sc.edu/mhunt/RNA-HO.htm, University of South Carolina, 2007.
29) Manzo U, Karunanidhi K, Paramyxovirus. Manzo U, Karunanidhi K, editors:
http://www.stanford.edu/group/virus/paramyxo/2005/index.htm, 2005.
30) Disorders of the Trachea and Bronchi. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
31) Ettinger SJ, Kantrowitz B, Brayley K, Diseases of the Trachea. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
32) Hydrocodone. In Plumb DC, Plumb's Veterinary Drug Handbook, 5th ed. USA, 2005, Blackwell Publishing.

Pet Informed is not in any way affiliated with any of the companies whose products
appear in images or information contained within this article. The images, taken by Pet Informed, are only used in order to illustrate certain points being made in the article.
Copyright April 29, 2008, www.pet-informed-veterinary-advice-online.com.
All rights reserved, protected under Australian copyright. No images or graphics on this Pet Informed website may be used without written permission of their owner, Dr. O'Meara.
Duramune, Protech, Protech Bronchi-Shield I, Protech Bronchi-Shield III and Fort Dodge are registered trademarks of Wyeth and its affiliates.
Nobivac is a registered trademark of Intervet.
Canvac is a registered trademark of CSL Limited.
Canigen, Canigen DHA2PPi and Canigen KC are registered trademarks of Virbac (Australia) Pty Ltd.
The formaldehyde compound shown is a product of Cattlekare.
White King is a registered trademark of Sara Lee.
Clavulox, Clavulox Drops, VibraVet, VibraVet Paste, Rimadyl and Zithromax are registered trademarks of Pfizer Animal Health.
Baytril is a registered trademark of Bayer Australia Ltd.
Orbax is a registered trademark of Schering-Plough Animal Health.
Linctol, Trivetrin and Tribrissen are registered trademarks of Jurox Pty Ltd.
Previcox is a registered trademark of Merial Australia Pty Ltd.
Metacam is a registered trademark of Boehringer Ingelheim Pty Ltd.
Bricanyl is a registered trademark of PMC Pharma.
Rikodeine is a registered trademark of 3M Pharmaceuticals Pty Ltd.
Augmentin is a registered trademark of GlaxoSmithKline.
Noroclav is a registered trademark of Norbrook.
Please note: the aforementioned puppy vaccination schedules, adult dog vaccination
guidelines, pregnancy vaccination guidelines and information on the new immunization schedules now being made available are general recommendations only.
The information provided is based on published information and recommendations made available from the vaccine companies themselves; relevant veterinary literature
and publications and my own experience as a practicing veterinarian.
The advice given is appropriate to the vast majority of pet owners, however, given
the large range of vaccine types and protocols now available, owners should take it upon themselves to ask their own veterinarian what vaccination schedules s/he is using so as
to be certain what to do. Owners with specific circumstances (high kennel cough virus
contamination in their environment, pregnant bitches, breeders, multiple-dog environments,
animals on immune-suppressant medicines, owners with immunosuppressant diseases or conditions
etc. etc.) should ask their vet what the safest and most effective protocol is for their situation.
Any dose rates mentioned on these pages should be confirmed by a vet. Dosing rates for common
drugs are being changed and updated all the time (e.g. as new research comes in and as drug
formulations change) and information here may not remain current for long. What's more, although we try very hard to maintain the accuracy of our information, typos and oversights do occur. Please check with your vet before dosing any pet any medication or drug.


 The damage and ulceration of the lining of the nose, trachea and bronchi results in paralysis and/or loss of the motile hairs (cilia) that normally clear bacteria from the airways. The loss of the
surface epithelial cells (which normally act as a physical barrier against infection) allows
the bacteria to attach to and gain a foothold in the exposed tissues underneath and the large volumes of inflammatory proteins and secretions within the damaged airways provides nutrition for the bacteria, allowing their populations to grow quickly. As
a result, secondary bacterial infection of the throat, trachea and nasal passages
can occur. This bacterial overgrowth results in massive numbers of white blood cells
flooding into the affected airways. The animal will often develop thickening of
the secretions within the trachea and nasal passages: these discharges may even develop a greenish or
yellowish discolouration (e.g. yellowish 'snot'). The presence of the white blood cells and bacteria within the airways can often worsen the clinical signs (e.g. the cough worsens as the bacteria and white blood cell toxins further erode the lining of the airways). Animals may find it difficult to breathe because of the thick pus plugging their airways (they will gag and hack and appear to choke
at times). These animals may be miserable and febrile (feverish) and will usually have a bad cough and sometimes a pussy nasal discharge. Sometimes these animals will be off their food and can appear very unwell. As a general rule, these animals will not usually have any increase in their respiratory rate (it should be 15-30 breaths per minute) because the disease is not yet affecting their lung function ... yet (see next section).
The damage and ulceration of the lining of the nose, trachea and bronchi results in paralysis and/or loss of the motile hairs (cilia) that normally clear bacteria from the airways. The loss of the
surface epithelial cells (which normally act as a physical barrier against infection) allows
the bacteria to attach to and gain a foothold in the exposed tissues underneath and the large volumes of inflammatory proteins and secretions within the damaged airways provides nutrition for the bacteria, allowing their populations to grow quickly. As
a result, secondary bacterial infection of the throat, trachea and nasal passages
can occur. This bacterial overgrowth results in massive numbers of white blood cells
flooding into the affected airways. The animal will often develop thickening of
the secretions within the trachea and nasal passages: these discharges may even develop a greenish or
yellowish discolouration (e.g. yellowish 'snot'). The presence of the white blood cells and bacteria within the airways can often worsen the clinical signs (e.g. the cough worsens as the bacteria and white blood cell toxins further erode the lining of the airways). Animals may find it difficult to breathe because of the thick pus plugging their airways (they will gag and hack and appear to choke
at times). These animals may be miserable and febrile (feverish) and will usually have a bad cough and sometimes a pussy nasal discharge. Sometimes these animals will be off their food and can appear very unwell. As a general rule, these animals will not usually have any increase in their respiratory rate (it should be 15-30 breaths per minute) because the disease is not yet affecting their lung function ... yet (see next section). 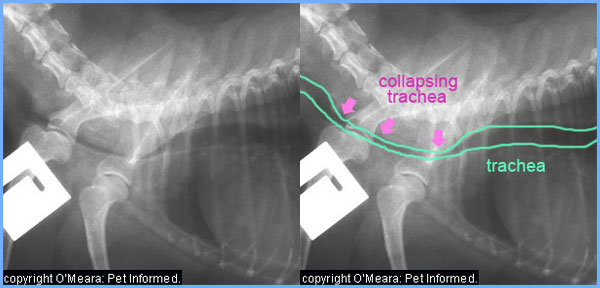
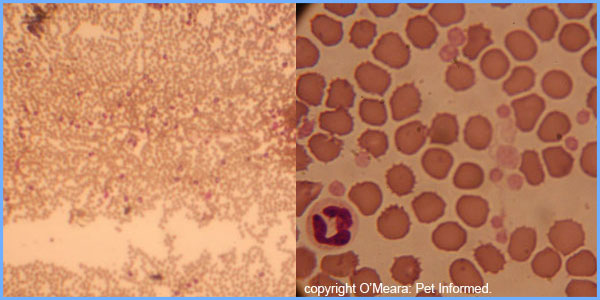
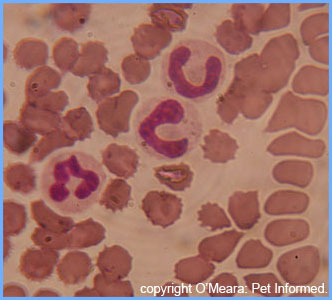
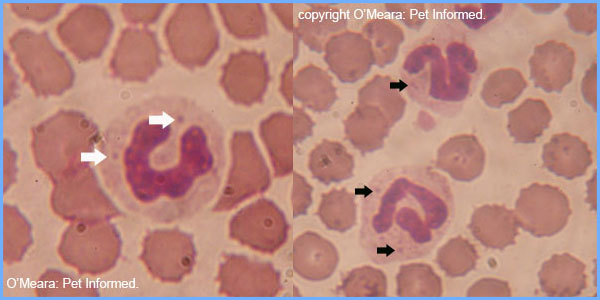

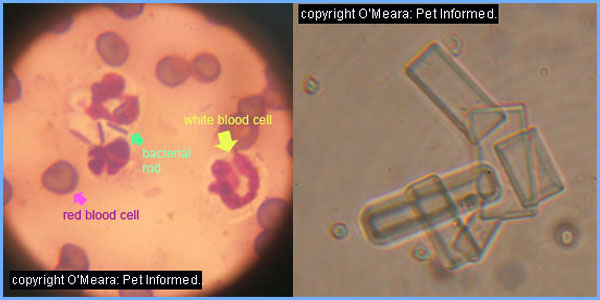
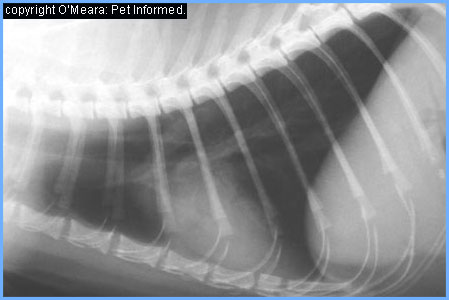
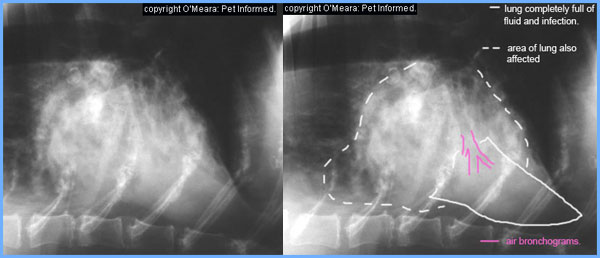
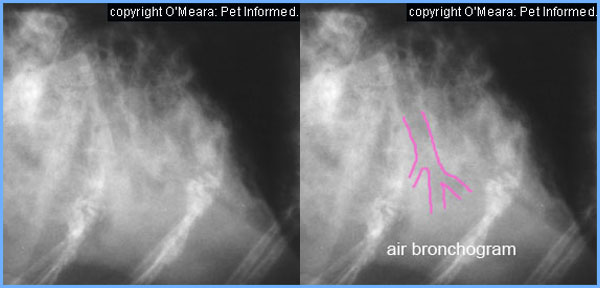
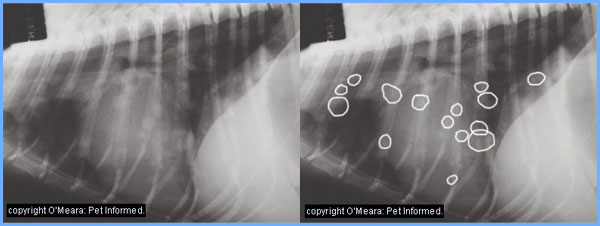
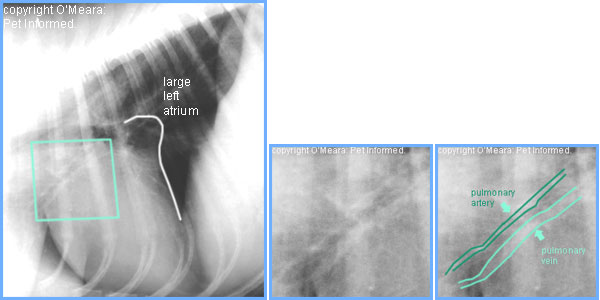
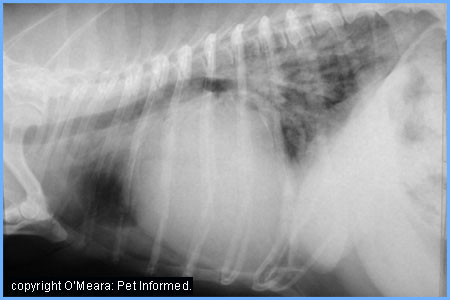
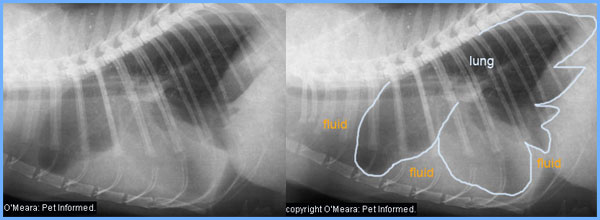
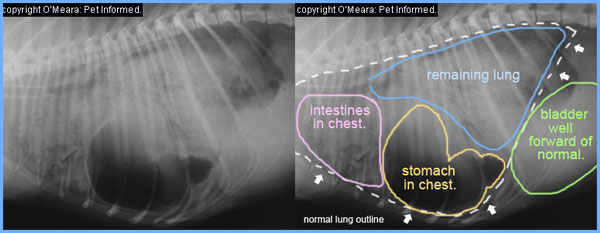
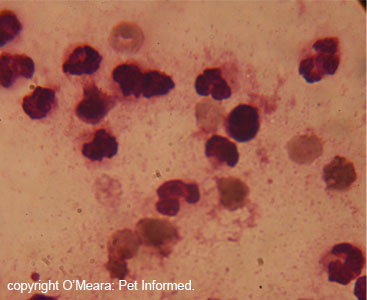
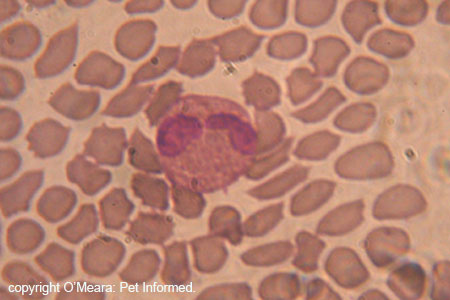

 Trimethoprim and sulfonamide are two individual antibiotic drugs that have been found to have
synergistic properties (enhanced bacterial killing properties) when they are used together. When used on their own, these drugs are bacteriostatic (they inhibit the
growth of bacteria, but don't kill them), but when used in combination, these drugs are
bacteriocidal (they kill the bacteria). As a result, most products containing trimethoprim or
sulfonamide include both drugs in the one capsule or tablet. The trimethoprim/sulfonamide combination drugs are highly effective at killing most of the bacterial types that commonly complicate kennel cough infections, including: Pasteurella, Streptococcus, Staphylococcus, E. coli, Klebsiella, Proteus and Bordetella. They have poor action against Pseudomonas. The trimethoprim-sulfa drugs are particularly useful because they are able to access many tissues (including the brain) that clavulanic acid/amoxycillin combinations can not reach.
Trimethoprim and sulfonamide are two individual antibiotic drugs that have been found to have
synergistic properties (enhanced bacterial killing properties) when they are used together. When used on their own, these drugs are bacteriostatic (they inhibit the
growth of bacteria, but don't kill them), but when used in combination, these drugs are
bacteriocidal (they kill the bacteria). As a result, most products containing trimethoprim or
sulfonamide include both drugs in the one capsule or tablet. The trimethoprim/sulfonamide combination drugs are highly effective at killing most of the bacterial types that commonly complicate kennel cough infections, including: Pasteurella, Streptococcus, Staphylococcus, E. coli, Klebsiella, Proteus and Bordetella. They have poor action against Pseudomonas. The trimethoprim-sulfa drugs are particularly useful because they are able to access many tissues (including the brain) that clavulanic acid/amoxycillin combinations can not reach. 



 Bleach.
Bleach. Aldehyde chemicals such as formaldehyde (formalin) and glutaraldehyde and other closely related substances
are high-level disinfectants which are able to kill kennel cough organisms, even at very low concentrations. Available
as liquid disinfectants or as gasses, these chemicals are often used in the sterilization
of sensitive optical equipment and equipment that is sensitive to heat and other chemicals.
Of the two forms, the liquid forms, particularly formaldehyde, are readily available and are able to be used on premises to kill kennel cough.
Aldehyde chemicals such as formaldehyde (formalin) and glutaraldehyde and other closely related substances
are high-level disinfectants which are able to kill kennel cough organisms, even at very low concentrations. Available
as liquid disinfectants or as gasses, these chemicals are often used in the sterilization
of sensitive optical equipment and equipment that is sensitive to heat and other chemicals.
Of the two forms, the liquid forms, particularly formaldehyde, are readily available and are able to be used on premises to kill kennel cough.